A harmless virus used as a delivery vehicle may help set a roadblock for a potentially catastrophic outbreak of bird flu in humans, assert researchers at Purdue University, West Lafayette, Ind., and the Centers for Disease Control and Prevention, Atlanta.
Purdue molecular virologist Suresh Mittal and his collaborators are investigating a new way to provide immunity against avian influenza viruses, or bird flu, the most lethal of which, H5N1, has a 50% fatality rate in humans.
The researchers are focusing on using a harmless virus, called adenovirus, as a transmitting agent for a vaccine to fight off highly virulent strains of the avian influenza viruses. Current vaccines are designed for strains of flu found in local areas and are effective only as long as the virus does not change form. Existing vaccines will have limited success against new strains of avian influenza. Every time a bird flu mutates, vaccines must be redesigned.
Another advantage to using an adenovirus as a vector, or transporter of vaccine into cells, is that it could be mass produced much more quickly than with current models. "Our approach is to use an adenovirus to deliver some components of the bird flu virus in a vaccine formulation," Mittal explains. "We already know how to grow large amounts of adenovirus and how to purify it because adenoviruses already are used in clinical trials for gene therapy as vectors. The ultimate goal of our research is to develop an effective avian influenza virus vaccine that will provide long-lasting and broad immunity against multiple strains of this virus."
The proteins that form the basis for all of today's flu vaccines are grown in fertilized chicken eggs. It takes months to produce a vaccine for a new virus strain using this method and limits supplies due to shortages in eggs for that purpose. The egg production method also creates difficulty in redesigning the vaccine to keep pace with virus mutations.
"Do we still want to depend on the egg to make our flu vaccines?" Mittal wonders. "When these types of viruses strike humans, they also strike poultry. In that case, the availability of fertilized eggs to make enough vaccine will be compromised."
A "medium-level" bird flu pandemic in the U.S. would kill between 90200,000 people with another 20-47,000,000 sickened, CDC experts estimate. The economic impact alone would be between $71-166,500,000,000. Influenza viruses are respiratory pathogens responsible for widespread infections in humans, a variety of birds, marine mammals, pigs, and horses. In Southeast Asia, millions of poultry have died or been euthanized because of H5N1 avian influenza.
Before the human cases of H5N1, there were no known instances of bird-to-human transmission that led to significant disease, Mittal reveals. However, this type of flu already has passed from poultry to people who had direct contact with iii birds or their feces, saliva, or nasal mucous. A few cases have been documented of human-to-human infection, reports the World Health Organization.
In addition, migratory waterfowl at China's Qinghai Lake Nature Reserve have succumbed to H5N1. While migratory birds often can pass avian influenza to other animals, they generally do not become iii. Scientists from the U.S. Geological Survey National Wildlife Health Center believe this is further evidence that H5N1 could trigger a human flu pandemic.
Since 2003, about 60 people have died in Southeast Asia from H5N1, around half of those afflicted. Outbreaks in birds have been confirmed in 11 countries, and the disease is spreading north into regions outside of Southeast Asia and already has been reported in Russia. The disease's spread, occurrences of other bird flu types, and the already confirmed human cases provide added impetus for finding more effective vaccine protection, Mittal asserts. The CDC reported two human cases of another bird flu in the U.S. in recent years--H7N2 in Virginia (2002) and New York (2003).
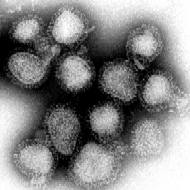
Viruses are classified according to the combination of two types of proteins found on the virus cell surface. The 15 types of hemagglutinin (H) protein and nine types of neuraminidase (N) protein form a large number of influenza viruses for which birds are the natural hosts. New, often more dangerous flu strains develop when the H and N combinations change. When the genes of a human or swine influenza mix with an avian variety, a highly pathogenic human flu likely will result.
These virus alterations work a bit like a jigsaw puzzle: As two viruses grow in the same animal, they replicate and reassemble their genome. If one virus takes a piece of genome from the other virus to fill an empty spot, then a new virus is born. The potential for a pandemic exists when one of these new viruses is introduced into the human population. People with no previous exposure to this new flu strain have little or no immunity, making them highly susceptible to a virus that now easily can spread from person to person.
The last pandemic was 1968-69 when 34,000 Americans died of the Hong Kong flu (H3N2), a disease still circulating. In 1957-58, Asian flu (H2N2) killed 70,000 people in the U.S. The worst flu pandemic was in 1918-19, when Spanish flu (H1N1) was fatal to 500,000 in the U.S. and as many as 50,000,000 worldwide. Unlike other influenza outbreaks, the origin of that virus remains unknown.
Scientists believe that without the right vaccines and preparation, H5N1 has the potential to be one of the deadliest flu outbreaks if it mutates to human-to-human transmission. This flu strain was first identified in South Africa in 1961, with the first bird-to-human case recorded in 1997. "Many people believe that this virus will mutate and become more widespread," Mittal warns. "The question is when? Are we prepared? We hope that successful completion of this project will result in development of an adenovirus-based vaccine effective against pathogenic avian influenza viruses."
COPYRIGHT 2005 Society for the Advancement of Education
COPYRIGHT 2006 Gale Group