Definition
Urinary anti-infectives are medicines used to treat or prevent infections of the urinary tract--the passage through which urine flows from the kidneys out of the body.
Purpose
Normally, no bacteria or other disease-causing organisms live in the bladder. Likewise, the urethra--the tube-like structure that carries urine from the bladder out of the body--usually has either no bacteria or not enough to cause problems. But the bladder, urethra, and other parts of the urinary tract may become infected when disease-causing organisms invade from other body regions or from outside the body. Urinary anti-infectives are used to treat such infections or to prevent them in people who get them often.
Description
Commonly used urinary anti-infectives include methenamine (Urex, Hiprex, Mandelamine), nalidixic acid (NegGram) and nitrofurantoin (Macrobid, Furatoin, and other brands). These medicines are available only with a physician's prescription and come in capsule, tablet, granule, and liquid forms.
Recommended dosage
Methenamine
For adults and children 12 years and over, the usual dosage is 1 gram, taken either twice a day or four times a day, depending on the form in which the drug comes. For children aged 6-12 years, the dosage ranges from 500 mg taken 2-4 times a day to 1 gram taken twice a day, again depending on the form of the drug. For children under 6 years, a physician must determine the dose.
This medicine will not work properly unless the urine is acidic, with a pH reading of 5.5 or below. The physician who prescribes the medicine will explain how to test the urine's acidity. The physician also may suggest diet changes that will make the urine more acidic, such as eating more protein, drinking cranberry juice, eating plums and prunes, but avoiding most other fruits, and cutting down on milk and other dairy products. Antacids also should be avoided.
Nalidixic acid
The recommended dosage for adults and children 12 years and older is 1 gram every 6 hours. If the medicine is taken for more than one or two weeks, the dosage may be decreased to 500 mg every 6 hours. A physician must determine the correct dosage for children 3 months to 12 years old. Children under 3 months should not take this medicine because it causes bone problems in young animals and could have the same effect in young children.
Nitrofurantoin
Capsules, tablets, or liquid
The usual dose for adults and teenagers is 50-100 mg every six hours.
Extended-release capsules
For adults and children 12 years and older, the usual dosage is 100 mg every 12 hours for 7 days.
For all forms of nitrofurantoin, a physician must determine the correct dose for children 1 month and older, based on the child's body weight. Children under 1 month should not take this medicine.
Precautions
Methenamine
People with certain medical conditions may have problems if they take this medicine. For example, people with severe liver disease may have worsened symptoms of their disease. And people who are dehydrated or who have severe kidney disease may be more likely to have side effects that affect the kidneys.
Nalidixic acid
Some people feel drowsy, dizzy, or less alert than usual when using this drug. The medicine may also cause blurred vision or other vision changes. Because of these possible problems, anyone who takes nalidixic acid should not drive, operate machinery, or do anything else that might be dangerous until they have found out how the drugs affect them.
Nalidixic acid may increase sensitivity to sunlight. Even brief exposure to sun can cause a severe sunburn or a rash. While being treated with this medicine, avoid being in direct sunlight, especially between 10 a.m. and 3 p.m.; wear a hat and tightly woven clothing that covers the arms and legs; use a sunscreen with a skin protection factor (SPF) of at least 15; protect the lips with a sun block lipstick; and do not use tanning beds, tanning booths, or sunlamps.
Diabetic patients should be aware that this medicine may cause false results on some urine sugar tests. Check with a physician before making any changes in diet or diabetes medicine based on the results of a urine test.
In laboratory studies, nalidixic acid interferes with bone development in young animals. The drug's effects have not been studied in pregnant women, but because of its effects in animals, it is not recommended for use during pregnancy.
This medicine generally does not cause problems in nursing babies whose mothers take it. However, nursing babies with glucose-6-phosphate dehydrogenase (G6PD) deficiency (an inherited disorder that affects mainly black males) may have blood problems if their mothers take nalidixic acid.
People with certain medical conditions may be more likely to have particular side effects if they take this medicine. For example, people with a history of seizures or severe hardening of the arteries in the brain may be more likely to have side effects that affect the nervous system. People with glucose-6-phosphate dehydrogenase (G6PD) deficiency are more likely to have side effects that affect the blood. Also, people with liver disease or severe kidney disease have an increased chance of having any of the drug's possible side effects.
Nitrofurantoin
Pregnant women should not take this medicine within 2 weeks of their delivery date and should not use it during labor and delivery, as this could cause problems in the baby.
Women who are breastfeeding should check with their physicians before using this medicine. It passes into breast milk and could cause problems in nursing babies whose mothers take it. This is especially true of babies with glucose-6-phosphate dehydrogenase (G6PD) deficiency. The medicine also should not be given directly to babies up to 1 month of age, as they are particularly sensitive to its effects.
Older people may be more likely to have side effects when taking nitrofurantoin, because they are more sensitive to the drug's effects.
Taking nitrofurantoin may cause problems for people with certain medical conditions. Side effects may be greater, for example, in people with lung disease or nerve damage. In people with kidney disease, the medicine may not work as well as it should, but may cause more side effects. Those with glucose-6-phosphate dehydrogenase (G6PD) deficiency who take nitrofurantoin may develop anemia.
Diabetic patients should be aware that this medicine may cause false results on some urine sugar tests. They should check with a physician before making any changes in diet or diabetes medicine based on the results of a urine test.
General precautions for all urinary anti-infectives
Symptoms should improve within a few days of starting to take a urinary anti-infective. If they do not, or if they become worse, check with a physician right away. Patients who need to take this medicine for long periods should see their physicians regularly, so that the physician can check their progress.
Anyone who has had unusual reactions to urinary anti-infectives in the past should let his or her physician know before taking the drugs again. The physician should also be told about any allergies to foods, dyes, preservatives, or other substances. Patients taking nalidixic acid should tell their physicians if they have ever had reactions to related medicines such as cinoxacin (Cinobac), ciprofloxacin (Cipro), enoxacin (Penetrex), norfloxacin (Noroxin) or ofloxacin (Floxin), all of which are also used to treat or prevent infections. Anyone taking nitrofurantoin should let the physician know if he or she has had an unusual reaction to medicines such as furazolidone (Furoxone) or nitrofurazone (Furacin).
Side effects
Methenamine
Nausea and vomiting are not common but may occur. These side effects do not need medical attention unless they are severe. One side effect that should be brought to a physician's attention immediately is a skin rash.
Nalidixic acid
Some side effects are fairly minor and are likely to go away as the body adjusts to the drug. These include dizziness, drowsiness, headache, nausea or vomiting, stomach pain and diarrhea. Unless these problems continue or are bothersome, they do not need medical attention.
Other side effects, however, should have prompt medical attention. Anyone who has changes in vision, such as blurred vision, double vision, decreased vision, changes in color vision, halos around lights, or notices an excessive brightness of lights should check with a physician immediately.
Nitrofurantoin
This medicine may make the urine turn reddish-yellow to brown. This is nothing to worry about. Other possible side effects that do not need medical attention unless they are severe include pain in the stomach or abdomen, stomach upset, diarrhea, loss of appetite, and nausea or vomiting.
Anyone who has chest pain, breathing problems, fever, chills, or a cough while taking nitrofurantoin should check with a physician immediately.
General advice on side effects for all urinary anti-infectives
Other side effects are possible when taking any urinary anti-infective. Anyone who has unusual symptoms while taking this type of medicine should get in touch with his or her physician.
Interactions
Methenamine
Certain medicines may make methenamine less effective. These include thiazide diuretics (water pills) and medicines that make the urine less acid, such as antacids, bicarbonate of soda, and the drugs acetazolamide (Diamox), dichlorphenamide (Daranide), and methazolamide (Neptazane), which are used to treat glaucoma, epilepsy, altitude sickness, and other conditions.
Nalidixic acid
People who are taking blood thinners (anticoagulants) may be more likely to have bleeding problems if they take this medicine.
Nitrofurantoin
Nitrofurantoin may interact with many other medicines. For example, taking nitrofurantoin with certain drugs that include methyldopa (Aldomet), sulfonamides (sulfa drugs), vitamin K, and diabetes medicines taken by mouth may increase the chance of side effects that affect the blood. General side effects are more likely in people who take nitrofurantoin with the gout drugs probenecid (Benemid) or sulfinpyrazone (Anturane). And the risk of side effects that involve the nervous system is higher in people who take nitrofurantoin with various drugs including lithium (Lithane), disulfiram (Antabuse), other anti-infectives, and the cancer drugs cisplatin (Platinol) and vincristine (Oncovin). Patients who have had a DPT (diphtheria, tetanus, and pertussis) vaccine within the last 30 days or who have one after taking nitrofurantoin are also more likely to have side effects that affect the nervous system. Because of the many possible interactions, anyone taking nitrofurantoin should be sure to check with a physician before combining it with any other medicine.
General advice about interactions
Not every drug that may interact with a urinary anti-infective is listed here. Be sure to check with a physician or pharmacist before combining a urinary anti-infective with any other prescription or nonprescription (over-the-counter) medicine.
Key Terms
- Altitude sickness
- A set of symptoms that people who normally live at low altitudes may have when they travel to high altitudes. The symptoms include nosebleed, nausea, and shortness of breath.
- Anemia
- A lack of hemoglobin--the compound in blood that carries oxygen from the lungs throughout the body and brings waste carbon dioxide from the cells to the lungs, where it is released.
- Bacteria
- Tiny, one-celled forms of life that cause many diseases and infections.
- Glaucoma
- A condition in which pressure in the eye is abnormally high. If not treated, glaucoma may lead to blindness.
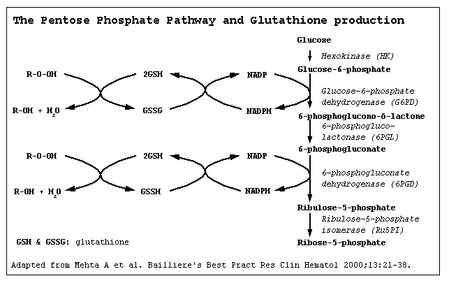
- Glucose-6-phosphate dehydrogenase (G6PD) deficiency
- An inherited disorder in which the body lacks an enzyme that normally protects red blood cells from toxic chemicals. When people with this condition take certain drugs, their red blood cells break down, causing anemia. This may also happen when they have a fever or an infection. The condition usually occurs in males. About 10% of black males have it, as do a small percentage of people from the Mediterranean region.
- Granule
- A small grain or pellet. Medicines that come in granule form usually are mixed with liquids or sprinkled on food before they are taken.
- Organism
- An individual of some type of life form, such as a plant or an animal.
- pH
- A measure of how acidic or alkaline something is. The pH scale ranges from 0 to 14. Values below 7 are acidic; values above 7 are alkaline.
- Seizure
- A sudden attack, spasm, or convulsion.
Further Reading
For Your Information
Periodicals
- Tucker, M. Susan. "Recurrent UTI: Who Should Treat Herself?" Patient Care 26 (July 15, 1992): 259.
Gale Encyclopedia of Medicine. Gale Research, 1999.