Turturro MA, Paris PM, Larkin GL. Tramadol versus hydrocodone-acetaminophen in acute musculoskeletal pain: a randomized, double-blind clinical trial. Ann Emerg Med 1998; 32:139-43.
Clinical question Is tramadol (Ultram) equivalent to a hydrocodone-acetaminophen combination in the treatment of acute musculoskeletal pain?
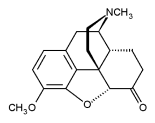
Background Tramadol is a centrally acting oral analgesic that has both mild opioid activity and monoamine reuptake inhibition. Indicated primarily for the treatment of chronic pain, it has been marketed extensively to providers who manage acute pain, because it has a low potential for abuse and no antiprostaglandin side effects. While it has been studied in comparison with other analgesics for postoperative pain, there have been no studies looking at comparable efficacy for acute outpatient pain management.
Population studied The authors studied a convenience sample of 68 adult patients, aged 18 to 70 years, presenting to the emergency department (ED) with acute musculoskeletal pain secondary to trauma. Exclusion criteria included having taken an analgesic within 4 hours of arrival to the ED, pregnancy, lactation, acute intoxication, suspected substance abuse, and a history of sensitivity to tramadol hydrochloride or either component of hydrocodone with acetaminophen. Patients taking monoamine oxidase inhibitors, carbamazepine, quinidine, tricyclic compounds, or selective serotonin reuptake inhibitors were excluded because of potential drug interactions or risk of seizures. Patients with back pain, because of the complexity of both the pain and the therapy, and patients who the examining provider felt required parenteral analgesia, were also excluded. Because of the small sample size and the evaluation of acute pain syndromes exclusively of the musculoskeletal type, relevance to the usual outpatient practice of family physicians is questionable.
Study design and validity This is a randomized, prospective, double-blind, nonplacebo-controlled study comparing the analgesic effect of tramadol hydrochloride (100 mg) to hydrocodone (5 mg) with acetaminophen (500 mg) in acute musculoskeletal pain secondary to trauma. No placebo control group was used because of ethical concerns about withholding analgesics from patients with acute pain. The capsules given to each group were identical in appearance. Pain was evaluated at baseline and at 30, 60, 90, 120, and 180 minutes, using a 100-mm visual analog pain scale (VAS). To reduce carryover bias, patients were not allowed to view previously completed scales when completing a new one. A power analysis showed that the number of patients enrolled was adequate to ensure a 90% probability that a VAS score difference of 30% was not because of random chance. All comparisons between groups used intention-to-treat analysis correctly. All other statistical tests were appropriate. The dropout rate was less than 10% for each group.
Outcomes measured The primary outcome measured was the interval level of pain using the VAS. Side effects were also elicited through open-ended questioning at the end of each subject's study period.
Results Sixty-eight subjects were enrolled in the study. Six patients, 3 from each group, dropped out because of insufficient analgesia (P = ns). The discharge diagnoses were similar between groups, and included 19 distal extremity fractures, 26 sprains or strains, and 21 contusions. Mean pain scores were similar at baseline and improved in both groups throughout the study interval. Mean pain scores in the hydrocodone-acetaminophen group were significantly lower than the tramadol group at 30 minutes (51 vs 63, P = .03), and the difference became more pronounced with each successive interval (180 minutes: 23 vs 51, P [is less than] .01). Six patients in the tramadol group and 4 patients in the hydrocodone-acetaminophen group exhibited side effects, with nausea or vomiting, drowsiness or dizziness, and anxiety reported.
Recommendations for clinical practice Compared with hydrocodone-acetaminophen, tramadol is an inferior acute pain analgesic for the treatment of acute musculoskeletal pain due to trauma. Tramadol's manufacturer has reported a significant side-effect profile, with almost 25% of patients reporting dizziness, nausea, and constipation, and nearly 20% reporting headache or somnolence. Given the significant cost differential between tramadol and hydrocodone-acetaminophen and taking into account tramadol's side-effect profile, unless there is some overriding reason to use tramadol, it should be considered a second-line agent in this setting. Studies comparing tramadol with other less expensive analgesics for both acute and chronic pain in the primary care setting are needed.
COPYRIGHT 1998 Dowden Health Media, Inc.
COPYRIGHT 2004 Gale Group