The term "community-acquired pneumonia" (CAP) refers to a pneumonia in a previously healthy person who acquired the infection outside a hospital. CAP is one of the most common serious infections in children, with an incidence of 34 to 40 cases per 1,000 children in Europe and North America. (1-3) Although death from CAP is rare in industrialized countries, lower respiratory tract infection is one of the leading causes of childhood mortality in developing countries. (4,5)
Etiology
Determining the cause of pneumonia in a child is often difficult, but the patient's age can help narrow the list of likely etiologies. Table 1 (6-9) lists common and less common causes of CAP by age group.
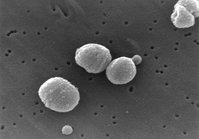
Group B streptococcus and gram-negative enteric bacteria are the most common pathogens in neonates (i.e., birth to 20 days) and are obtained via vertical transmission from the mother during birth. Anaerobic organisms may be acquired from chorioamnionitis. Pneumonia in infants aged three weeks to three months is most often bacterial; Streptococcus pneumoniae is the most common pathogen.
In infants older than four months and in preschool-aged children, viruses are the most frequent cause of CAP; respiratory syncytial virus (RSV) is the most common. Viral pneumonia occurs more often in the fall and winter than in the spring and summer. Bacterial infections can occur at any time of the year in preschool- and school-aged children and in adolescents.
S. pneumoniae is the most common bacterial cause of CAP after the neonatal period. Less common bacterial etiologies include Haemophilus influenzae type B, Moraxella catarrhalis, and Staphylococcus aureus. Mycoplasma pneumoniae and Chlamydia pneumoniae frequently are associated with CAP in pre-school-aged children and are common causes of CAP in older children and adolescents. (10,11) Pertussis should be considered in all children with CAP, especially if immunizations are not current. Mycobacterium tuberculosis also may cause CAP in children at risk for exposure. Coinfection with two or more microbial agents is more common than previously thought, with a rate of up to 41 percent in hospitalized patients. (6)
Clinical Evaluation
The strongest predictors of pneumonia in children are fever, cyanosis, and more than one of the following signs of respiratory distress: tachypnea, cough, nasal flaring, retractions, rales, and decreased breath sounds. (5,12,13)
Pneumonia should be suspected if tachypnea occurs in a patient younger than two years with a temperature higher than 38[degrees]C (100.4[degrees]F). Measurement of tachypnea requires a full one-minute count while the child is quiet. The World Health Organization's age-specific criteria for tachypnea are the most widely used: a respiratory rate of more than 50 breaths per minute in infants two to 12 months of age; more than 40 breaths per minute in children one to five years of age; and more than 30 breaths per minute in children older than five years. (14)
Children without fever or symptoms of respiratory distress are unlikely to have pneumonia. (1,15)
Key points of the clinical assessment are given in Table 2. (9) The patient history, taken at the time of diagnosis, should include the child's age, immunization status, hospitalizations, day care attendance, and recent exposures, travel, and antibiotic use.
The physician should review the child's history to identify any underlying cardiac or pulmonary diseases, immune deficiencies, or neuromuscular disorders. Inquires should be made about possible foreign object aspiration or ingestion of toxic substances. Findings not related to the respiratory tract, such as lethargy, poor feeding, vomiting, diarrhea, abdominal pain, irritability, and signs of dehydration, also should be noted.
The physical examination begins with an overall assessment of the child's well-being and identification of obvious signs of hypoxia and dehydration. The child (especially a younger child) is checked for "toxic appearance," tachypnea, elevated temperature, retractions, grunting, and use of accessory muscles. The upper respiratory tract should be examined for evidence of otitis media, rhinorrhea, nasal polyposis, and pharyngitis. Physical signs such as heart murmurs or nail clubbing may suggest underlying cardiac or pulmonary disease.
Older children and adolescents are more likely to have findings such as rales, dullness to percussion, bronchial breath sounds, tactile fremitus, and a pleural rub. (7) Care-ful auscultation with an appropriate-sized stethoscope may reveal localized rales and wheezing in younger chil-dren. Children with dehydration may have no abnormal auscultatory findings.
Diagnostic Testing
In most children with CAP, identification of the causative organism is not critical. (16) Patients with severe symptoms, those who are hospitalized, and those who have a complicated clinical course should undergo diagnostic testing to determine the etiology. The cause also should be determined if there appears to be a community outbreak.
Older children and adolescents may be able to produce sputum for Gram stain and culture. Adequate specimens contain more than 25 leukocytes and fewer than 25 squamous epithelial cells per low-power field. (7)
Rapid antigen tests are available for RSV, parain-fluenza 1, 2, and 3, influenza A and B, and adenovirus. These assays, which are performed on specimens collected from the nasopharynx, can help determine the etiology of viral pneumonia. (1,15,17) Nasopharyngeal specimens for bacterial culture or antigen assays are less useful, because bacteria commonly colonize on the nasopharynx. (1,15,17) Antigen and antibody assays for pneumococcal infection are not sensitive enough to be helpful in diagnosing S. pneumoniae infection. In the future, detection of pneumococcal immune complexes may offer a rapid etiologic diagnosis in children older than two years. (18)
Serologic testing for IgM or an increase in IgG titers may be performed for Mycoplasma and Chlamydia species. However, serologic tests often provide only a retrospective diagnosis and are more useful in establishing the causative agent during an outbreak than in treating individual children. (19) Cultures for Mycoplasma and Chlamydia are not routinely recommended. Polymerase chain reaction testing is not readily accessible, and positive results do not necessarily imply causality. (16)
The complete blood count with differential, C-reactive protein level, and erythrocyte sedimentation rate do not differentiate bacterial from viral infection and should not be measured routinely. (1,20) After the neonatal period, the incidence of bacteremia in children is so low that collection of blood for cultures can be individualized to patients who appear more ill. (6)
Chest radiographs do not differentiate causative agents of CAP as well as was previously thought. (1,21) Lobar consolidation classically has been associated with pneumococcal infections, and interstitial infiltrates have been associated with viral infections. However, both lobar consolidation and interstitial infiltrates have been identified in all types of infections--viral alone, bacterial alone, and viral-bacterial. (22) Chest radiographs should not be obtained routinely in children with mild, uncomplicated lower respiratory tract infection. (1,13) Indications for chest radiographs include ambiguous clinical findings, prolonged pneumonia, pneumonia that is unresponsive to antibiotic therapy, and the possibility of complications such as pleural effusions. (13)
Oxygen saturation should be assessed by pulse oximetry in children with respiratory distress, significant tachypnea, or pallor. (15)
Treatment
Treatment decisions are based on the child's age and clinical and epidemiologic factors. (1,8) Antibiotic therapy should be initiated promptly in children who are thought to have bacterial CAP. Because definitive information about the causative organism is usually unknown, the choice of antibiotic is empiric. (16) Table 3 lists the recommended outpatient and inpatient antibiotic therapies for different age groups, based on evidence-based guidelines from the University of Cincinnati Children's Hospital, the Alberta Medical Association, and the British Thoracic Society. (1,8,13,15,23)
INPATIENTS
Table 4 lists factors to consider in deciding whether inpatient management is necessary. (1,15) Hospitalization is required for all infants from birth to 20 days of age, infants three weeks to three months of age with fever, and all children who appear toxic. Hospital admission criteria for children four months to five years of age include hypoxemia or a respiratory rate of more than 70 breaths per minute. Other indicators for admission include difficulty breathing, intermittent apnea, grunting, poor feeding, and inadequate observation or supervision by family. (1) Admission criteria for older children include hypoxemia, cyanosis, a respiratory rate of more than 50 breaths per minute, difficulty breathing, and inadequate observation or supervision by family. (1)
NEONATES
Infants younger than three weeks with respiratory distress always should be admitted to a hospital, and a diagnosis of bacterial pneumonia should be assumed until proved otherwise. Cultures of blood, urine, and cerebrospinal fluid should be obtained, and treatment with ampicillin and gentamicin, with or without cefotaxime (Claforan), should be started as soon as possible. (7,8,23)
INFANTS
Infants three weeks to three months of age who are suspected of having bacterial pneumonia require immediate attention, particularly if they are febrile, tachypneic, or appear toxic. (7) These patients are best treated in a hospital. Initial therapy consists of cefuroxime (Ceftin) or cefotaxime. (15) Blood, urine, and cerebrospinal fluid cultures; a complete blood count with differential; and a chest radiograph should be obtained. (7,8) Once stabilized, infants may be changed to an oral antibiotic for 10 days.
Chlamydia trachomatis infection should be suspected in infants who are afebrile or nontoxic and have a dry cough. (7,8) These patients often have a peripheral eosinophilic pleocytosis. (7) In such cases, treatment guidelines recommend outpatient treatment with an oral macrolide and close follow-up. (8) If the physician decides to treat the infant as an inpatient, intravenous erythromycin is the drug of choice. (8)
PRESCHOOL-AGED CHILDREN
Viruses cause most cases of pneumonia in preschool-aged children (i.e., four months to five years of age). (1,9,16,24) Although most physicians start antibiotic therapy, guidelines allow for withholding treatment if a viral etiology is suspected and close follow-up can be ensured. (1,9,13,15,16,24) These children usually have associated symptoms of viral infection, such as pharyngitis, rhinorrhea, and diarrhea (Table 5). (1)
Pneumococcal infection is the most common cause of bacterial pneumonia in this age group. (7,24) The onset of pneumococcal pneumonia is usually abrupt, with none of the prodromal symptoms associated with viral ill-nesses. A child suspected of having pneumococcal pneumonia who is not hypoxic, in distress, or unstable can be treated empirically with high-dosage amoxicillin. (8,9,13,24) The physician may initiate therapy with a single dose of ceftriaxone (Rocephin). (13) Alternatives include amoxicillin-clavulanic acid (Augmentin), azithromycin (Zithromax), cefaclor (Ceclor), clarithromycin (Biaxin), and erythromycin.
Preschool-aged children who require hospital admission are treated with cefuroxime or cefotaxime. (7,15) Once the child is afebrile and stable, he or she is switched to an oral antibiotic and treated on an outpatient basis.
OLDER CHILDREN
S. pneumoniae is a significant pathogen in school-aged children and adolescents (i.e., five to 18 years of age) with CAP. M. pneumoniae and C. pneumoniae infections also are more common in these children than in other age groups. (1)
In school-aged children, pneumococcal pneumonia usually begins with a high fever and sputum-producing cough. M. pneumoniae infection often begins with headache or gastrointestinal symptoms; rhinorrhea is uncommon. (7) Other symptoms, such as fever, arthralgia, and cough, in a school-aged child suggest Mycoplasma infection. (1) A clinical decision tree for ruling out Mycoplasma infection in children with CAP is presented in Figure 1. (25)
CAP caused by C. pneumoniae routinely begins with pharyngitis, followed by a cough and high fever. If pneumococcal pneumonia is suspected, high-dosage amoxicillin may be used. (1,23,26) If M. pneumoniae or C. pneumoniae infection is suspected, a macrolide antibiotic is the drug of choice. (1,23,26) Azithromycin, erythro-mycin, or clarithromycin may be used as a single agent in this age group because all of these agents provide adequate coverage for penicillin-sensitive pneumococcus. (1,7,13) Therapeutic options for hospitalized patients are cefuroxime or cefotaxime in addition to a macrolide. (15,26)
The rights holder did not grant the American Academy of Family Physicians the right to sublicense this material to a third party. For the missing item, see the original print version of this publication.
DURATION OF THERAPY
Antibiotic therapy should be continued for seven to 10 days in patients with uncomplicated CAP, although no controlled study of the optimal treatment duration exists. (15) Follow-up for outpatients should be done at 24 to 72 hours after diagnosis. (1,3,24) Reevaluation is necessary in children who continue to have unresolved symptoms or fever at 48 hours after diagnosis. In these patients, physicians should suspect inappropriate antibiotic therapy or a lung complication, such as an empyema or abscess. (1)
Asymptomatic children with normal physical findings after treatment do not need follow-up chest radiographs. (7,24,27) Repeat chest radiographs or computed tomographic scans are recommended if the illness is protracted or a complication such as empyema is suspected. (1)
Penicillin-resistant pneumococcus is a concern in the treatment of CAP. Evidence indicates that inpatient intravenous therapy with a penicillin or cephalosporin is effective against penicillin-resistant pneumococcus. Oral [beta]-lactam antibiotics are appropriate first-line therapies for patients with ambulatory CAP. (8,16,28,29)
Prevention
Childhood immunizations have helped greatly in the prevention of pneumonia in children. Pneumonia is a known complication of rubeola, varicella, and pertussis. These illnesses and the pneumonias related to them rarely are seen today because of routine childhood immunizations. (30) Pneumonia caused by H. influenzae type B also is rare, because of routine administration of the Hib vaccine.
In February 2000, a new heptavalent pneumococcal vaccine was licensed for use in the United States. This vaccine produces immunity for the seven most common disease-producing serotypes of S. pneumoniae in children. Widespread use of this vaccine is expected to decrease the incidence of invasive pneumococcal disease dramatically. (8,31) Initial trials have shown the vaccine to be highly effective in preventing invasive disease. (31) There appears to be a similar decrease in the incidence of pneumococcal pneumonia alone, (32) although the study that demonstrated this finding was limited by the inability to definitively diagnose the cause of pneumonia. More recent longitudinal data have shown a significant decrease in rates of invasive pneumococcal disease, particularly in children two years of age and younger. (33,34)
Vaccination with the heptavalent pneumococcal vaccine may increase carriage of noninvasive serotypes. A recent study (35) suggests that immunized children are more likely to develop otitis media with serotypes not covered by the heptavalent vaccination. However, the long-term benefits of heptavalent pneumococcal vaccine are promising and continue to be investigated.
The American Academy of Pediatrics (AAP) recommends influenza vaccination for all high-risk children six months of age and older. (36) To protect against the complications of influenza, including pneumonia, the AAP also recommends vaccination of all children six months through 23 months of age, to the extent logistically and economically feasible. (36,37)
Members of various family medicine departments develop articles for "Practical Therapeutics." This article is one in a series coordinated by the Department of Family and Geriatric Medicine at the University of Louisville School of Medicine, Louisville, Ky. Guest editor of the series is James G. O'Brien, M.D.
The authors indicate that they do not have any conflicts of interest. Sources of funding: none reported.
The authors thank Maggie Steptoe for assistance in the preparation of the manuscript.
REFERENCES
(1.) British Thoracic Society Standards of Care Committee. British Thoracic Society guidelines for the management of community acquired pneumonia in childhood. Thorax 2002;57(suppl 1):i1-24.
(2.) Murphy TF, Henderson FW, Clyde WA Jr, Collier AM, Denny FW. Pneumonia: an eleven-year study in a pediatric practice. Am J Epidemiol 1981;113:12-21.
(3.) Jokinen C, Heiskanen L, Juvonen H, Kallinen S, Karkola K, Korppi M, et al. Incidence of community-acquired pneumonia in the population of four municipalities in eastern Finland. Am J Epidemiol 1993;137:977-88.
(4.) Boschi-Pinto C, Debay M. Informal consultation on epidemiologic estimates for child health. 11-12 June 2001. Accessed online February 27, 2004, at: http://www.who.int/child-adolescent-health/New_Publications/ Overview/Report_of_CHERG_meeting.htm.
(5.) Redd SC, Vreuls R, Metsing M, Mohobane PH, Patrick E, Moteetee M. Clinical signs of pneumonia in children attending a hospital outpatient department in Lesotho. Bull World Health Organ 1994;72:113-8.
(6.) Juven T, Mertsola J, Waris M, Leinonen M, Meurman O, Roivainen M, et al. Etiology of community-acquired pneumonia in 254 hospitalized children. Pediatr Infect Dis J 2000;19:293-8.
(7.) Gaston B. Pneumonia. Pediatr Rev 2002;23:132-40.
(8.) McIntosh K. Community-acquired pneumonia in children. N Engl J Med 2002;346:429-37.
(9.) Bradley JS. Management of community-acquired pediatric pneumonia in an era of increasing antibiotic resistance and conjugate vaccines. Pediatr Infect Dis J 2002;21:592-8, 613-4.
(10.) Principi N, Esposito S. Mycoplasma pneumoniae and Chlamydia pneu-moniae cause lower respiratory tract disease in paediatric patients. Curr Opin Infect Dis 2002;15:295-300.
(11.) Heiskanen-Kosma T, Korppi M, Jokinen C, Kurki S, Heiskanen L, Juvonen H, et al. Etiology of childhood pneumonia: serologic results of a pro-spective, population-based study. Pediatr Infect Dis J 1998;17:986-91.
(12.) Margolis P, Gadomski A. The rational clinical examination. Does this infant have pneumonia? JAMA 1998;279:308-13.
(13.) Cincinnati Children's Hospital Medical Center Health Policy and Clini-cal Effectiveness Program. Evidence based clinical practice guideline. Community acquired pneumonia in children 60 days to 17 years of age. Accessed online February 27, 2004, at: http://www.cincinnatichildrens.org/NR/rdonlyres/ E25BBF59-5EDD-4B75-A28F-24B6F6C35016/0/PneumoniaGL.pdf.
(14.) World Health Organization. Essential drugs and medicines policy. Drugs used in bacterial infections. Accessed online February 27, 2004, at: http://www.who.int/medicines/library/bacterial_model_pres/ bacterial_content.shtml.
(15.) Alberta Clinical Practice Guidelines Steering Committee. Guideline for the diagnosis and management of community acquired pneumonia: pediatric. 2002. Accessed online June 1, 2004, at: http://www.albertadoctors.org/bcm/ama/ ama-website.nsf/AllDocSearch/87256DB000705C3F87256E0500553605/$File/ PNEUMONIA_PEDIATRICS.PDF.
(16.) McCracken GH Jr. Diagnosis and management of pneumonia in chil-dren. Pediatr Infect Dis J 2000;19:924-8.
(17.) Korppi M, Heiskanen-Kosma T, Leinonen M, Halonen P. Antigen and antibody assays in the aetiological diagnosis of respiratory infection in children. Acta Paediatr 1993;82:137-41.
(18.) Korppi M, Leinonen M. Pneumococcal immune complexes in the diagnosis of lower respiratory infections in children. Pediatr Infect Dis J1998;17:992-5.
(19.) Principi N, Esposito S. Emerging role of Mycoplasma pneumoniae and Chlamydia pneumoniae in paediatric respiratory-tract infections. Lancet Infect Dis 2001;1:334-44.
(20.) Nohynek H, Valkeila E, Leinonen M, Eskola J. Erythrocyte sedimentation rate, white blood cell count and serum C-reactive protein in assessing etiologic diagnosis of acute lower respiratory infections in children. Pediatr Infect Dis J 1995;14:484-90.
(21.) Esposito S, Bosis S, Cavagna R, Faelli N, Begliatti E, Marchisio P, et al. Characteristics of Streptococcus pneumoniae and atypical bacterial infections in children 2-5 years of age with community-acquired pneumonia. Clin Infect Dis 2002;35:1345-52.
(22.) Korppi M, Kiekara O, Heiskanen-Kosma T, Soimakallio S. Comparison of radiological findings and microbial aetiology of childhood pneumonia. Acta Paediatr 1993;82:360-3.
(23.) Bradley JS, Nelson JD. 2002-2003 Nelson's pocket book of pediatric antimicrobial therapy. 15th ed. Philadelphia: Lippincott, Williams & Wilkins;2002:31-5.
(24.) Peter G. Pneumonia. In: Burg FD, Gellis SS, Kagan BM. Gellis & Kagan's current pediatric therapy. 16th ed. Philadelphia: Saunders;1999:32-5.
(25.) Fischer JE, Steiner F, Zucol F, Berger C, Martignon L, Bossart W, et al. Use of simple heuristics to target macrolide prescription in children with community-acquired pneumonia. Arch Pediatr Adolesc Med 2002;156:1005-8.
(26.) Nelson JD. Community-acquired pneumonia in children: guidelines for treatment. Pediatr Infect Dis J 2000;19:251-3.
(27.) Gibson NA, Hollman AS, Paton JY. Value of radiological follow up of childhood pneumonia. BMJ 1993;307:1117.
(28.) Heffelfinger JD, Dowell SF, Jorgensen JH, Klugman KP, Mabry LR, Musher DM, et al. Management of community-acquired pneumonia in the era of pneumococcal resistance: a report from the Drug-Resistant Streptococcus pneumoniae Therapeutic Working Group. Arch Intern Med 2000;160:1399-408.
(29.) McCracken GH Jr. Etiology and treatment of pneumonia. Pediatr Infect Dis J 2000;19:373-7.
(30.) Mandell GL, Douglas RG, Bennett JE, Dolin R. Mandell, Douglas, and Bennett's principles of practice of infectious diseases. 5th ed. Philadel-phia: Churchill Livingstone, 2000:2416-7.
(31.) Black S, Shinefield H, Fireman B, Lewis E, Ray P, Hansen JR, et al. Effi-cacy, safety and immunogenicity of heptavalent pneumococcal conjugate vaccine in children. Northern California Kaiser Permanente Vaccine Study Center Group. Pediatr Infect Dis J 2000;19:187-95.
(32.) Black SB, Shinefield HR, Ling S, Hansen J, Fireman B, Spring D, et al. Effectiveness of heptavalent pneumococcal conjugate vaccine in children younger than five years of age for prevention of pneumonia. Pediatr Infect Dis J 2002;21:810-5.
(33.) Lin PL, Michaels MG, Janosky J, Ortenzo M, Wald ER, Mason EO Jr. Incidence of invasive pneumococcal disease in children 3 to 36 months of age at a tertiary care pediatric center 2 years after licensure of the pneumococcal conjugate vaccine. Pediatrics 2003;111(4 pt 1):896-9.
(34.) Whitney CG, Farley MM, Hadler J, Harrison LH, Bennett NM, Lynfield R, et al. Decline in invasive pneumococcal disease after the intro-duction of protein-polysaccharide conjugate vaccine. N Engl J Med 2003;348:1737-46.
(35.) Eskola J, Kilpi T, Palmu A, Jokinen J, Haapakoski J, Herva E, et al. Effi-cacy of a pneumococcal conjugate vaccine against acute otitis media. N Engl J Med 2001;344:403-9.
(36.) Committee on Infectious Diseases. American Academy of Pedi-atrics. Reduction of the influenza burden in children. Pediatrics 2002;110:1246-52.
(37.) Bridges CB, Fukuda K, Uyeki TM, Cox NJ, Singleton JA; Centers for Disease Control and Prevention, Advisory Committee on Immunization Practices. Prevention and control of influenza. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2002;51:1-31.
MICHAEL OSTAPCHUK, M.D., is assistant professor of family and geriatric medicine and associate director of the family practice resi-dency program at the University of Louisville (Ky.) School of Medicine. Dr. Ostapchuk received his medical degree from the University of Kentucky College of Medicine, Lexington, and a master's degree in science education from the University of Southern California, Los Angeles. He completed a pediatric residency at East Carolina University School of Medicine, Greenville, N.C., and a family medi-cine residency at the University of Louisville School of Medicine.
DONNA M. ROBERTS, M.D., is director of predoctoral education and associate professor in the Department of Family and Geriatric Medicine at the University of Louisville School of Medicine. Dr. Roberts received her medical degree from West Virginia University School of Medicine, Morgantown, and completed a family medi-cine residency at the University of Louisville School of Medicine.
RICHARD HADDY, M.D., is professor and vice chairman for aca-demic affairs in the Department of Family and Geriatric Medicine at the University of Louisville School of Medicine. He received his medical degree from Michigan State University College of Human Medicine, East Lansing, and completed a family medicine resi-dency at the University of Iowa Hospitals and Clinics, Iowa City. Dr. Haddy also completed a one-year fellowship in infectious diseases at the Saginaw campus of Michigan State University College of Human Medicine.
Address correspondence to Michael Ostapchuk, M.D., Department of Family and Geriatric Medicine, University of Louisville School of Medicine, Med Center One, 501 East Broadway, Suite 240, Louisville, KY 40202 (e-mail: m0osta01@gwise.louisville.edu). Reprints are not available from the authors.
COPYRIGHT 2004 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group