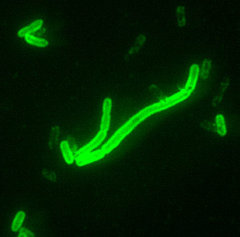
To the Editor: Plague is one of the oldest identifiable diseases. Modern public health measures and effective antimicrobial treatments have led to a decrease in plague cases worldwide. However, plague remains endemic in many natural foci. Since the early 1990s, the World Health Organization (WHO) has reported a steadily increasing trend in human plague cases, which has resulted in the recognition of plague as a reemerging disease (1). The emergence of antimicrobial drug-resistant along with an increasing number of strains of Yersinia pestis, plague cases, remind us that plague still poses a serious public health threat (2,3). In China, human cases of plague have been reported to WHO nearly every year from 1989 to 2003; these account for 9.5% of cases and 15.5% of deaths from this disease in Asia (1). Human cases of plague in China are usually caused by contact with plague-infected rodents. Here, we report the results of a serologic survey by using 3 methods (passive hemagglutination assay, Western blot, and protein microarray analysis) in marmot hunters in Qinghai Province, China.
One hundred twenty serum samples were collected in 2 villages in Huangyuan County, Qinghai Province, from marmot hunters (63 samples) and their family members (57 samples); none had a history of fever in the past 2 years. One hundred nineteen serum samples were collected from persons with no history of marmot hunting in 2 nearby counties in Qinghai Province in which plague was not endemic. Thirty serum samples were collected from persons in Beijing and used as negative controls.
All serum samples were initially screened with a passive hemagglutination assay to detect immunoglobulin (Ig) G antibody against F1 antigen of Y. pestis, by using a standard protocol (4). We then used an F1 antigen-based Western blot to analyze all serum samples. The protein microarray analysis was performed with 149 purified recombinant proteins of Y. pestis (5).
The results of the serologic survey are summarized in the Table. The passive hemagglutination assay showed 17 positive samples in the marmot hunter population. None of the control serum samples were positive for F1 antigen in this assay. Western blot identified 9 additional positive samples in the marmot hunter population, resulting in a seropositivity rate of 21.7% (26/120). We also found positive samples in 4 (3.4%) of 119 serum samples by using Western blot in persons from areas in which plague was not endemic. Identical results were also obtained by using protein microarray analysis, which validated the results of Western blot.
Previous studies have shown that plague antibodies were more prevalent in males in the exposed population, and differences in the age, sex, or ethnic group of plague patients are the result of variations in exposure to the pathogen, not intrinsic factors (6,7). Our study showed that in the marmot hunter population, the plague seropositivity rate was significantly higher in males (36.8%, 25/68) than in females (2.0%, 1/52, p<0.01). Among the marmot hunter population, 63 (92.6%) of 68 males were hunters. Plague antibodies were also more prevalent in marmot hunters (39.7%, 25/63) than in their family members (1.8%, 1/57, p<0.01).
This is the first serologic survey of plague in the marmot hunter population. The plague seropositivity rate of 21.7% (26/120) in hunters and their families is much higher than the 3.4% (4/119) in the population from regions in which plague was not endemic (p<0.01). Seroprevalence in marmot hunters was even higher (39.7%), which suggests that marmot hunting is a risk factor for plague infection.
The marmot (Marmota himalayana) is the main host of Y. pestis in Qinghai Province. Plague-infected marmots are more easily captured by hunters. When persons hunt and butcher marmots without any effective protection, Y. pestis can be transmitted through tiny wounds in the skin, by bites of infected fleas, or by the respiratory route. Asymptomatic plague infection in marmot hunters might be explained by prophylactic use of antimicrobial drugs. Most hunters usually take sulfamethoxazole or tetracycline as a prophylactic measure. Even if the hunters were infected with Y. pestis, they would likely not develop symptomatic plague. However, if the antimicrobial drugs are not effective or hunters do not use prophylaxis, symptomatic reported human cases of plague in infections will occur. Most Qinghai Province were caused by hunting or butchering marmots, as shown by a recent outbreak of plague in October 2004 in Qinghai, in which 19 cases were reported and 8 persons died (M. Li et al., unpub, data).
Acknowledgments
We thank Jin Wang, Junxing Yang, Dongsheng Zhou, Zongmin Du, Zhaobiao Guo, and Junhui Zhai for technical assistance.
This work was supported by the National Natural Science Foundation of China (30430620).
Min Li, * (1), Yajun Song, ([dagger]) (1) Bei Li, ([dagger]) Zujun Wang, * Ronghai Yang, * Liangxiao Jiang, ([dagger]) and Ruifu Yang ([dagger])
* Qinghai Institute for Endemic Diseases Prevention and Control, Xining, People's Republic of China; and ([dagger]) Beijing Institute of Microbiology and Epidemiology, Beijing, People's Republic of China
(1) These authors contributed equally to this study.
References
(1.) World Health Organization. Human plague in 2002 and 2003. Wkly Epidemiol Rec. 2004;79:301-6.
(2.) Galimand M, Guiyoule A, Gerbaud G, Rasoamanana B, Chanteau S, Camiel E, et al. Multidrug resistance in Yersinia pestis mediated by a transferable plasmid. N Engl J Med. 1997;337:677-80. (3.) Guiyoule A, Gerbaud G, Buchrieser C, Galimand M, Rahalison L, Chanteau S, et al. Transferable plasmid-mediated resistance to streptomycin in a clinical isolate of Yersinia pestis. Emerg Infect Dis. 2001; 7:43-8.
(4.) Cavanaugh DC, Thorpe BD, Bushman JB, Nicholes PS, Rust JH Jr. Detection of an enzootic plague focus by serological methods. Bull World Health Organ. 1965;32:197~03.
(5.) Li B, Jiang L, Song Q, Yang J, Chen Z, Guo Z, et al. Protein microarray for profiling antibody responses to Yesinia pestis live vaccine. Infect Immun. 2005:73:3734-9.
(6.) Chanteau S, Ratsitorahina M, Rahalison L, Rasoamanana B, Chan F, Boisier P, et al. Current epidemiology of human plague in Madagascar. Microbes Infect. 2000;2: 25-31.
Min Li, *(1) Yajun Song, ([dagger]) (1) Bei Li, ([dagger]) Zuyun Wang, * Ronghai Yang, * Lingxiao Jiang, ([dagger]) and Ruifu Yang ([dagger])
(7.) Boisier P, Rahalison L, Rasolomaharo M, Ratsitorahina M, Mahafaly M, Razafimahefa M, et al. Epidemiologic features of four successive annual outbreaks of bubonic plague in Mahajanga, Madagascar. Emerg Infect Dis. 2002;8:311-6.
Address for correspondence: Ruifu Yang, State Key Laboratory of Pathogens and Biosecurity, Laboratory of Analytical Microbiology, National Center for Biomedical Analysis, Beijing Institute of Microbiology and Epidemiology, Beijing 100071, People's Republic of China; fax: 86-10-8382-0748; email: yangrf@nic.bmi.ac.cn
COPYRIGHT 2005 U.S. National Center for Infectious Diseases
COPYRIGHT 2005 Gale Group