Background: Community-acquired pneumonia (CAP) is a major cause of morbidity and mortality worldwide. The inability or failure of many subjects to adhere to standard antibiotic regimens, which may last up to 10 days, results in suboptimal antibiotic treatment. Treatment with a single-dose antibiotic regimen may improve compliance with prescribed therapy. A novel microsphere formulation of azithromycin provides a single-dose regimen while maintaining tolerability.
Study objective: To compare the efficacy and safety of a single 2.0-g dose of azithromycin microspheres to that of an extended-release formulation of clarithromycin (1.0 g/d for 7 days) for the treatment of adults with mild-to-moderate CAP.
Design: A phase III, multinational, multicenter, randomized, double-blind, double-dummy study, comparing single-dose azithromycin microspheres to extended-release clarithromycin, both administered orally.
Methods: Subjects with mild-to-moderate CAP (Fine class I and II) were included. The primary end point was clinical response at the test-of-cure (TOC) visit (days 14 to 21) in the clinical per protocol (CPP) population. The bacteriologic response at the TOC visit was assessed in subjects with a baseline pathogen.
Results: A total of 501 subjects were randomized, and 499 were treated. Clinical cure rates at the TOC visit in the CPP population were 92.6% (187 of 202 subjects) for azithromycin microspheres and 94.7% (198 of 209 subjects) for extended-release clarithromycin. Overall pathogen eradication rates were 91.8% (123 of 134 subjects) for azithromycin microspheres and 90.5% (153 of 169 subjects) for extended-release clarithromycin. Both agents were well tolerated. The incidence of treatment-related adverse events was 26.3% with azithromycin microspheres and 24.6% with extended-release clarithromycin. Most adverse events were mild to moderate in severity.
Conclusion: A single 2.0-g dose of azithromycin microspheres was as effective and well tolerated as a 7-day course of extended-release clarithromycin in the treatment of adults with mild-to-moderate CAP.
Key words: azithromycin; clarithromycin; community-acquired pneumonia; single-dose regimen
Abbreviations: BPP = bacteriologic per protocol; CAP = community acquired pneumonia; CI = confidence interval; CPP = clinical per protocol; MIC = minimum inhibitory concentration; TOC = test of cure
**********
Community-acquired pneumonia (CAP) is a common and serious lower respiratory tract infection and is associated with significant morbidity and mortality worldwide. Estimates of incidence vary according to the population surveyed: 0.3% in the United Kingdom, 0.5% in Sweden, 2% in Australia, and 2.3% in the United States. (1-3) The incidence of CAP is highest at the extremes of age: in the United States, it is highest among those aged [greater than or equal to] 65 years (2.4%) and < 7 years (2.6%). (1,4) Approximately 2 to 5 million cases of CAP occur annually in the United States, where it is the sixth most common cause of death and the main cause of death due to infection. (5-7) CAP results in approximately 10 million physician visits, 500,000 hospitalizations, and 45,000 deaths annually. (8) In the United States, most CAP subjects are treated as outpatients, but approximately 20% require hospitalization. (9,10)
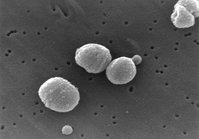
In the majority of outpatients, a causative pathogen is not identified prior to the start of therapy. (5) Antibiotic therapy for CAP is thus usually empiric and is directed against the most common typical and atypical pathogens: Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, Chlamydia pneumoniae, Mycoplasma pneumoniae, and Legionella pneumoniae. (11-13) Several treatment guidelines (4,10,13) recommend oral macrolides, including the azalide antibiotic azithromycin, as first-line agents for the outpatient treatment of CAP in North America.
Oral azithromycin has been used successfully for the treatment of mild-to-moderate CAP, as either a 5-day or a 3-day regimen, for > 10 years. (14,15) Azithromycin is rapidly absorbed and achieves sustained high levels in respiratory tissues. (16) Azithromycin concentrates in phagocytic cells, such as macrophages and polymorphonuclear neutrophils, enabling delivery directly to sites of infection. (17,18) The 60-h half-life and favorable intrapulmonary pharmacokinetics of azithromycin make it a good candidate for the short-course treatment of CAP. (19,20)
A novel microsphere formulation of azithromycin has recently been developed that makes it possible to administer a higher oral dose of azithromycin as a single-dose regimen while maintaining tolerability. The maximum concentration and 24-h area under the curve after a single 2.0-g dose of azithromycin microspheres are two and three times higher, respectively, than those achieved with 1.5 g of conventional, immediate-release azithromycin administered over either 3 days (500 mg qd x 3) or 5 days (500 mg on day 1, followed by 250 mg qd x 4). This so-called "front loading" of the dose early in the course of infection maximizes drug exposure when bacterial burden is highest. Front loading also increases the 24-h area under the curve/minimum inhibitory concentration (MIC) ratio, the pharmacokinetic/pharmacodynamic parameter that best predicts efficacy of azithromycin. (21) Data from animal infection models suggest that this approach is effective in a variety of respiratory tract infections. (22-24) Administration of a single, large dose of azithromycin has been shown to achieve more rapid bacterial eradication and enhanced survival than the same dose divided over several days in preclinical infection models of otitis media, murine pneumonia, and septicemia. (23,24) This study was designed to evaluate the efficacy and safety of a single 2.0-g dose of azithromycin microspheres, compared to that of a 7-day course of an extended-release formulation of clarithromycin, 1.0 g/d for 7 days, for the treatment of adults with mild-to-moderate CAP.
SUBJECTS AND METHODS
Study Design
This was a phase III, multinational, multicenter, double-blind, double-dummy study in which subjects were randomized, in a 1:1 ratio, to either azithromycin microspheres or extended-release clarithromycin. A single 2.0-g dose of azithromycin microspheres was administered as an oral suspension. Extended-release clarithromycin was administered orally as two 500-mg capsules qd for 7 days. The first dose of each study medication was administered in an observed setting; all subjects received a single dose of azithromycin microspheres or placebo, followed by two capsules of extended-release clarithromycin or placebo 30 min later. Subsequently, subjects were directed to take two capsules (extended-release clarithromycin/placebo) daily on days 2 through 7. Eligible subjects were required to be [greater than or equal to] 16 years old, with evidence of mild-to-moderate CAP as defined by a prospectively calculated modified Fine risk score of [less than or equal to] 70 (Fine classes I and II). (25)
The study was conducted in 58 outpatient centers worldwide (25 in the United States, 10 in Canada, 6 in Argentina, 6 in Russia, 5 in India, 4 in Estonia, and 2 in Lithuania), with a planned enrollment of approximately 504 subjects. Subjects were randomized according to a computer-generated pseudorandom code using the method of permutated blocks, balanced within investigational site. Randomization numbers were assigned by a central Web/telephone computer-based telerandomization system.
Subject assessments were conducted at baseline (day 1), on treatment (days 3 to 5), end-of-treatment (telephone contact, days 8 to 11), posttreatment test of cure (TOC) [days 14 to 21], and at a long-term follow-up visit (days 28 to 35). Clinical efficacy was assessed at the TOC visit. Subjects from whom a pathogen was identified at baseline were also assessed for bacteriologic response. The study was conducted according to the Declaration of Helsinki, and the study protocol was reviewed and approved by the institutional review boards of the participating centers.
Subjects
Written, informed consent was obtained from all study subjects or a legally authorized representative. To be eligible for enrollment in the study, subjects had to meet the following inclusion criteria: men or women aged [greater than or equal to] 16 years, for whom oral, outpatient therapy was indicated; cough productive of sputum; diagnosis of pneumonia as demonstrated by two or more of the following signs or symptoms: auscultatory findings on pulmonary examination of rales and/or evidence of pulmonary consolidation; dyspnea or tachypnea; body temperature > 38[degrees]C (oral); or an elevated total peripheral WBC count (> 10,000/[micro]L) or > 15% immature neutrophils (bands). Subjects were required to undergo chest radiography, posteroanterior and lateral, revealing the presence of a new infiltrate or consolidation that could not be attributed to a process other than pneumonia; and a modified Fine risk score of [less than or equal to] 70 (Fine classes I and II). Women of childbearing potential were required to have a negative urine pregnancy test result within 48 h prior to start of study medication. Exclusion criteria included previously diagnosed conditions that might mimic or complicate the course and the evaluation of the infectious process (eg, bronchiectasis, lung abscess or empyema, active tuberculosis, pulmonary malignancy, cystic fibrosis, postobstructive pneumonia); hospitalization in the previous 14 days or infection acquired in hospital; and residence in a long-term care facility.
The primary population for analysis was the clinical per protocol (CPP) population, which consisted of clinically eligible subjects (all treated subjects with a clinical diagnosis of CAP) who received 6 days of study medication, including active plus placebo doses; who received no concomitant systemic antibiotic potentially effective against CAP pathogens; and who received an assessment in the appropriate visit window. Treatment failures in the clinically eligible population who received at least 3 days of study medication were also included in the CPP population. The bacteriologic per protocol (BPP) population included those CPP subjects in whom a baseline bacterial pathogen was identified. Sputum specimens were cultured for typical bacterial pathogens such as S pneumoniae, H influenzae, and M catarrhalis. Laboratory workup for M pneumoniae included oropharyngeal swab for polymerase chain reaction and culture, as well as acute and convalescent serology by immunoflourescent antibody assay. Laboratory workup for C pneumoniae included oropharyngeal swab for polymerase chain reaction, as well as acute and convalescent serology by microimmunofluorescent antibody assay.
Efficacy
The primary efficacy analysis was the assessment of clinical response in the CPP population at the TOC visit. The clinical response was defined as either cure (signs and symptoms related to the acute infection had resolved, or clinical improvement was such that no additional antibiotics were deemed necessary, and the chest radiograph performed at the TOC visit had either improved or not progressed) or failure (one or more of the following: signs and symptoms related to the acute infection had persisted or worsened and additional antibiotics were necessary; new clinical signs and/or symptoms of pneumonia had appeared and additional antibiotics were necessary; radiologic evidence of pneumonia progression during treatment; or death due to pneumonia). In some cases, for instance, when no additional antibiotic was prescribed and some signs or symptoms improved but others did not, a response of cure or failure could not be assigned. In these instances, the sponsor manually reviewed the subject's data and assigned a response prior to unblinding the data.
The bacteriologic response for respiratory pathogens isolated at baseline was based on either TOC culture results or, if a sputum specimen could not be produced at the TOC visit, on the clinical assessment at the TOC visit. The bacteriologic response was defined as eradication (the original pathogen was not identified in the sputum specimen), presumed eradication (subject was not producing sputum and the clinical response was cure), persistence (the original pathogen was still present), and presumed persistence (subject was not producing sputum and the clinical response was failure).
Subjects with a clinical response of cure at the TOC visit were assessed for relapse at a long-term follow-up visit (days 28 to 35). Relapse was defined as either of the following: symptoms related to pneumonia recurred after initial resolution or improvement; new clinical signs or symptoms of pneumonia appeared without documentation of a new pathogen; or the subject received alternate antibiotic therapy for worsening signs or symptoms or reappearance of new signs and symptoms of pneumonia.
Safety
All subjects who received at least one dose of study medication were evaluated for safety, which was assessed by spontaneous reports, physical examination, and laboratory test results. All adverse events, regardless of treatment group or suspected causal relationship to study drug, were recorded. Clinically significant changes in physical examination findings and abnormal laboratory test findings were also recorded as adverse events.
Statistical Analysis
The primary efficacy analysis compared the clinical cure rates for azithromycin microspheres and clarithromycin XL at the TOC visit (days 14 to 21) in the CPP population. Azithromycin microspheres were considered noninferior to clarithromycin XL if the lower boundary of the 95% confidence interval (CI) around the difference in cure rates (azithromycin microspheres--extended-release clarithromycin) was > -10%. The sample size requiring 402 CPP population subjects (201 subjects per arm) was determined based on the following assumptions: 80% power to show noninferiority at the two-sided level of significance; a noninferiority criterion of > -10%; and an assumed clinical cure rate of 85% in both treatment groups. Approximately 504 subjects were to be enrolled to account for an estimated nonevaluability rate of 20%.
Secondary efficacy analyses included the clinical response by baseline pathogen for the BPP population at the TOC visit, and bacteriologic response on a per pathogen basis for the BPP population at the TOC visit. When 95% CIs for the difference in success rates were constructed, the normal approximation to the binomial distribution was used.
RESULTS
A total of 501 subjects were randomized, and 499 were treated (azithromycin microspheres, n = 247; extended-release clarithromycin, n = 252) at 58 centers in seven countries. The numbers of subjects enrolled into the azithromycin microspheres and extended-release clarithromycin study arms, respectively, in each country were as follows: United States, n = 102 and n = 109; Canada, n = 34 and n = 38; Argentina, n = 34 and n = 33; Russia, n = 13 and n = 13; India, n = 32 and n = 31; Estonia, n = 12 and n=13; and Lithuania, n=20 and n=17. Overall, subject demographics were similar in both treatment arms (Table 1). Most subjects were white and had unilobar disease. Slightly over half of the subjects were smokers or ex-smokers.
The CPP population comprised 411 of the 499 treated subjects (82.4%): 202 in the azithromycin microspheres study arm and 209 in the extended-release clarithromycin study arm. Forty-five subjects were excluded from the CPP population in the azithromycin microspheres study arm (13 with insufficient signs and symptoms of CAP, 8 with no radiographic evidence of CAP, 23 with no TOC visit, and 1 who received another antibiotic). In the extended-release clarithromycin study arm, 43 subjects were excluded from the CPP population (10 with insufficient signs and symptoms of CAP, 8 with no radiographic evidence of CAP, and 25 with no TOC visit). The CPP clinical response at the TOC visit was 92.6% for azithromycin microspheres and 94.7% for extended-release clarithromycin (95% CI, -6.9 to 2.6) [Table 2]. The lower boundary of the 95% CI around the difference in cure rates (azithromycin microspheres- extended-release clarithromycin) was > -10%, demonstrating that azithromycin microspheres was as effective as extended-release clarithromycin.
At the long-term follow-up visit (days 28 to 35), only one subject (0.6%) in the azithromycin microspheres study arm and five subjects (2.8%) in the extended-release clarithromycin study arm were classified as having relapsed (Table 2). The clinical response rates for azithromycin microspheres and extended-release clarithromycin at the TOC visit were comparable in all subject populations studied (Table 3).
Overall, there were little differences in clinical cure rates between treatment groups by gender, age, or race in the CPP population. Clinical cure rates for azithromycin microspheres were 95.7% and 92.2% in subjects aged [greater than or equal to] 65 years old and < 65 years old, respectively, while those for extended-release clarithromycin were 94.7% in both populations. There were little differences between treatment groups in the clinical cure rate according to the extent of pneumonia, vaccination history, or history of diabetes. Subjects with multilobar pneumonia had a clinical cure rate of 88.5%, as compared with 94.4% in all subjects with unilobar pneumonia, indicating that most subjects with more extensive pneumonia were also successfully cured. In the other subject populations, clinical response by the various prognostic factors was similar to that of the CPP population.
Of the 499 subjects treated, 281 subjects (56%) had a pathogen identified at baseline: 201 subjects (40%) had a single pathogen and 80 subjects (16%) had multiple pathogens. At baseline, 122 subjects (24%) had an atypical pathogen identified: 59 subjects (24%) in the azithromycin microspheres group and 63 subjects (25%) in the extended-release clarithromycin group. In the all-treated population, 22 subjects (9%) in the azithromycin microspheres group and 33 subjects (13%) in the extended-release clarithromycin group had both an atypical and typical pathogen isolated at baseline. Of the 56 isolates of S pneumoniae isolated at baseline, 49 isolates (87.5%) were considered azithromycin susceptible, 1 isolate (1.7%) was intermediate, and 6 isolates (10.7%) were azithromycin resistant; 6 of these isolates (10.7%) were also considered resistant to clarithromycin.
Table 4 shows the clinical response for selected baseline pathogens. Cure rates were comparable between the two regimens for both typical and atypical pathogens. Overall pathogen eradication rates were similar for azithromycin microspheres (91.8%; 123 of 134 subjects) and extended-release clarithromycin (90.5%; 153 of 169 subjects), although most bacteriologic responses were based on clinical response (ie, presumed eradication) rather than on follow-up culture results.
Of the seven azithromycin-nonsusceptible S pneumoniae isolates, two were collected from subjects in the azithromycin microspheres treatment group (Table 5). Both isolates had azithromycin MICs of 4 [micro]g/mL. One subject was considered a clinical cure, while the other was considered a failure; the subject who was a failure had two other copathogens identified in the baseline sputum culture. Of the six clarithromycin-resistant S pneumoniae isolates, four were collected from subjects in the extended-release clarithromycin treatment group (Table 6). Two subjects were considered cures, and two subjects were considered clinical failures.
There was one subject in the clarithromycin treatment group who had a baseline sputum culture positive for S pneumoniae that was of intermediate susceptibility to azithromycin (MIC = 1 [micro]g/mL) and susceptible to clarithromycin (MIC = 0.25 [micro]g/mL). The isolate tested negative for both the mef and ermB genes, suggesting that resistance, in this instance, may have been conferred by a point mutation. This subject had a clinical response of cure.
There were three clinical failures associated with intermediate-resistant and resistant pathogens other than S pneumoniae. In the azithromycin microspheres study arm, one subject failed with an azithromycin-resistant Staphylococcus aureus (MIC > 4 [micro]g/mL) and one subject failed with an azithromycin-resistant Klebsiella pneumoniae (MIC > 4 [micro]g/mL). In the extended-release clarithromycin study arm, one subject failed with a clarithromycin-intermediate-resistant H influenzae (MIC = 16 [micro]g/mL).
Due to the single-dose nature of the azithromycin microspheres regimen, 100% of all subjects randomized to receive azithromycin microspheres were compliant with the regimen. In contrast, 15 of 254 subjects (5.9%) randomized to the extended-release clarithromycin study arm did not complete the entire 7-day course of active treatment. As expected, compliance with the dosing schedule over the study duration (active plus placebo) was similar for both treatment groups, ie, a similar number of patients in the azithromycin microspheres group, 20 of 247 patients (8.1%), were noncompliant with placebo treatment during the 6-day placebo period.
Both agents were well tolerated. Approximately one fourth of the treated subjects in each treatment arm experienced treatment-related adverse events (azithromycin microspheres, 26.3%; extended-release clarithromycin, 24.6%). Table 7 shows the incidence rates of the most common events reported in the azithromycin microspheres and extended-release clarithromycin groups, respectively, including diarrhea/loose stools (12.1% vs 7.5%), nausea (3.6% vs 3.2%), and abdominal pain (3.6% vs 1.2%). A total of 25 azithromycin microspheres subjects (10%) had treatment-related diarrhea, all episodes of which were either mild (n = 16) or moderate (n = 9) in severity. In 13 of the 25 subjects (52%), diarrhea was limited to day 1 or 2 of the study. Most reported adverse events were mild or moderate in severity. For azithromycin microspheres, most adverse events occurred on the day of administration and resolved within a few days. There were no clinically significant changes in clinical laboratory parameters during the study.
One subject in the azithromycin microspheres group discontinued due to a treatment-related adverse event (0.4%, nausea); this occurred on study day 4, when the subject was taking extended-release clarithromycin placebo. Two azithromycin microspheres subjects and one extended-release clarithromycin subject were hospitalized for worsening of pneumonia. Four deaths occurred during the study, one while on study therapy and three after therapy, all in the extended-release clarithromycin study arm. None of the deaths were attributed to study therapy or progression of CAP.
DISCUSSION
The results of this international, multicenter, randomized, double-blind, double-dummy study demonstrate that a single 2.0-g dose of azithromycin microspheres was as effective as extended-release clarithromycin, 1.0 g/d for 7 days, when used to treat adults with mild-to-moderate CAP. The clinical response rates in the CPP population at TOC were similar for the two treatment arms: 92.6% for azithromycin microspheres, and 94.7% for extended-release clarithromycin. Clinical efficacy was maintained at the long-term follow-up visit, with relapse rates of 0.6% and 2.8% in the azithromycin microsphere group and extended-release clarithromycin group, respectively.
Azithromycin microspheres and extended-release clarithromycin were equally effective in eradicating bacterial pathogens; overall pathogen eradication rates were 91.8% for azithromycin microspheres and 90.5% for extended-release clarithromycin. A single dose of azithromycin microspheres demonstrated excellent activity against the key typical bacterial pathogens S pneumoniae, H influenzae, and M catarrhalis, with clinical cure rates [greater than or equal to] 89.5%, and the key atypical bacterial pathogens C pneumoniae and M pneumoniae with clinical cure rates [greater than or equal to] 90.5%.
Outcomes in subjects aged [greater than or equal to] 65 years old were essentially the same as in subjects aged < 65 years old (clinical cure rates in the CPP population were 95.7% and 92.2%, respectively for azithromycin, and 94.7% for clarithromycin in both populations). Similarly, there were no remarkable differences in clinical cure rates by gender or race in the CPP population. The clinical cure rates and pathogen eradication rates achieved in this study are similar to those reported in previous CAP studies comparing a 3-day azithromycin regimen with a 10-day clarithromycin regimen, (15) a 10-day clarithromycin regimen, (26) and a 3-day azithromycin regimen. (27,28)
In this study, slightly over half of the subjects had a pathogen isolated at baseline. This is consistent with the results of other published antibiotic studies (15,29,30) in CAP, which have reported percentages of subjects with baseline pathogens ranging from 31 to 45%.
Both azithromycin microspheres and extended-release clarithromycin were well tolerated, with a similar proportion of patients in each treatment group experiencing treatment-related adverse events. Only two subjects, one in each treatment group, discontinued therapy due to treatment-related adverse events, and no treatment-related serious adverse events were reported. Although the incidence of diarrhea/loose stools was higher in the azithromycin microspheres group, all episodes were mild or moderate in intensity and in 52% of subjects the symptoms were limited to days 1 and 2.
Compliance with active treatment in azithromycin microspheres study arm was 100%, compared with 94% for the 7-day clarithromycin regimen, suggesting that the shorter the dosing schedule, the more likely subjects were to complete the full course of treatment. Evidence indicates that patient compliance with antibiotic therapy for respiratory tract infections worsens as the number of daily doses and the duration of the treatment regimen increase. (31) Noncompliance with therapy may be associated with treatment failure, deterioration in the patient's condition, and increased use and cost of health-care resources, such as the requirement for additional drugs and hospital admission. (31)
Improved compliance may also reduce the emergence of resistant strains. (32) This is reflected in the recent US Food and Drug Administration labeling for systemic antibiotics, which advise that skipping doses or not completing the full course of therapy may decrease the effectiveness of the treatment and increase the likelihood that bacteria will develop resistance. (33) Single-dose antibiotic therapy helps maximize patient compliance and may therefore reduce the likelihood of treatment failures and the emergence of resistant pathogens.
Another compliance-related advantage of single-dose therapy with azithromycin microspheres is the potential for use as directly observed therapy. This option may be valuable in the clinic or emergency department, where compliance may be in doubt or barriers to filling prescriptions may exist.
In conclusion, the results of this study demonstrate that a single 2.0-g dose of azithromycin microspheres was as effective and well tolerated as extended-release clarithromycin, 1.0 g/d for 7 days, for the treatment of mild-to-moderate CAP in adults. The results from this study demonstrate that the azithromycin microspheres formulation is an appropriate therapy for mild-to-moderate CAP.
ACKNOWLEDGMENT: The authors thank Jennifer Garner for providing statistical support for this study.
This clinical trial was funded by Pfizer Inc. Dr. Lewis and Dr. Breen are employed by Pfizer Inc. Dr. Drehobl and Dr. De Salvo participated as lead investigators in the trial.
Manuscript received December 15, 2004; revision accepted March 23, 2005.
REFERENCES
(1) National Center for Health Statistics. Third National Health and Nutrition Examination Survey, 1988-1994. Washington, DC: US Department of Health and Human Services, 1995
(2) Mandell LA, Niederman N. The Canadian Community-acquired Pneumonia Consensus Group. Antimicrobial treatment of community-acquired pneumonia in adults: a conference report. Can J Infect Dis 1993; 4:25-28
(3) Tsirgiotis E, Ruffin R. Community acquired pneumonia: a perspective for general practice. Aust Fam Physician 2000; 29:639-645
(4) Mandell LA, Marrie TJ, Grossman RF, et al. Canadian guidelines for the initial management of community-acquired pneumonia: an evidence-based update by the Canadian Infectious Diseases Society and the Canadian Thoracic Society. Clin Infect Dis 2000; 31:383-421
(5) Bartlett JG, Breiman RF, Mandell LA, et al. Community-acquired pneumonia in adults: guidelines for management. Clin Infect Dis 1998; 26:811-838
(6) Kuti JL, Capitano B, Nicolau DP. Cost-effective approaches to the treatment of community-acquired pneumonia. Pharmacoeconomics 2002; 20:513-528
(7) Niederman MS, McCombs JS, Under AN, et al. The cost of treating community-acquired pneumonia. Clin Ther 1998; 20:820-837
(8) Bartlett JG, Dowell SF, Mandell LA, et al. Practice guidelines for the management of community-acquired pneumonia in adults. Infectious Diseases Society of America. Clin Infect Dis 2000; 31:347-382
(9) Marston BJ, Plouffe JF, File TM Jr, et al. Incidence of community-acquired pneumonia requiring hospitalization: results of a population-based active surveillance study in Ohio. Arch Intern Med 1997; 157:1709-1718
(10) Niederman MS, Mandell LA, Anzueto A, et al. Guidelines for the management of adults with community-acquired pneumonia: diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med 2001; 163:1730-1754
(11) Bernstein JM. Treatment of community-acquired pneumonia: IDSA guidelines. Chest 1999; 115(suppl):9S-13S
(12) Mandell LA. Community-acquired pneumonia: etiology, epidemiology, and treatment. Chest 1995; 108(suppl):S35-S42
(13) Mandell LA, Bartlett JG, Dowell SF, et al. Update of practice guidelines for the management of community-acquired pneumonia in immunocompetent adults. Clin Infect Dis 2003; 37:1405-1433
(14) Hoepelman IM, Mollers MJ, van Schie MH, et al. A short (3-day) course of azithromycin tablets versus a 10-day course of amoxicillin-clavulanic acid (co-amoxiclav) in the treatment of adults with lower respiratory tract infections and effects on long-term outcome. Int J Antimicrob Agents 1998; 9:141-146
(15) O'Doherty B, Muller O. Randomized, multicentre study of the efficacy and tolerance of azithromycin versus clarithromycin in the treatment of adults with mild to moderate community acquired pneumonia. Azithromycin Study Group. Eur J Clin Microbiol Infect Dis 1998; 17:828-833
(16) Schentag JJ, Ballow CH. Tissue-directed pharmacokinetics. Am J Med 1991; 91(suppl 3A):5S-11S
(17) Baldwin DR, Wise R, Andrews JM, et al. Azithromycin concentrations at the sites of pulmonary infection. Eur Respir J 1990; 3:886-890
(18) Mandell GL. Delivery of antibiotics by phagocytes. Clin Infect Dis 1994; 19:922-925
(19) Rapp RP. Pharmacokinetics and pharmacodynamics of intravenous and oral azithromycin: enhanced tissue activity and minimal drug interactions. Ann Pharmacother 1998; 32:785-793
(20) Rothermel CD. Single-dose azithromycin for acute otitis media: a pharmacokinetic/pharmacodynamic rationale. Curr Ther Res 2003; 64(suppl A):A4-A15
(21) Craig WA. Postantibiotic effects and the dosing of macrolides, azalides, and streptogramins. In: Zinner SH, Young LS, Acar JF, eds. Expanding indications for the new macrolides, azalides and streptogramins. New York, NY: Marcel Dekker, 1997; 27-38
(22) Babl FE, Pelton SI, Li Z. Experimental acute otitis media due to non-typeable Haemophilus influenzae: comparison of high and low azithromycin doses with placebo. Antimicrob Agents Chemother 2002; 46:2194-2199
(23) Girard D, Finegan SM, Cimochowski CR, et al. Accelerated dosing of azithromycin in preclinical infection models. Presented as the 102nd American Society for Microbiology General Meeting, May 19-23, 2002, Orlando, FL; abstract A-57
(24) Kamicker BJ, Bertsche CD, Medina IA. In rodent models, a single dose of azithromycin was more effective than dosing split over 3 or 5 days. Presented at the 44th annual meeting of Interscience Conference on Antimicrobial Agents and Chemotherapy, October 30 to November 2, 2004, Washington, DC; abstract B-1181
(25) Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 1997; 336:243-250
(26) Mathers DL, Hassman J, Tellier G. Efficacy and tolerability of once-daily oral telithromycin compared with clarithromycin for the treatment of community-acquired pneumonia in adults. Clin Ther 2004; 26:48-62
(27) Myburgh J, Nagel GJ, Petschel E. The efficacy and tolerance of a three-day course of azithromycin in the treatment of community-acquired pneumonia. J Antimicrob Chemother 1993; 31(supp1 E):163-169
(28) Uzun O, Hayran M, Akova M, et al. Efficacy of a three-day course of azithromycin in the treatment of community-acquired pneumococcal pneumonia: preliminary report. J Chemother 1994; 6:53--57
(29) File TM, Schlemmer B, Garau J, et al. Efficacy and safety of gemifloxacin in the treatment of community-acquired pneumonia: a randomized, double-blind comparison with trovafloxacin. J Antimicrob Chemother 2001; 48:67-74
(30) O'Doherty B, Dutchman DA, Pettit R, et al. Randomized, double-blind, comparative study of grepafloxacin and amoxycillin in the treatment of patients with community-acquired pneumonia. J Anfimicrob Chemother 1997; 40(suppl A): 73-81
(31) Kardas P. Patient compliance with antibiotic treatment for respiratory tract infections. J Antimicrob Chemother 2002; 49:897-903
(32) Pichichero ME. Short course antibiotic therapy for respiratory infections: a review of the evidence. Pediatr Infect Dis J 2000; 19:929-937
(33) U.S. Food and Drug Administration. Labeling requirements for systemic antibacterial drug products intended for human use. Available at: www.fda.gov/oc/opacom/hottopics/anti_ resist.html. Accessed June 28, 2004
Margaret A. Drehobl, MD; Maria C. De Salvo, MD; Drew E. Lewis, MD; and Jeanne D. Breen, MD
* From the Scripps Clinic-Clinical Research (Dr. Drehobl), San Diego, CA; Division Neumotisiologia (Dr. De Salvo), Hospital General de Agudos "Dr. E. Tornu," Buenos Aires, Argentina; and Pfizer Global Research and Development (Drs. Lewis and Breen), Pfizer Inc., New London, CT.
Correspondence to: Drew E. Lewis, MD, Pfizer Global Research and Development, 50 Pequot Ave, New London, CT 06320
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group