Severe metabolic abnormalities can sometimes create confusing and grossly abnormal electrocardiogram (ECG) recordings. In this case study, a man who had diabetic ketoacidosis and acute renal failure with severe hyperkalemia had an unusual cardiac rhythm strip recording. A subsequent 12-lead ECG showed findings compatible with an acute myocardial infarction of the anterior wall. An ECG obtained after aggressive treatment of the metabolic disorders had a more normal pattern.
Severe metabolic abnormalities can create grossly abnormal ECG readings.
Scenario
Mr B, a 60-year-old man, came to the emergency department because he had had severe pain and coolness of the left lower extremity for 6 hours. He had experienced some pain in the extremity for the previous 6 months and was being treated medically. Examination in the emergency department revealed loss of pulses and findings suggest an embolus in the left iliac vein. Mr B was sent to the operating room, where he underwent emergency bilateral external iliac vein embolectomy. On arrival in the critical care unit, he was lethargic and had Kussmaul respirations. His medical and surgical history included hypertension, type I diabetes mellitus, amputation of the right leg above the knee, and a distal aorta to left femoral artery bypass graft. As a means to assist in interpretation of the cardiac rhythm strip, a 12-lead ECG (Figure 1) was obtained.
[FIGURE 1 OMITTED]
Interpretation
P waves could not be discerned on the first 12-lead ECG. The cardiac rhythm was interpreted as possible accelerated junctional rhythm. The anterior leads showed ST-segment elevation in leads [V.sub.1] and [V.sub.2] and ST-segment depression in leads I, aVL, and [V.sub.4] through [V.sub.6]. Ischemic changes of ST-segment and T-wave inversion were noted in the inferior wall leads. The QRS complex was widened to 0.12 s as a result of hyperkalemia due to diabetic ketoacidosis and rhabdomyolysis with acute anuric renal failure. An ECG (Figure 2) obtained after treatment of the hyperkalemia showed first-degree atrioventricular block as evidenced by a PR interval of 0.24 s, narrowing of the QRS complex to 0.08 s, and the presence of peaked T waves in leads [V.sub.1] through [V.sub.3] The peaked T waves were consistent with the continued hyperkalemia.
[FIGURE 2 OMITTED]
Although findings on an initial ECG were suggestive of an acute anterior wall myocardial infarction, the findings on an ECG obtained after aggressive treatment of the metabolic disorders were normal.
Rationale
In diabetic ketoacidosis, potassium ions shift from the intracellular fluid to the extracellular fluid in response to the influx of the excess hydrogen ions into the cell. Diabetic ketoacidosis occurs as a result of a physiological stressor to the body, which can have a variety of causes, resulting in an increased need for insulin. In Mr B, the physiological stressor was the acute vascular occlusion, resulting in tissue ischemia and necrosis, and subsequent surgical intervention. Insulin is required to facilitate the transport of glucose into the cell for energy or storage and to decrease the production of glucose by the liver. (1)
Because of the loss of blood flow to Mr B's extremities, severe muscle ischemia developed that led to profound muscle necrosis and the massive release of myoglobin, creatine kinase, cellular contents, and other serum enzymes into the bloodstream. As a result of the massive release of enzymes, Mr B experienced acute anuric renal failure, which also contributed to his metabolic acidosis and hyperkalemia. (2)
Medical Management
Once the laboratory report of the critically elevated serum level of potassium (see Table) was received, multiple treatments were started. The immediate goal was to cause a rapid shift of potassium from the extracellular fluid back into the intracellular fluid. The purpose of the rapid shift is to facilitate excretion of the potassium to reestablish a normal serum level. First-line medications included 100 mmol of sodium bicarbonate, a 50% solution of dextrose, and 15 units of regular insulin, all administered as an intravenous bolus. Sodium bicarbonate is an alkalinizing agent used to correct acidosis by increasing the extracellular pH, resulting in a temporary shift of potassium into the cell. Dextrose and insulin facilitate the entry of glucose into the cell, and the potassium follows the glucose. (4)
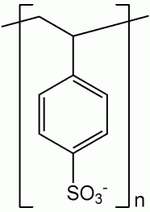
An infusion of calcium gluconate 10% was given over 30 minutes. Calcium gluconate antagonizes the cardiac conduction abnormalities caused by the hyperkalemia. Mr B had been given 30 g of sodium polystyrene sulfonate (Kayexalate) via a nasogastric tube preoperatively, and this treatment was repeated. Sodium polystyrene sulfonate causes an exchange of sodium for potassium in the gut, where the potassium can be excreted via the large intestine. The onset of the effects of sodium polystyrene sulfonate is 2 to 12 hours after administration, and the effects last 4 to 6 hours. If given orally, polystyrene sulfonate can result in decreases of 0.5 to 1 mmol/L in the serum level of potassium. Several doses are required to be effective. (4) Mr B was also treated with a continuous 1-hour albuterol nebulization. (3) Albuterol is a [[beta].sub.2]-adrenergic agonist that increases the plasma levels of insulin, resulting in a shift of the extracellular potassium into the intracellular space. With the use of a continuous 1-hour nebulization, serum potassium levels can be lowered 0.5 to 1.5 mmol/L; the effect is evident in 30 minutes and persists up to 2 hours. (4) These interventions were successful in resolving the cardiac conduction disturbances, as apparent on the second ECG (Figure 2). Mr B required emergent hemodialysis for the acute anuric renal failure due to rhabdomyolysis.
Mr B's hospital course was plagued with numerous complications. Continued ischemia of his lower trunk resulted in gangrenous changes of both buttocks and hips. On day 13 of his hospitalization, the persistent ischemia resulted in massive sacral decubitus ulcers with eschar and sacral necrosis requiring extensive debridement. The decubitus ulcers progressed to stage IV despite the use of a low-pressure mattress, aggressive wound management, and frequent turning. During a second debridement of the decubitus ulcers on day 19, a diverting colostomy was performed to prevent soilage of the sacral wounds with stool. The sigmoid colon was infarcted and gangrenous at that time. Mr B remained in critical care receiving hemodialysis and supportive care. On day 37, he returned to the operating room for an exploratory laparotomy with revision of the colostomy because of profound ischemia of the stoma. Despite aggressive therapy, Mr B's prognosis was poor, and on day 41, he died of his extensive wounds and multisystem organ failure.
REFERENCES
(1.) Johnson B. Endocrine disorders. In: Kinney MR, Dunbar SB, Brooks-Brunn JA, Molter N, Vitello-Cicciu JM. AACN Clinical Reference for Critical Care Nursing. 4th ed. Philadelphia, Pa: Mosby; 1996:849-854.
(2.) McCance KL, Heuther SE. Pathophysiology: The Biological Basis for Disease in Adults and Children. 2nd ed. Philadelphia, Pa: Mosby-Year Book; 1994:1444-1445.
(3.) Tierney LW, McPhee S J, Papadakis MA. Current Medical Diagnosis and Treatment. 40th ed. New York, NY: Lange Medical Books; 2001:877-879, 1659-1667.
(4.) Garth D. Hyperkalemia. Available at: www.emedicine.com/emerg /topic261.htm. Accessed May 24, 2005.
Linda K. Cook, RN, PhD, CCRN, CCNS, ACNP-BC. From Doctors Community Hospital, Lanham, Md.
Commentary by Mary Jo Grap (see shaded boxes).
COPYRIGHT 2005 American Association of Critical-Care Nurses
COPYRIGHT 2005 Gale Group