The number of frail older adults living in long-term care (LTC) facilities is expected to increase dramatically over the next 30 years. (1) An estimated 40 percent of adults will spend some time in an LTC facility before dying. (2) Because residents of these facilities have higher levels of functional disability and underlying medical illness than older adults in the community, they are at increased risk of acquiring infectious diseases. (3)
Pneumonia is the leading cause of morbidity and mortality in this population. It also is the leading reason for transfer to acute-care facilities. (4-6) At a median incidence rate of 1 to 1.2 per 1,000 patient-days, (4,7) residents of LTC facilities develop pneumonia approximately 10 times more frequently than older adults in the community. (3) Their hospitalization rate is reported to be nearly 30 times higher. (8)
LTC facilities include a variety of residences that provide care for patients with biologic and psychologic disabilities. Because nursing homes are the most numerous and best described of the LTC facilities, studies frequently use the terms "nursing homes" and "LTC facilities" interchangeably. (9) This article will continue that practice.
As the population of older adults grows, the LTC facility will become an increasingly important site for medical care. There is little agreement, however, about the evaluation and management of nursing home-acquired pneumonia. (3) This article summarizes recent literature on the diagnosis, treatment, and prevention of pneumonia in older persons who live in LTC facilities.
Risk Factors
The diagnosis and prevention of pneumonia in LTC facilities requires the identification and recognition of risk factors. Past retrospective studies have yielded conflicting information. (7) A recent prospective cohort study reported that older age, male sex, swallowing difficulty, and inability to take oral medications were significant risk factors. (7) A prospective, case-control study that focused on modifiable factors reported that unwitnessed aspiration, sedative medication, and the number of comorbidities were associated significantly with pneumonia. (5)
A number of factors may increase the risk of pneumonia and of cross-transmission of pathogens among LTC residents. Individual factors include malnutrition, long-term disease, functional impairment, medications, invasive devices, and prolonged antimicrobial exposure. Institutional factors include larger facilities with a single nursing unit or multiple units with shared nursing staff, group activities, low immunization rates, excessive antimicrobial use, and widespread colonization of residents with antimicrobial-resistant organisms. (1)
Etiology
The etiology of most cases of nursing home-acquired pneumonia is undetermined. (10) Barriers preventing accurate microbial testing include the inability of most patients to produce a sputum specimen suitable for analysis, and the difficulty of distinguishing between colonization and infection in viable specimens. (4,8,10,11) Frequently, patients have received empiric oral antibiotic treatment before specimens for diagnostic testing are obtained. (12)
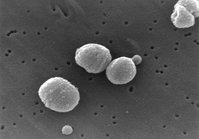
To date, no multicenter studies have used standardized definitions and comprehensive testing to establish the etiology of nursing home-acquired pneumonia. (12) This inconsistency is reflected in a wide range of results. In a 1998 survey of published studies, Streptococcus pneumoniae was identified in zero to 39 percent of specimens, Staphylococcus aureus in zero to 33 percent, and gram-negative bacteria in zero to 55 percent. (4) A recent study listed agents commonly associated with pneumonia in older adults living in the community or in LTC facilities (Table 1).12 The potential relationship between unrecognized aspiration of oral or gastric contents and the subsequent development of pneumonia in older adults is receiving more attention. An association has been reported between dysphagia and increased oropharyngeal colonization with bacteria including S. aureus and gram-negative bacilli such as Klebsiella pneumoniae and Escherichia coli. Such colonization potentially could lead to aspiration pneumonia. (13) Pseudomonas aeruginosa has been isolated from 34 percent of nasogastric tube-fed older hospitalized patients but from none of the orally fed control group. Other gramnegative organisms were isolated from 64 percent of tube-fed patients and from only 8 percent of the control group. Thus, the oropharynx of tube-fed patients could be a potential reservoir for P. aeruginosa. (14)
A recent study examined the relationship between strictly defined aspiration events and outcome in patients hospitalized with suspected pneumonia. (15) Results showed that aspiration pneumonitis, subsequent to gastric aspiration, occurred twice as often as pneumonia. Although the condition is not infectious in its initial stages, the authors report that physicians tend to treat aspiration pneumonitis with antibiotics. They report that many episodes of aspiration pneumonitis resolve with supportive care alone, and that the mortality related to this condition may differ from the mortality related to infectious pneumonia. If confirmed, this finding could have important implications for the diagnosis and management of suspected pneumonia. (15)
Diagnosis
Pneumonia in older LTC residents often presents without typical symptoms. One third may not have a fever, and many do not cough or exhibit dyspnea. (4,10)
In an earlier study of nursing home-acquired pneumonia, rapid identification of respiratory symptoms followed by prompt response, appropriate antibiotic usage, and hospitalization when indicated led to improved survival. (11) Subsequently, the authors of this study convened a national multidisciplinary, multispecialty panel (Hutt Kramer panel) of experts to develop comprehensive, evidence-based guidelines for the management of nursing home-acquired pneumonia. In 2003, the panel evaluated the published literature and graded each recommendation according to a standard system, using three categories for the strength of evidence: A (good); B (moderate); and C (poor). (11) We have translated those ratings to the strength-of-recommendation taxonomy labels used in this journal.
As noted, prompt recognition of nursing home-acquired pneumonia and rapid institution of antibiotic therapy is associated with improved outcomes. Recommendations for recognition and physician notification of serious respiratory symptoms are presented in Table 2. (11) Criteria for a diagnosis of "probable pneumonia" are presented in Table 3. (11)
Because nursing home-acquired pneumonia often is the terminal event of a long and debilitating illness, the decision to hospitalize a resident is especially important. (11) However, there are no defined criteria for determining which residents should be hospitalized. (1,15) Although one study suggested that treatment in the facility without hospitalization is beneficial, (16) there is little research to support that conclusion. (6) In the absence of standards for hospitalization, it is difficult to evaluate and compare outcome studies. Negative aspects of hospital transfer include physical discomfort, disorientation, and exposure to additional problems such as delirium, falls, incontinence, dehydration, adverse drug effects, and nosocomial infections. (17) Prospective studies to determine which residents would benefit from hospitalization for the treatment of nursing home-acquired pneumonia are needed.(18)
The Hutt Kramer panel recommends that the patient's desire for hospitalization and aggressive care be assessed directly, if possible, or by chart review or discussion with the patient's health care surrogate. Patients with orders for no hospitalization and those who refuse hospitalization, personally or through a surrogate, should not be hospitalized. (11) The panel's recommendations to guide decision making for patients willing to be hospitalized are presented in Table 4. (11)
Treatment
In comparison with community-acquired pneumonia, far fewer studies address the management of nursing home-acquired pneumonia. (3,12) In 2000, members of the Society for Healthcare Epidemiology of America (SHEA) formulated minimum criteria for the empiric initiation of antibiotics in clinically stable residents of LTC facilities with signs and symptoms of bacterial infection. They focused on the broader category of lower respiratory illnesses, which includes pneumonia and other lower respiratory tract infections. (12)
The following year, the Hutt Kramer panel published guidelines that focused specifically on pneumonia. (11) They list five recommendations for antibiotic use, which do not conflict with recently published guidelines on use of antibiotics in LTC facilities.
The SHEA group and the Hutt Kramer panel disagree about the choice of specific antibiotics. The differences involve three key factors: the relative importance of gram-negative rods as etiologic versus colonizing organisms in nursing home-acquired pneumonia; the relative importance of atypical organisms; and concern that an important percentage of bacteria in LTC facilities already may be resistant to many of the antibiotics endorsed by the SHEA group. The Hutt Kramer panel cites studies suggesting that broader spectrum empiric treatment of nursing home-acquired pneumonia provides a survival benefit. (11) The panel's recommendations include the following: antibiotics chosen as empiric therapy should cover S. pneumoniae, Haemophilus influenzae, gram-negative rods, and S. aureus; acceptable choices for empiric treatment are antipneumococcal quinolones or an extended-spectrum beta-lactam plus a macrolide; and treatment should last for 10 to 14 days.
Prognosis
Because some LTC residents are chronically ill and nearing the end of life, physicians should consider severity of illness when making treatment decisions. The scoring system presented in Table 5 (19) identifies patient characteristics that predict 30-day mortality in LTC residents with lower respiratory tract infections. Scores are assigned the following mortality risk, with the risk percentage that comes from a prospective validation of the score: 1 to 4 (low, 1.8 percent); 5 to 6 (relatively low, 5.0 percent); 7 to 8 (moderate, 11.6 percent); 9 to 10 (high, 25.0 percent); and 11 to 17 (very high, 54.2 percent). (19)
A prospective case-control study found that an episode of nursing home-acquired pneumonia is associated with significant mortality that persists for up to two years. Two risk factors--large-volume aspiration and sedating medication--are potentially modifiable. (5) The degree of dementia also is related independently to mortality attributed to nursing home-acquired pneumonia after controlling for age, comorbidity, sex, and type of treatment, including antibiotics. In addition, dementia severity was independently related to the death rate within the first week after pneumonia. The functional and pathophysiologic consequences of progressive dementia account in part for an increased three-month mortality after pneumonia, irrespective of aspiration or weight loss. (20) These findings highlight the need for advance care planning with patients and their health care surrogates, if possible, particularly about choices for treatment.
Prevention
Prevention of pneumonia in LTC facilities focuses on recognizing and modifying risk factors. These include the immunization rate, potentials for cross-transmission of pathogens during group activities and resident-health care worker interactions, and the potential for development of antimicrobial-resistant bacteria from widespread empiric use of antimicrobial therapy.
The guidelines from the Hutt Kramer panel state that residents should be vaccinated against S. pneumoniae at admission unless there is documentation of vaccination within five years before admission or of an allergic response to previous pneumococcal vaccine; residents should be vaccinated against influenza by December of each year if they are not allergic to eggs or previous influenza vaccines; residents admitted between December and March should be vaccinated if they are not already immunized for the current influenza season and are not allergic; and the facility should provide and strongly recommend influenza immunization for all employees by December of each year if the employee is not allergic to eggs or previous vaccines. (11)
Standard precautions by staff also are thought to have an impact on the transmission of antimicrobial-resistant organisms. (2) Precautions include glove use for contact with blood and body fluids and good hand hygiene. While the use of isolation and barrier precautions with colonized residents has not been shown to reduce infections from antimicrobial-resistant organisms consistently, new guidelines are being developed through the sponsorship of the Centers for Disease Control and Prevention that specifically address isolation in LTC facilities. Many state and local health departments also have developed isolation guidelines. (2)
Infections acquired in LTC facilities have a major effect on morbidity, mortality, human suffering, and health care costs. It is likely that the anticipated growth in the older adult population will be accompanied by an increased need for long-term care. Improving the prevention and management of infections must become a priority if the quality of care in these facilities is to be improved. (1)
The authors indicate that they have no conflicts of interest. Sources of funding: none reported.
Members of various family medicine departments develop articles for "Practical Therapeutics." This article is one in a series coordinated by the Department of Family and Geriatric Medicine at the University of Louisville School of Medicine, Louisville, Ky. Guest editor of the series is James G. O'Brien, M.D.
TABLE 2
Recommendations for Recognition and Physician Notification of Serious Respiratory Symptoms
Physicians caring for long-term care residents should be available or offer cross-coverage by pager 24 hours a day, seven days a week.
Staff should page the physician within one hour when a resident is noted to have any two of the following signs or symptoms: new or worsening cough; increased or newly purulent sputum; decline in cognitive, physical, or functional status; fever; hypothermia; dyspnea; tachypnea; chest pain; new or worsening hypoxemia.
Evaluation at symptom onset should include vital signs (temperature, pulse rate, respiratory rate, and blood pressure) and oxygen saturation if a pulse oximeter is available.
When notified, the physician should call back within one hour.
If the care facility staff has not heard from the physician within one hour, the director of nurses (or a designee) should be notified; this person is responsible for asking the medical director (or a designee) to assume care of the resident until the medical director can contact the attending physician.
Information from reference 11.
TABLE 3
Criteria for Diagnosis of Probable Pneumonia
The physician and facility staff should agree that pneumonia is a possible cause of a change in respiratory status if the patient has two or more of the following signs or symptoms:
New or worsening cough
Newly purulent sputum
Temperature of 38.1[degrees]C (100.5[degrees]F), < 35.6[degrees]C (96[degrees]F), or 1.1[degrees]C (2[degrees]F) more than baseline
Respiratory rate = 25 breaths per minute
Tachycardia
New or worsening hypoxia
Pleuritic chest pain
Decline in cognitive or functional status
Physical findings on chest examination such as rales or rhonchi
Information from reference 11.
TABLE 4
Guide for Hospitalizing Willing Patients
Patients with two or more of the following symptoms should be hospitalized:
Oxygen saturation < 90% on room air at sea level
Systolic blood pressure < 90 mm Hg or 20 mm Hg less than baseline
Respiratory rate > 30 breaths per minute or 10 breaths per minute more than baseline
Requiring 3 L per minute of oxygen more than baseline
Uncontrolled chronic obstructive pulmonary disease, congestive heart failure, or diabetes mellitus
Unarousable if previously conscious
New or increased agitation
If the facility cannot provide vital sign assessment every four hours, laboratory access, parenteral hydration, and two licensed nurses per shift, consideration should be given to hospitalizing patients who have only one of the listed symptoms.
Patients with none of the listed symptoms should be treated in the care facility unless the patient or a surrogate insists on hospitalization. Information from reference 11.
REFERENCES
(1.) Richards C. Infections in residents of long-term care facilities: an agenda for research. Report of an expert panel. J Am Geriatr Soc 2002;50:570-6.
(2.) Richards CL Jr, Steele L. Antimicrobial-resistant bacteria in long-term care facilities: infection control considerations. J Am Med Dir Assoc 2003;4(3 suppl):S110-4.
(3.) Muder RR. Approach to the problem of pneumonia in long-term care facilities. Compr Ther 2000;26:255-62.
(4.) Muder RR. Pneumonia in residents of long-term care facilities: epidemiology, etiology, management, and prevention. Am J Med 1998;105:319-30.
(5.) Vergis EN, Brennen C, Wagener M, Muder RR. Pneumonia in long-term care: a prospective case-control study of risk factors and impact on survival. Arch Intern Med 2001;161:2378-81.
(6.) Binder EF, Kruse RL, Sherman AK, Madsen R, Zweig SC, D'Agostino R, et al. Predictors of short-term functional decline in survivors of nursing home-acquired lower respiratory tract infection. J Gerontol A Biol Sci Med Sci 2003;58:60-7.
(7.) Loeb M, McGeer A, McArthur M, Walter S, Simor AE. Risk factors for pneumonia and other lower respiratory tract infections in elderly residents of long-term care facilities. Arch Intern Med 1999;159:2058-64.
(8.) Marrie TJ. Pneumonia in the long-term-care facility. Infect Control Hosp Epidemiol 2002;23:159-64.
(9.) Strausbaugh LJ, Joseph CL. The burden of infection in long-term care. Infect Control Hosp Epidemiol 2000;21:674-9.
(10.) Medina-Walpole AM, Katz PR. Nursing home-acquired pneumonia. J Am Geriatr Soc 1999;47:1005-15.
(11.) Hutt E, Kramer AM. Evidence-based guidelines for management of nursing home-acquired pneumonia. J Fam Pract 2002;51:709-16.
(12.) Loeb M. Pneumonia in older persons. Clin Infect Dis 2003;37:1335-9.
(13.) Marik PE, Kaplan D. Aspiration pneumonia and dysphagia in the elderly. Chest 2003;124:328-36.
(14.) Leibovitz A, Dan M, Zinger J, Carmeli Y, Habot B, Segal R. Pseudomonas aeruginosa and the oropharyngeal ecosystem of tube-fed patients. Emerg Infect Dis 2003;9:956-9.
(15.) Mylotte JM, Goodnough S, Naughton BJ. Pneumonia versus aspiration pneumonitis in nursing home residents: diagnosis and management. J Am Geriatr Soc 2003;51:17-23.
(16.) Fried TR, Gillick MR, Lipsitz LA. Short-term functional outcomes of long-term care residents with pneumonia treated with and without hospital transfer. J Am Geriatr Soc 1997;45:302-6.
(17.) Ouslander JG, Weinberg AD, Phillips V. Inappropriate hospitalization of nursing facility residents: a symptom of a sick system of care for frail older people. J Am Geriatr Soc 2000;48:230-1.
(18.) Mylotte JM. Nursing home-acquired pneumonia. Clin Infect Dis 2002;35:1205-11.
(19.) Mehr DR, Binder EF, Kruse RL, Zweig SC, Madsen R, Popejoy L, et al. Predicting mortality in nursing home residents with lower respiratory tract infection: the Missouri LRI study. JAMA 2001;286:2427-36.
(20.) Van der Steen JT, Ooms ME, Mehr DR, van der Wal G, Ribbe MW. Severe dementia and adverse outcomes of nursing home-acquired pneumonia: evidence for mediation by functional and pathophysiological decline. J Am Geriatr Soc 2002;50:439-48.
CHRISTIAN DAVIS FURMAN, M.D., M.S.P.H., is assistant professor of internal medicine and assistant professor of family and geriatric medicine at the University of Louisville School of Medicine, Louisville, Ky. She received her medical degree and completed a residency in internal medicine at the University of Louisville School of Medicine. She completed a geriatric fellowship and obtained a master's degree in public health at the University of Louisville.
ABI V. RAYNER, M.D., is assistant professor in the Department of Epidemiology and Clinical Investigative Sciences, University of Louisville School of Public Health and Information Science. She received her medical degree from the University of Florida College of Medicine, Gainesville. She completed a family practice residency at the University of Wyoming School of Human Medicine, Casper.
ELISABETH PELCHER TOBIN, PH.D., is research associate in the Department of Family and Geriatric Medicine, University of Louisville School of Medicine. She received a master's degree in food microbiology from the University of Illinois, Urbana, and a master's degree in health systems and a doctorate in health policy analysis from the University of Louisville. Address correspondence to Christian Davis Furman, M.D., M.S.P.H., Med Center One Building, Second Floor, Department of Family and Geriatric Medicine, University of Louisville School of Medicine, Louisville, KY 40202 (e-mail: cdfurm02@louisville.edu). Reprints are not available from the authors.
COPYRIGHT 2004 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group