The Pulmonary Complications, ICU Support, and Prognostic Factors of Hospitalized Patients With HIV (PIP) Study
Study objectives: To describe the causative organisms and factors associated with bacterial pneumonia and to assess its impact on the outcome of hospitalized patients with HIV.
Design: Prospective, observational.
Setting: A university-affiliated medical center.
Methods: We included 1,225 consecutive hospital admissions, from April 1995 through March 1998, of 599 adults with HIV. We collected data on APACHE II (acute physiology and chronic health evaluation II) score, leukocyte and CD4+ lymphocyte counts, length of hospital stay, ICU admission rate, and case-fatality rate. Chest radiographs and laboratory results were reviewed. The presence of bacterial pneumonia was noted.
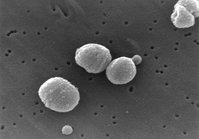
Results: Bacterial pneumonia was diagnosed in 111 hospitalizations (9%): 80 (72%) were community-acquired infections. The CD4+ lymphocyte count was lower (median, 38 vs 66/[micro]L, p = 0.0027), APACHE II score higher (17 vs 13, p [is less than] 0.0001), length of hospital stay longer (median, 6 vs 4), and ICU admission (28% vs 9%) and case-fatality rates (21% vs 4%) higher in patients with bacterial pneumonia compared with those without bacterial pneumonia. The most common pathogen was Pseudomonas aeruginosa (32 admissions), followed by Streptococcus pneumoniae (22 admissions), Staphylococcus aureus (16 admissions), and Haemophilus influenzae (11 admissions). Thirty-three (30%) of the pneumonias were bacteremic. Bacteremia was more common in pneumococcal than in pseudomonal pneumonia (95% vs 9%, p [is less than] 0.0001). Compared with patients with pneumococcal pneumonia, patients with pseudomonal pneumonia had lower leukocyte and CD4+ lymphocyte counts, longer hospital stay, and similar case-fatality rate.
Conclusions: P aeruginosa is becoming a common cause of both community-acquired and nosocomial bacterial pneumonia in hospitalized patients with HIV, especially in those with low leukocyte and CD4+ lymphocyte counts.
(CHEST 2000; 117:1017-1022)
Key words: AIDS; bacterial pneumonia; HIV; ICU admission; mortality; Pseudmonas aeruginosa infection; Streptococcus pneumoniae infection
Abbreviation: APACHE II = acute physiology and chronic health evaluation II
Since the beginning of the AIDS epidemic, the lungs have continued to be a frequent site of organ complication. Traditionally, pulmonary infections in patients with HIV have been classified into opportunistic and nonopportunistic. Opportunistic infections are caused by organisms that do not cause disease in immunocompetent individuals. However, any human pathogenic organism can cause disease in patients with HIV, blurring this classic classification. The type of pulmonary infection occurring in an HIV-infected patient depends on the stage of the HIV infection, the individual history of prior infection, the virulence of the infecting organism, and other host-related factors, such as the disease exposure category and geographic location. Various defects in immunity have been described early in the disease process of patients with HIV infection, before we see a decline in the CD4+ lymphocyte count. In addition to the low CD4+ lymphocyte count, humoral immune dysfunction, depressed IgA2 and IgG2 levels, and decreased CD4+ T-lymphocyte cell-mediated antibody-dependent cellular cytotoxicity are also present in HIV-infected patients, predisposing them to bacterial infections.[1-3] Bacterial infections are the most common respiratory complications in patients with HIV infection.4 These infections occur at all levels of CD4+ lymphocyte count but become more frequent as the CD4+ lymphocyte count declines.[5,6] The purpose of this study was to describe the incidence and types of bacterial pneumonia in hospitalized patients with HIV infection and to determine the factors associated with it and its impact on patient outcome.
MATERIALS AND METHODS
This prospective, observational study included 1,225 consecutive hospital admissions of 599 adults with HIV infection treated at the University Medical Center, Jacksonville, FL, from April 1995 through March 1998. All adults with HIV infection who were admitted to the hospital were included in the study. The University Medical Center is a 528-bed, teaching inner-city hospital affiliated with the University of Florida. The need for informed consent was waived by the Institutional Review Board of the hospital.
Bacterial pneumonia was defined by the presence of new or worsening infiltrate on chest radiograph, temperature [is greater than] 100.4 [degrees] F or [is less than] 96.8 [degrees] F, leukocyte count [is greater than] 12,000/[mm.sup.3] or [is less than] 4,000/[mm.sup.3] or bandemia [is greater than] 10%, and sputum Gram's stain or culture showing a bacterial organism in a purulent sputum or quantitative culture of BAL showing bacteria [is greater than or equal to] [10.sup.4]/mL or the isolation of a likely pathogen from blood, or pleural fluid or urine positive for Legionella pneumophila antigen. Purulent sputum was identified by the presence of [is greater than] 25 WBCs and [is less than] 10 epithelial cells per microscopic low-power field of a sputum sample. Nosocomial pneumonia was defined as pneumonia that developed after 48 h of hospitalization or within 14 days of previous hospitalization. All chest radiographs were reviewed by one of the investigators (B.A.), a pulmonologist. We collected data on age, sex, race, exposure category for HIV infection, place of acquisition, WBC count, CD4+ lymphocyte count, APACHE II (acute physiology and chronic health evaluation II) score, chest radiograph findings, the presence of bacteremia, ICU admission status, length of hospital stay, and in-hospital mortality. For the purpose of this study, each admission was considered as one patient and termed a patient-admission.
StatView 5.0 computer software (SAS Institute Inc.; Cary, NC) was used for statistical analysis. Results are expressed as mean [+ or -] SD. Comparisons between groups were made using Student's t test, Mann-Whitney U test, [chi square], Fisher's Exact Test, and logistic regression analysis. Probability values [is less than] 0.05 were considered significant.
RESULTS
The demographic characteristics, exposure categories, CD4+ lymphocyte count, and APACHE II scores of the patients are listed in Table 1.
Table 1--Demographic Characteristics, Exposure Categories, CD4+ Lymphocyte Count, and APACHE II Scores of 1,225 Hospital Admissions of 599 Patients With HIV(*)
(*) Age of patients (mean [+ or -] SD) was 38.2 [+ or -] 8.9 years.
One hundred eleven of the 1,225 patient-admissions (9%) had bacterial pneumonia: 80 (72%) community-acquired and 31 (28%) nosocomial. The 111 episodes of bacterial pneumonia occurred in 94 patients: one episode in 82 patients, two episodes in 10 patients, three episodes in 1 patient, and six episodes in 1 patient. The causative organisms are listed in Table 2. Among the 12 patients with two or more episodes of bacterial pneumonia, 4 had repeated episodes caused by Pseudomonas aeruginosa, and 8 had repeated episodes caused by different organisms, none by the same organism. Pneumocystis carinii pneumonia was present in 14 of the 111 patient-admissions with bacterial pneumonia (13%). Fiberoptic bronchoscopy, performed in 69 patient-admissions, was diagnostic of bacterial pneumonia in 3, all from P aeruginosa. Fifty-seven of the organisms were Gram-negative and 43 were Gram-positive. Although the sputum Gram's stain showed organisms, the cultures were negative in 11 patients. All BAL specimens were examined for the presence of Mycoplasma pneumoniae and L pneumophila infection. However, no atypical bacterial pneumonia was diagnosed by bronchoscopy. There was one case of L pneumophila pneumonia detected by direct fluorescence antibody for urine antigen.
Table 2--Bacterial Pathogens Isolated in 111 Episodes of Pneumonia in Patients With HIV
There were no significant differences in age, sex, and risk factors for HIV infection between patients with or without bacterial pneumonia (Table 3). Bacterial pneumonia was more common in Hispanics compared with African Americans and whites (Table 3). The CD4+ lymphocyte count was lower and the APACHE II score higher in patients with bacterial pneumonia compared with those without bacterial pneumonia (Table 3). Of the 111 bacterial pneumonias, 33 (30%) were bacteremic: Streptococcus pneumoniae (21), P aeruginosa (3), Streptococcus viridans (3), Staphylococcus aureus (2), Escherichia coli (1), Haemophilus influenza (1), Enterococcus spp (1), and Group C streptococcus (1). Twenty (91%) of the pneumococcal isolates were fully sensitive to penicillin, and 2 (9%) were intermediately sensitive.
Table 3--Differences in Age, Sex, Race, Exposure Category, CD4+ Lymphocyte Count, and APACHE II Scores Between Patients With or Without Bacterial Pneumonia
The differences in the length of hospital stay, ICU admission rate, and in-hospital mortality between patients with or without bacterial pneumonia are listed in Table 4. The in-hospital mortality rate of patients with bacterial pneumonia was 21% (23 of 111). Multiple logistic regression analysis showed that there was a significant difference only in APACHE II score (15 vs 25, p = 0.0003) not in CD4+ lymphocyte count (50 vs 18/[micro]L, p = 0.6431) or in incidence of bacteremia (28% vs 35%, p = 0.7128) between survivors and nonsurvivors with bacterial pneumonia.
Table 4--Differences in Length of Hospital Stay, ICU Admission Rate, and In-Hospital Mortality Between Patients With or Without Bacterial Pneumonia
P aeruginosa and S pneumoniae were the two most common causes of bacterial pneumonia. There were no significant differences in age, sex, race, and exposure category between patients with pseudomonal or pneumococcal pneumonia. Twenty of the 22 pneumococcal pneumonias (91%) were community-acquired compared with 20 of the 32 pseudomonal pneumonias (63%; p = 0.0269). The differences in APACHE II score, WBC count, CD4+ lymphocyte count, incidence of bacteremia, incidence of pleural effusions and multilobar infiltrate on chest radiograph, ICU admission rate, length of hospital stay, and in-hospital mortality between patients with pseudomonal and pneumococcal pneumonia are listed in Table 5.
Table 5--Differences in APACHE II Score, Leukocyte Count, CD4+ Lymphocyte Count, Incidence of Bacteremia, Incidences of Pleural Effusion and Multilobar Infiltrate on Chest Radiograph, ICU Admission Rate, Length of Hospital Stay, and In-Hospital Mortality Between Patients With Pseudomonal and Pneumococcal Pneumonia
DISCUSSION
This study describes 111 cases of bacterial pneumonia among 1,225 hospital admissions of 599 patients with HIV infection. P aeruginosa and S pneumoniae were the two most common causative pathogens.
Early in the HIV epidemic, researchers noted that bacterial pneumonia was a common cause of morbidity.[7-9] Decreasing CD4+ lymphocyte count, injection drug use, prior sinusitis, and prior lower respiratory tract bacterial infection are risk factors for bacterial pneumonia in patients with HIV infection.[5,10-12] A recent multicenter study showed the incidence of bacterial pneumonia to be 5.5 per 100 person-years among HIV seropositive individuals[10] ; this incidence was higher than that of P carinii pneumonia.[10] An autopsy study from two medical centers has confirmed bacterial pneumonia to be the most common pulmonary complication in patients with HIV.[13] The cumulative incidence of bacterial pneumonia in hospitalized patients with HIV infection may be as high as 12.5 per 100 person-years.[11] In our study, the incidence of bacterial pneumonia was 9 per 100 inpatients. However, this number underestimates the actual incidence, because we did not include the cases that were empirically treated for presumed pneumonia without obtaining respiratory specimens to confirm the diagnosis. Unlike previous studies, we did not find a significant relationship between injection drug use and bacterial pneumonia. Although the incidence of bacterial pneumonia was higher in Hispanics in our study, we cannot make any reasonable conclusion because only nine patients were of Hispanic origin.
The annual incidence of pneumococcal bacteremia is estimated to be as high as 940 per 100,000 patients with AIDS.[14] In certain regions, the majority of adults with pneumococcal infection and [is less than] 40 years of age are HIV seropositive.[15,16] Previous studies have shown S pneumoniae to be the most common cause of bacterial pneumonia.[5,8,11] In our study, S pneumoniae was not the most common pathogen causing bacterial pneumonia. S pneumoniae is isolated in blood cultures of 60% of HIV-infected patients with pneumococcal pneumonia and 15 to 30% of patients without HIV infection.[1] In the multicenter study by the Pulmonary Complications of HIV Infection Study Group, 11 of the 36 pneumococcal pneumonias (31%) were bacteremic.[5] In our study, 95% of the pneumococcal pneumonias were bacteremic, suggesting underdiagnosis of nonbacteremic pneumococcal pneumonia. Because our study was purely observational, we did not have any control on the management plan of the individual patients. The common medical practice in our emergency department included giving at least one IV dose each of trimethoprim/sulfamethoxazole and a third-generation cephalosporin to ill-looking HIV-infected patients with suspected pneumonia before obtaining respiratory specimens. This practice may have led to a falsely decreased incidence of pneumococcal pneumonia in our study.
Penicillin remains the drug of choice for patients infected with a susceptible strain of S pneumoniae. In the United States, 7% of S pneumoniae are penicillin-resistant compared with 44% in Spain.[17] In a study from France of HIV-infected inpatients with bacterial pneumonia, 75% of the pneumococci had decreased susceptibility to penicillin.[11] In our study, only 9% of the pneumococci had decreased susceptibility to penicillin.
Bacteremic and nonbacteremic P aeruginosa infections are becoming more common in patients with HIV.[18] An effective defense against P aeruginosa depends on functions of the epithelial cell barrier, antibodies, complement system, phagocytic cells, and lymphocytes.[19] Traditionally, P aeruginosa infection has been associated with neutropenia, hospitalization, central venous catheters, burn wounds, bronchiectasis, and cystic fibrosis.[19] The development of bronchiectasis and defects in granulocytes, chemotaxis, phagocytosis, and bacterial killing have been described in HIV-infected patients and have predisposed them to infection with P aeruginosa.[2,3,20,21] In a prospective study of HIV-infected inpatients from France, 6 of the 33 identified pathogens causing bacterial pneumonia (18%) were P aeruginosa.[11] In the multicenter study by the Pulmonary Complications of HIV Injection Study Group, P aeruginosa accounted for 6 of the 89 organisms identified as causing bacterial pneumonia (7%).[5] Other studies have highlighted the importance of P aeruginosa pneumonia in patients with HIV infection, including a rise in its incidence more recently.[22-26] Most of these infections are community-acquired.[22-26] The incidence of P aeruginosa infection in hospitalized patients with HIV is estimated to be 5.8% and on the rise.[26] In our study, the incidence of pneumonia from P aeruginosa in hospitalized patients with HIV infection was 2.6%. Unlike previous studies, we found P aeruginosa, not S pneumoniae, to be the most common pathogen causing bacterial pneumonia in our patients. The underdiagnosis of pneumococcal pneumonia in our study, caused by technical difficulties in culturing S pneumoniae and empiric antibiotic use before obtaining adequate respiratory samples, may partly explain this unexpected finding. The low CD4+ lymphocyte count in our patients with pseudomonal pneumonia was similar to the findings in other studies.[22,25]
Atypical bacterial pneumonia was diagnosed in only one patient in our study. The Pulmonary Complications of HIV Infection Study Group reported only one case of L pneumophila among 237 episodes of bacterial pneumonia in HIV-positive patients.[5] There are case reports of pneumonia caused by Bordetella bronchiseptica in patients with HIV infection.[27,28] B bronchiseptica was the only unusual bacterial pathogen found to cause pneumonia in our study.
Recent trends among persons dying of HIV infection in the United States show an increase in the percentage of deaths associated with bacterial pneumonia.[29] An Italian study of 350 episodes of bacterial pneumonia reported a case-fatality rate of 27%.[12] The case-fatality rate was 21% in our study. Compared with patients without bacterial pneumonia, patients with bacterial pneumonia had longer length of hospital stay and higher ICU admission and case-fatality rates in our study. This indicates the adverse impact of bacterial pneumonia on the morbidity and mortality of hospitalized patients with HIV infection.
Our study has several limitations. The diagnostic and therapeutic approaches varied according to each patient's primary physician. The initiation of empiric antibiotic therapy before obtaining respiratory specimen samples may have led to the underdiagnosis of bacterial pneumonia, pneumococcal in particular. Although there were patients whose clinical presentation and response to therapy were consistent with bacterial pneumonia, they were not considered as having bacterial pneumonia unless they had microbiologic evidence of bacterial pneumonia. This may have led to underestimation of the incidence of bacterial pneumonia. Because we were unable to document the patients' antiretroviral treatment and trimethoprim/sulfamethoxazole use before hospitalization, we could not determine their effect on the incidence and type of the bacterial pneumonia.
In summary, we have described the incidence and types of bacterial pneumonia in hospitalized patients with HIV infection. Pseudomonal pneumonia is becoming a common pulmonary complication, especially in patients with low leukocyte and CD4+ lymphocyte counts. Compared with pneumococcal pneumonia, pseudomonal pneumonia is associated with a lower incidence of bacteremia and a longer hospital stay. Despite the low CD4+ lymphocyte and leukocyte counts associated with pseudomonal pneumonia, the mortality rate is only 19%. We need to closely monitor the changes in disease patterns, including the pathogens causing pneumonia, in different institutions and regions. Our observations suggest that pseudomonal pneumonia should be included in the differential diagnosis of both community-acquired and nosocomial pneumonia in patients with HIV infection.
ACKNOWLEDGMENT: We thank Dr. David L. Armbruster for editing our manuscript.
REFERENCES
[1] Janoff EN, Breiman RE, Daley CL, et al. Pneumococcal disease during HIV infection: epidemiologic, clinical, and immunologic perspectives. Ann Intern Med 1992; 117:314-324
[2] Lane HC, Masur H, Edgar LC, et al. Abnormalities of B-cell activation and immunoregulation in patients with the acquired immunodeficiency syndrome. N Engl J Med 1983; 309:453-458
[3] Ammann AJ, Schiffman G, Abrams D, et al. B-cell immune deficiency syndrome. JAMA 1984; 251:1447-1449
[4] Wallace JM, Rao AV, Glassroth J, et al. Respiratory illness in persons with human immunodeficiency virus infection. Am Rev Respir Dis 1993; 148:1523-1529
[5] Hirschtick R, Glassroth J, Jordan MC, et al. Bacterial pneumonia in patients infected with human immunodeficiency virus. N Engl J Med 1995; 333:845-851
[6] Jung AC, Paauw DS. Diagnosing HIV-related disease. using CD4 count as a guide. J Gen Intern Med 1998; 13:131-136
[7] Simberkoff MS, Sadr WE, Schiffman G, et al. Streptococcus pneumoniae infection and bacteremia in patients with acquired immune deficiency syndrome with report of pneumococcal vaccine failure. Am Rev Respir Dis 1984; 130:11741176
[8] Polsky B, Gold JWM, Whimbey E, et al. Bacterial pneumonia in patients with acquired immunodeficiency syndrome. Ann Intern Med 1986; 104:38-41
[9] Witt DJ, Craven DE, McCabe WR. Bacterial infections in adult patients with acquired immune deficiency syndrome (AIDS) and AIDS-related complex. Am J Med 1987; 82:900-906
[10] Wallace JM, Hansen NI, Lavange L, et al. Respiratory disease trends in the pulmonary complications of HIV Infection Study Cohort. Am J Respir Crit Care Med 1997; 155:72-80
[11] Baril L, Astagneau P, Nguyen J, et al. Pyogenic bacterial pneumonia in human immunodeficiency virus-infected inpatients: a clinical, radiological, microbiological, and epidemiological study. Clin Infect Dis 1998; 26:964-971
[12] Tumbarello M, Tacconelli E, de Gaetano K, et al. Bacterial pneumonia in HIV-infected patients: analysis of risk factors and prognostic indicators. J Acquir Immune Defic Syndr Hum Retrovirol 1998; 18:39-45
[13] Afessa B, Green W, Chiao J, et al. Pulmonary complications of HIV infection: autopsy findings. Chest 1998; 113:1225-1229
[14] Redd SC, Rutherford GW, Sande MA, et al. The role of human immunodeficiency virus infection in pneumococcal bacteremia in San Francisco residents. J Infect Dis 1990; 162:1012-1017
[15] Garcia-Leoni ME, Moreno S, Rodeno P, et al. Pneumococcal pneumonia in adult hospitalized patients infected with the human immunodeficiency virus. Arch Intern Med 1992; 152:1808-1812
[16] Afessa B, Greaves WL, Frederick WR. Pneumococcal bacteremia in adults: differences between patients with and without human immunodeficiency virus infection. Int J Infect Dis 1997; 2:21-25
[17] Friedland IR, McCracken GH. Management of infections caused by antibiotic resistant Streptococcus pneumoniae. N Engl J Med 1994; 331:377-382
[18] Dropulik LK, Leslie JM, Eldred LJ, et al. Clinical manifestations and risk factors of Pseudomonas aeruginosa infection in patients with AIDS. J Infect Dis 1995; 171:930-937
[19] Bodey GP, Boliver R, Fainstein V, et al. Infections caused by Pseudomonas aeruginosa. Rev Infect Dis 1983; 5:279-313
[20] Murphy PM, Lane HC, Fauci AS, et al. Impairment of neutrophil bactericidal capacity in patients with AIDS. J Infect Dis 1988; 158:627-630
[21] Holmes AH, Trotmand-Dickerson B, Edwards A, et al. Bronchiectasis in HIV disease. Q J Med 1992; 85:875-882
[22] Baron AD, Hollander H. Pseudomonas aeruginosa bronchopulmonary infection in late human immunodeficiency virus disease. Am Rev Respir Dis 1993; 148:992-996
[23] Shepp DH, Tang ITL, Ramundo MB, et al. Serious Pseudomonas aeruginosa infection in AIDS. J Acquir Immune Defic Syndr 1994; 7:823-831
[24] Mendelson MH, Gurtman A, Szabo S, et al. Pseudomonas aeruginosa bacteremia in patients with AIDS. Clin Infect Dis 1994; 18:886-895
[25] Schuster MG, Norris AH Community-acquired Pseudomonas aeruginosa pneumonia in patients with HIV infection. AIDS 1994; 8:1437-1441
[26] Fichtenbaum CJ, Woeltje KF, Powderly WG. Serious Pseudomonas aeruginosa infections in patients infected with human immunodeficiency virus: a case-control study. Clin Infect Dis 1994; 19:417-422
[27] Lawson RA. Bordetella bronchiseptica pneumonia [letter]. Thorax 1994; 49:1278
[28] Libanore M, Rossi MR, Pantaleoni M, et al. Bordetella bronchiseptica pneumonia in an AIDS patient: a new opportunistic infection. Infection 1995; 23:312-313
[29] Selik RM, Chu SY, Ward JW. Trends in infectious diseases and cancers among persons dying of HIV infection in the United States from 1987 to 1992. Ann Intern Med 1995; 15:933-936
(*) From the Department of Internal Medicine, Division of Pulmonary and Critical Care, University of Florida Health Science Center, Jacksonville, FL.
Manuscript received May 11, 1999; revision accepted September 9, 1999.
Correspondence to: Bekele Afessa, MD, FCCP, Division of Pulmonary and Critical Care Medicine, Department of Medicine, University of Tennessee, Memphis, 956 Court Ave, Rm H314, Memphis, TN 38163; e-mail: Bafessa@UTMEM1.UTMEM.EDU
COPYRIGHT 2000 American College of Chest Physicians
COPYRIGHT 2000 Gale Group