This protocol is intended to assist pathologists in providing clinically useful and relevant information as a result of the examination of surgical specimens. Use of this protocol is intended to be entirely voluntary. If equally valid protocols or similar documents are applicable, the pathologist is, of course, free to follow those authorities. Indeed, the ultimate judgment regarding the propriety of any specific procedure must be made by a specific patient or specimen.
It should be understood that adherence to this protocol will not guarantee a successful result. Nevertheless, pathologists are urged to familiarize themselves with this document. Should a physician choose to deviate from the protocol owing to the circumstances of a particular patient or specimen, the physician is advised to make a contemporaneous written notation of the reason for the procedure followed.
EXPLANATORY NOTES
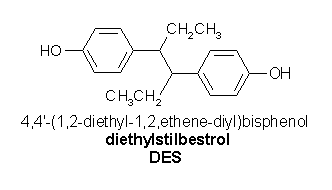
A: Prenatal Diethylstilbestrol Exposure.-Prenatal exposure to diethylstilbestrol or related synthetic drugs was relatively common in the United States and other countries until 1971, when its relation to clear cell adenocarcinomas of the vagina and cervix led to proscription of these drugs by the Food and Drug Administration. A history of this type of prenatal drug exposure should alert the pathologist to the possible presence of those tumors and associated lesions.l-3
B: Prior Tumors and Operations.-A history of dysplasia, carcinoma in situ, or invasive carcinoma of the cervix, as well as knowledge of its microscopic features may be essential in the determination of whether a subsequent vaginal tumor is a recurrent or new tumor. Also, a history of a carcinoma even higher in the female genital tract may influence the interpretation of a neoplasm that is detected in a specimen of the vagina. Prior pathology slides and reports should be obtained and reviewed if a review is deemed essential by the clinician or pathologist for optimal pathologic evaluation of the present specimen.
C: Clinical Findings and Diethylstilbestrol Exposure.-Naked-eye examination, colposcopy and iodine staining of the cervix and vagina may disclose a variety of changes highly suspicious of prenatal diethylstilbestrol exposure, such as cervical hypoplasia, pseudopolyp, coxcomb deformity, and vaginal adenosis or ridge, any of which should alert the pathologist to examine carefully for diethylstilbestrol changes.
D: Bethesda Classification System of Cervical/Vaginal Cytology.-For consistency in reporting, the cytologic classification proposed in the Bethesda System is recommended.4 This protocol does not preclude the use of other systems of classification; the Papanicolaou class designation system, however, is not recommended.
G: Other Prognostic Factors.-The architectural pattern of clear cell adenocarcinoma may have prognostic significance. Too few DNA ploidy studies and molecular genetic studies have been done to establish their prognostic value in cases of vaginal cancer.
H: Other Lesions.-Squamous dysplasia or carcinoma in situ, adenocarcinoma in situ, or atypical adenosis, particularly if such changes are at the resection margin, may increase the frequency of recurrent tumor.
I: Staining of Mucosal Surface.-Schiller's and Lugol's solutions stain glyco*enated epithelium brown. Therefore, they stain glycogenated squamous epithelium and wellglycogenated tumors. The stains are useful in identifying sites of nonstaining vaginal adenosis or immature squamous metaplasia of adenosis in patients exposed to diethylstilbestrol that may not be detectable before staining.
K: Cervical Abnormalities.-Ectropion (erosion, eversion) of the cervix, which is characterized by the appearance of glandular (columnar) epithelium outside the external os of the cervix, is seen in approximately 90% of women exposed to diethylstilbestrol in utero (but is often seen in nonexposed women as well). Approximately one third of patients exposed to diethystilbestrol have one or more gross structural abnormalities of the cervix (note C).
L: Fallopian Tubes.-The fallopian tubes are abnormal in some women exposed to diethylstilbestrol in the form of hypoplasia or defects demonstrated on hysterosalpingographic examination.3
Contributors: the College of American Pathologists Cancer Committee; Arthur L. Herbst, MD; and Robert J. Kurman, MD.
References
1. Herbst AL, Ulfelder H, Poskanzer DC. Adenocarcinoma of the vagina: association of maternal stilbestrol therapy with tumor appearance in young women. N Engl J Med. 1971;284:878-881.
2. Herbst AL, Bern H. Developmental Effects of DES Pregnancy. New York, NY: Thieme-Stratton, Inc; 1981:chap 3, 4, 6, 7. 3. Kaufman RH, Noller K, Adam E, et al. Upper genital tract abnormalities and pregnancy outcome in diethylstilbestrol-exposure progeny. Am J Obstet Gynecol. 1984;148:973-984.
4. Kurman RI, Solomon D. The Bethesda System for Reporting Cervical/Vaginal Cytologic Diagnoses: Definitions, Criteria, and Explanatory Notes for Terminology and Specimen Adequacy New York, NY: Springer-Verlag; 1994.
5. Scully RE, Bonfiglio TA, Kurman RJ, Silverberg SG, Wilkinson WJ. Histological typing of female genital tract tumours. In: World Health Organization: International Histological Classification of Tumours. New York, NY: Springer-Verlag; 1994.
6. Pettersson F. International Federation of Gynecology and Obstetrics Report. Stockholm, Sweden: International Federation of Gynecology and Obstetrics; 1988.
7. Fleming ID, Cooper JS, Henson DE, et al, eds. AICC Manual for Staging of Cancer. 5th ed. Philadelphia, Pa: Lippincott Raven; 1997.
Bibliography
Kurman RJ, Norris HJ, Wilkinson E. Tumors of the Cervix, Vagina, and Vulva. Washington, DC: Armed Forces Institute of Pathology; 1992. Atlas of Tumor Pathology; 3rd series, fascicle 4.
Kurman RJ. Blaustein's Pathology of the Female Genital Tract 4th ed. New York, NY: Springer-Verlag; 1994.
Robert E. Scully, MD, for the Members of the Cancer Committee, College of American Pathologists
Accepted for publication August 26, 1998. From the Department of Pathology, Massachusetts General Hospital, Boston.
Copyright College of American Pathologists Jan 1999
Provided by ProQuest Information and Learning Company. All rights Reserved