Gaucher's disease is an uncommon familial disorder characterized by deficiency of beta-glucosidase, a lysosomal enzyme responsible for the degradation of glucosyl ceramide (glucocerebroside). This biochemical defect leads to glucocerebroside-laden histiocytes (Gaucher cells) which assume distinctive morphologic features in systemic organs. Deposits of Gaucher cells typically accumulate in the spleen, liver, bone marrow, lymph nodes, and in some cases, the brain and lung.[1] While Gaucher cells may infiltrate the lung and extramedullary hematopoiesis invariably involves the spleen and liver, intrathoracic extramedullary hematopoiesis has not been previously described in Gaucher's disease.
CASE REPORT
A 74-year-old woman presented with a one-month history of dry cough recently productive of a small amount of white sputum. She denied fever, chills, weight loss, and dyspnea. Gaucher's disease had been diagnosed on bone marrow aspirate ten years earlier when she presented with a prolonged bleeding time, thrombocytopenia, and purpura. She had no other signs or symptoms referable to this disorder except for transient elevation of liver enzymes and mild splenomegaly discovered 2 years prior. Other past medical history included stage la ovarian adenocarcinoma 11 years earlier, without evidence of recurrence following hysterectomy and bilateral salpingooophorectomy.
Physical examination revealed a well-appearing woman with normal vital signs and in no apparent discomfort. The lung examination was normal, and there was no detectable lymphadenopathy or abdominal organomegaly. Examination of her skin disclosed a few purpuric lesions and petechiae.
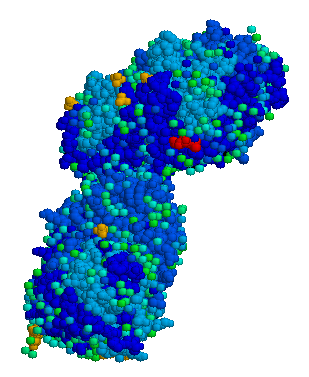
Laboratory data including hematocrit value, erythrocyte indices, and morphologic findings, white blood cell and platelet counts, and liver enzyme levels were within the normal range. Pulmonary function tests showed mild reversible airway dysfunction but normal lung volumes and diffusing capacity for carbon monoxide. The chest radiograph showed a new, discrete 2-cm paraspinal mass at the level of the ninth thoracic vertebra which was confirmed by computed tomography (Fig 1). No parenchymal lung disease or lymphadenopathy was present. Percutaneous computed tomography-guided fine needle aspiration of the paravertebral mass showed Gaucher cells as well as megakaryocytes and immature red blood cells, findings representing extramedullary hematopoiesis (Fig 2). The patient's cough responded to inhaled bronchodilators.
DISCUSSION
Gaucher's disease is an inborn error of metabolism with several genetically distinct clinical types. At least three forms are described,[2] and all may demonstrate lung parenchymal abnormalities. The adult form (type 1, chronic nonneuronopathic type) may present in infancy or adulthood, typically showing anemia, thrombocytopenia, splenomegaly, and bone lesions. Although somewhat variable, the course is relatively benign. The present case depicts this form. The rarer infantile form (type 2, acute neuronopathic type) is malignant, demonstrating progressive neurologic symptoms and death from respiratory infection by age 2 years. An intermediate juvenile form (type 3, subacute neuronopathic type) consists of a heterogeneous patient group demonstrating reticuloendothelial involvement as well as progressive neurologic deterioration characteristic of the infantile form. This type also exhibits an aggressive course resulting in hepatosplenomegaly and early death.
Intrathoracic Gaucher's disease typically affects the lung and is characterized histologically by extensive infiltration of interlobular septa, alveolar spaces, and terminal bronchioles by iron-laden Gaucher cells. It correlates roentgenographically with a diffuse reticulonodular or miliary parenchymal pattern.[3,4] The diffuse pulmonary infiltration, absent in the present case, affects a small minority of patients. We could find no documentation in the literature of a discrete intrathoracic mass due to Gaucher's disease, except for a single case of mediastinal lymph node enlargement.[5]
Intrathoracic extramedullary hematopoiesis causing a round or lobulated posterior mediastinal mass is uncommon, having only 35 cases in the literature as of 1985.[6] occurs as a compensatory response to disruption of normal bone marrow function. The overwhelming majority are related to destruction of erythrocytes (eg, hereditary spherocytosis, thalassemia, congenital hemolytic anemia, sickle cell anemia) or bone marrow insufficiency (eg, myelofibrosis, carcinomatosis, or lymphomatosis of bone marrow). Such cases are often but not always associated with splenomegaly and hypersplenism. This patient's presentation is atypical because of a normal hematocrit value and red blood cell morphologic findings.
The presence of intrathoracic extramedullary hematopoiesis should be suspected in a patient with known Gaucher's disease who has a thoracic paravertebral mass. Although such masses usually are asymptomatic, paraplegia due to cord compression by paravertebral extramedullary hematopoiesis from other etiologies has been reported. In the proper clinical setting, a combination of noninvasive imaging modalities, including computed tomography, radionuclide scanning,[7] or magnetic resonance imaging,[6] or all three, may be definitive in the diagnosis of intrathoracic extramedullary hematopoiesis. In difficult cases, however, tissue biopsy or aspiration is confirmatory.
REFERENCES
[1] Lee RE, Peters SP, Glew RH. Gaucher's disease: clinical, morphologic, and pathogenetic considerations. Pathol Annu 1977; 2:309-39 [2] Kolodny EH. Gaucher disease. In: Wyngaarden JB, Smith LH, Bennett JC, eds. Cecil textbook of medicine. 19th ed. Philadelphia: WB Saunders, 1992; 1091-93 [3] Schneider EL, Epstein CJ, Kaback MJ, Brandes D. Severe pulmonary involvement in adult Gaucher's disease: report of three cases and review of the literature. Am J Med 1977; 63:475-80 [4] Fisher MR, Sider L. Roentgenogram of the month: diffuse reticulonodular infiltrate associated with splenomegaly. Chest 1983; 84:609-10 [5] Myers B. Gaucher's disease of lungs. Br Med J 1937; 2:8-10 [6] Savader SJ, Otero RR, Savader BL. M R imaging of intrathoracic extramedullary hematopoiesis. J Comput Assist Tomogr 1988; 12:878-80 [7] Adams BK, Smuts NA. The detection of extramedullary hematopoiesis in a patient with osteopetrosis. Eur J Nucl Med 1989; 15:803-04 (*) From Department of Radiology (Drs. Ch'en and Lynch), Pathology (Dr. Shroyer), and Division of Pulmonary Sciences and Critical Care Medicine (Dr. Schwarz), University of Colorado Health Sciences Center, Denver.
COPYRIGHT 1993 American College of Chest Physicians
COPYRIGHT 2004 Gale Group