SAN FRANCISCO -- Patients receiving bone densitometry should be counseled about their T and the z scores, Steven T. Harris, M.D., advised at a meeting on osteoporosis sponsored by the University of California, San Francisco.
The T score compares the patient's bone mineral density with the mean peak bone density of a 30-year-old person of the same sex and is expressed as a number of standard deviations above or below the young person's density, said Dr. Harris of the university.
The z score compares the patient's bone mineral density with mean peak density for someone the same age, and helps give patients some perspective. "In my consultative practice over the years, I've seen many, many, many patients who have been terrified by being told that they have osteoporosis at age 78 by comparing them to that 30-year-old, and yet who feel reassured when you show them where they are relative to their peers," he said.
Sharing both score types helps give patients a more accurate picture of their bone health. A 55-year-old woman with a z score of -2 has bone density around the lower limits of normal for her age, but her T score would be -3.2 in comparison with a young adult. That patient can be reassured that she's similar to her peers, but should be persuaded that "there is an issue here that needs to be addressed," he said.
That said, the patient with a T score above -2.5 (the cutoff for osteoporosis) can still have a clinical diagnosis of osteoporosis if other factors are present such as atraumatic vertebral fractures.
Getting a z score can be especially motivating because those patients who are abnormal, compared with their peers, need the greatest attention to possible secondary causes of low bone density. "If you see an abnormal z score, it makes you worry that much more about something very unusual going on in that particular patient," Dr. Harris said.
Patients should also be warned that first bone density measurements give a snapshot of the skeleton's current state. But a low T score does not identify the cause of the low bone density, and the patient should not be labeled osteoporosis automatically, he added. Density reports can have a fairly wide margin of error on first-time measurements. In addition, bone density measurements often vary by a few percentage points when done by different machines. Whenever possible, follow-up scans should be performed with the same machine, he advised.
Vitamin D deficiency leading to reduced osteomalacia can produce a low T score that can improve dramatically once the vitamin deficiency is corrected. Celiac disease with malabsorption can lead to a low T score.
Individual T scores for L1-L4 on spinal densitometry are usually aggregated for diagnostic purposes instead of using the individual results for vertebral bodies. The best and worst scores for individual vertebrae should be within one standard deviation of each other. If not, one should suspect an imaging artifact. In these cases, usually the "best" T score is spurious, Dr. Harris said.
It's important to not just read the densitometry report but to look at the scan, he added. A spine with scoliosis, for example, will have changes in facet joints that make the accuracy of densitometry problematic.
Whiteness seen on the L3 and L4 sections of a spinal scan may be due to facet joint sclerosis, skewing density readings. The aggregation of L1-L4 measurements in one such patient produced a T score of-1.7, suggestive of osteopenia. Excluding the L3-L4 measurements, however, the T score was -2.9, in the range of osteoporosis, he said.
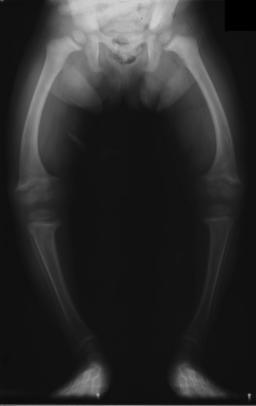
On hip scans, check to make sure the hip was imaged in the correct position, with the femoral shaft straight up and down and with sufficient internal rotation on the leg so that little or none of the lesser trochanter is visible.
BY SHERRY BOSCHERT
San Francisco Bureau
COPYRIGHT 2005 International Medical News Group
COPYRIGHT 2005 Gale Group