Background: The radicular pain caused by disc herniation can be explained by two mechanisms: the compression of the nerve root by the herniated disc or the irritation of the nerve root due to chemical factors. Percutaneous laser disc decompression (PLDD) was introduced for the treatment of lumbar disc hernias in the 1980s. Decompression of the nerve root is assumed to be an effective therapeutic mechanism for PLDD. However, laser irradiation might reduce the chemical factors that cause nerve root irritation by altering intra-disc proteins. We used nerve conduction velocities (NCV) and levels of two chemical factors to evaluate the differences between the two groups in this in vivo study.
Methods: All rabbits had the nerve root in contact with the leakage from the nucleus pulposus. One group underwent laser irradiation for the leaking nucleus pulposus including the incision site of the disc and nucleus pulposus itself. The levels of two chemical factors, prostaglandin E2 and phospholipase E2, in the intervertebral disc were measured before and after laser irradiation.
Results: NCV in the laser-irradiated group was significantly faster than in the non-laser-irradiated group. The levels of chemical factors were significantly reduced after laser irradiation.
Conclusions: One of the mechanisms thought to be responsible for PLDD's effectiveness is a decrease in the chemical factors through protein alteration in the intervertebral disc by laser irradiation. [Neurol Res 2005; 27: 319-323]
Keywords: Laser; PLDD; disk hernia; chemical factor
INTRODUCTION
Percutaneous laser disc decompression (PLDD) was introduced for the treatment of lumbar disc hernias in the 1980s1. In this procedure, laser energy is percutaneously introduced into a herniated intervertebral disc. It vaporizes a small volume of nucleus pulposus, which results in the immediate reduction of the intra-disc pressure and the relief of pain in as many as 89% of patients2.
The radicular pain caused by disc herniation can be explained by two mechanisms: the compression of the nerve root by the herniated disc3, or irritation of the nerve root by chemical factors4-7.
One of the possible effects of PLDD is the generation of heat that is able to reduce the release of chemical factors from the herniated disc. The present study was initiated to assess whether or not the generation of heat by laser irradiation reduces the release of chemical factors from the nucleus pulposus in an animal study.
MATERIALS AND METHODS
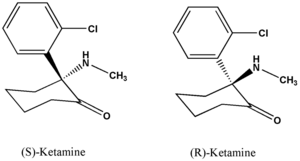
Rabbits with a body weight of 2-2.5 kg were anesthetized with an intramuscular injection of 25 mg/kg body weight of Ketalar (ketamine, 50 mg/ml). The rabbits were placed in the prone position, and a medial partial hemilaminectomy was performed between L1 and L2 under sterile conditions.
Non-laser-irradiated series (n=5)
The L2 nerve root was gently freed and moved medially to expose the L1-L2 disc. A 3-mm incision was made into the dorsolateral portion of the annulus fibrous. Although this procedure did not induce herniation of the disc material that resembles radiological or open surgery findings, the nucleus pulposus material could be identified on the scalpel blade and seen as it slowly leaked through the incision. Approximately 0.01 ml of saline was gently injected into the center of the disc through the incision in the annulus fibrosis to ensure that there was communication between the nucleus pulposus and the epidural space. The wound was sutured carefully after the procedure, and the rabbits were brought back to the area of animal holding. The rabbits were followed daily to monitor their general condition, neurologic status and the healing of the wounds.
The rabbits were again anesthetized 2 weeks after the initial surgery. We performed a laminectomy from L5 to L6 to expose the contents of the spinal canal. The L6 nerve root was identified. At the end, we re-opened the wound of the initial surgery and exposed the thecal sac at the one intervertebral level rostral to the L1 lamina. Under conditions of controlled temperature and moisture, the thecal sac was stimulated at that intervertebral level using a SEN-7203 electronic stimulator (Nihon Kohden, Tokyo, Japan). The stimulation voltage was in the range of 2.0-4.0 V. The stimulation duration was 1 millisecond. The electrographic recording was obtained from the L6 nerve root.
Laser-irradiated series (n=5)
In the first operation, laser irradiation was performed after the nucleus pulposus material was freed to leak. The laser was positioned above the leaking nucleus pulposus including the incision site of the disc and nucleus pulposus itself. A laser of wavelength was 1.014 nm with a power of 5 W continuous wave (Nd-YAG Laser, CL-50, manufactured by SLT Japan Co., Ltd). The total energy of the laser irradiation was 20 J/disc.
Two weeks after the procedure, the nerve conduction velocities (NCV) were calculated in the same fashion as in the non-laser-irradiated subjects.
Sham-operation series (n=5)
The L2 nerve root was gently freed and moved medially to expose the L1-L2 disc. However, no incision was made into the dorsolateral portion of the annulus fibrous during the initial operation. However, 2 weeks after the procedure, the NCV was calculated in the same fashion as in the non-laser-irradiated subjects.
The value of prostaglandin E2 and phospholipase A2 levels in the nucleus pulposus of the non-laser-irradiated animals and the laser-irradiated animals were evaluated. After electrographic recording, anulus fibrosus of the L1-L2 intervertebral disc was incised widely and its nucleus pulposus was removed with forceps. The obtained nucleus pulposus were homogenized on ice with the use of a pestle. These specimens were not cultured or incubated before processing.
Prostaglandin E2
A solid-phase extraction procedure as described by Powell was carried out to purify the prostaglandins in each specimen8. Briefly, the supernatant of the centrifuged homogenate was acidified and passed through a column of octadecylsilyl silica (Sep-Pak cartridges, Millipore Corporation, Bedford, MA). Polar materials were eluted with dilute ethanol and non-polar lipids and monohydroxy fatty acids with petroleum ether. Subsequent elution of the column with methyl formate gave a final fraction containing prostaglandins. After evaporation of the methyl formate, the samples were assayed for prostaglandin E2 content in duplicate using an enzyme-linked immunosorbent assay (ELISA) kit purchased from Amersham Life Science (RPN222, Arlington Heights, IL). The quantity of prostaglandin E2 in a sample was determined by interpolation.
Phospholipase A2
Each sample was thawed, ground and homogenated in a cold mixture of 0.36 N sulfuric acid/1.6 M sodium chloride (24 ml/g net weight). After 3 hours at 4°C, the mixtures were centrifuged for 30 minutes at 10,000 g. The supernatants were dialyzed against two changes of 10 mM of sodium acetate buffer, pH 4.5, and were again centrifuged for 30 minutes at 10,000g. The resultant supernatants were assayed for phospholipase A2 activity.
Phospholipase A2 activity was measured by an established method, using 1-C^sup 14^ oleate-labeled autoclaved Eschericha coli as a substrate. In a total volume of 0.5 ml, the assay mixtures contained: 10 µl HID acid extract, 100 mM buffer (sodium acetate pH 3.0-5.0, BisTris pH 6.0-7.0, HEPES pH 7.0-8.0 and glycyl glycine pH 8.0-9.0), 5 mM CaCl^sub 2^, 4.8 × 108 [1-C^sup 14^ oleate-labeled autoclaved Eschericha coli (8000 cpm and 10 nM phospholipids)]. Samples were also assayed without added CaCl^sub 2^, and in the presence of 1 mM EDTA. The reaction mixtures were incubated for 2.5 minutes at 37°C, and the reactions were stopped by the addition of 3.0 ml of chloroform-methanol (1: 2 v/v). The radioactive lipids were extracted and separated by thin-layer chromatography9,10. The results are expressed as percent hydrolysis or as nanomole phospholipids hydrolyzed per minute per milligram of protein.
We followed the "Guide to the Care and Use of Laboratory Animals" (NIH).
RESULTS
The rabbits were in a good general condition during the 14 days between the two surgical procedures, and no wound infections were noted. There was no evidence of any apparent neurologic deficit in any of the rabbits, which was based on the behavior and gait of the rabbits.
The NCV in the non-laser-irradiated rabbits was lower than in the sham-operation animals (Student's t-test, p
The values of prostaglandin E2 and phospholipase A2 in the nucleus pulposus of the non-laser-irradiated, the laser-irradiated and the sham-operated animals are presented in Figures 2 and 3. All the values from the animals in the laser-irradiated group were significantly lower than the values from the animals in the non-laser-irradiated group (Figure 2a,b). All the values from the animals in the non-laser-irradiated group were not significantly less than the values from the animals in the sham-operated group (Figure 2a,b).
DISCUSSION
Mechanical compression of the nerve root contributes to the symptoms of lumbosacral radiculopathy from lumbar vertebrae herniated discs. However, in the clinical setting, this mechanism cannot explain all of the reasons for radiculopathy in lumbar vertebrae herniated discs. Therefore, chemical factors, in addition to mechanical compression, have recently attracted attention in this field. Several reports have documented how inflammatory reactions contribute to symptoms of inferior limb pain in lumbar vertebrae herniated discs4,5,10-13. It has been experimentally clarified that the intervertebral disc tissue itself causes inflammation that is localized and changes the functional anatomy of the nerve14. Even if mechanical compression factors are not present, this fact strongly suggests that the intervertebral disc tissue alone can lead to lumbosacral area radiculopathy.
In a canine experiment, inflammatory reactions were shown to occur in the epidural space when the nucleus pulposus of a dog was placed in the epidural space12. Similar inflammatory reactions have been revealed in swine experiments13. The nerve conduction velocity falls remarkably. Many inflammatory cells and inflammation material can be identified in the perineural area when the nucleus pulposus comes in contact with cauda equina or the nerve root14. Chen et al. reported that exposure of the nerve root to nucleus pulposus for 7 days caused vacuolar swelling of the Schmidt-Lanterman incisures15 and blocked neural conduction16.
The pH value of an intervertebral disk hernia and circumferential tissue has been presented, and has been speculated to be the cause of the inflammatory reaction in the area of the nerve root17. Since this, various kinds of materials are thought to be chemical factors that contribute to inflammatory reactions secondary to intervertebral disk hernias. Glycoprotein11, immunoglobulin G18, phospholipase A2(19), Stromelysine20 and prostaglandin E2(21) have been shown to affect intraherniated discs and nerve tissue.
In this study, we measured prostaglandin E2 and phospholipase A2 as chemical factors that cause radiculopathy. Prostaglandin E2 in herniated discs was found in particular in the discs of patients who had positive straight leg raising tests21. High phospholipase A2 enzyme activity may clinically be highly relevant and is perhaps a key to the development of more effective forms of management of pain originating in a herniated disc, because the enzyme has a regulatory function through its release of arachidonic acid from cellular membranes in the inflammatory cascade after tissue injury. Enzyme activity will result in the production of key inflammatory mediators, e.g. prostaglandins, leukotriens and platelet-activating factor19,22-24. However Gronblad et al reported that phospholipase A2 enzyme activity was not particularly high in human disc tissue and did not appear to be higher in herniated or degenerated discs than control disc tissue25. But this enzyme is surely present in herniated disc. And it has the potential function to occur in an inflammatory cascade. A herniated disc including this enzyme may lead to inflammation above the affected nerve.
Intervertebral disc herniation can be treated by open discectomy, microdiscectomy or automated nucieotome discectomy. These methods achieve clinical success by reducing the volume of the nucleus pulposus or by moving the herniated disc away from the nerve root6,26-29. Smith first described the concept of intra-disc therapy for decompression of a herniated disc in 1963 as chemonucleolysis. Chemonucleolysis uses the enzyme chymopapain30 and has been used less frequently in recent years because of its allergic complications31. Instead, Hijikata et al. introduced percutaneous nucleotomy with manual instruments in 197532. By introducting an automated cutter and suction system by Onik et al.33, this less invasive technique of percutaneous nucleotomy has been popular, and has been shown to relieve pain in up to 88% of patients31. For the symptomatic lumbar disc hernia, a variety of those percutaneous procedures, termed "intra-disc therapy", have been developed as alternatives to open surgery. PLDD was introduced as an intra-disc therapy for the treatment of lumbar disc hernias in the 1980s1.
The effects of the compression mechanism on intervertebral disc hernias of PLDD is based on experimental results that show that the intervertebral disc pressure is depressed by 50% by intra-disc ablation with laser irradiation34. As for PLDD, the laser energy arrives at the intervertebral disc nucleus pulposus, and the tissue transpires by the incurred heat. The intervertebral disc pressure diminishes by forming a cavity, which results in an immediate reduction of intra-disc pressure and relief of pain in as many as 89% of patients2.
PLDD is positioned using surgical methods of treatment, for lumbar herniated discs, that aim to decrease in intervertebral disc pressure. For other therapies it is a completely foreign point to generate an increase in heat in the intervertebral disc. The fiber tip induces laser energy, and ablation usually occurs with alterations in its periphery. It has already been established that intervertebral disc pressure decreases by the ablation2. Furthermore, the heat produced by laser irradiation might decrease chemical factors and allow the therapeutic effect to take place.
In this study, the nerve conduction velocity clearly decreased when the leakage from the nucleus pulposus came in contact with the nerve root. Recovery of NCV was seen in the group of animals that received laser irradiation. In addition, levels of prostaglandin E2 and phospholipase A2 were lower in the group that received laser irradiation.
Both these chemical factors between SHAM-operated and non-laser-irradiated animals did not have a significant difference. This indicates that these chemical factors originally exist in the nucleus pulposus. These chemical factors appear to mediate some of the inflammatory effects of lumbar disc hernia. An intact annulus may provide some protection against a stimulus caused by these chemical mediators21. In this study, there was communication between the nucleus pulposus and the epidural space in the laser- and non-laser-irradiated animals, but no mechanical compression for dura mater and/or nerve root. Nucleus pulposus contained these chemical factors. These chemical factors potentially cause neural inflammation. Many inflammatory cells and inflammation material can be identified in the perineural area when the nucleus pulposus comes in contact with cauda equina or the nerve root14. Exposure of the nerve root to the nucleus pulposus resulted in neural conduction block. These chemical factors may produce this conduction block.
From this point of view, the alteration of proteins in the disc, caused by the heat produced by laser irradiation, reduces chemical factors such as prostaglandin E2 and phospholipase A2, which cause radiculopathy. This is regarded as one of the mechanisms of PLDD effectiveness.
REFERENCES
1 Choy D, Case R, Fielding W, et al. Percutaneous laser nucleolysis of lumbar disks. N Engl J Med 1987; 317: 771-772
2 Choy D. Early relief of erectile dysfunction after laser decompression of herniated lumbar disc. Spine State Art Rev 1999; 7: 11-15
3 Epstein J, Epstein B, Rosenthal A, et al. Sciatica caused by nerve root entrapment in the lateral recess: The superior facet syndrome. J Neurosurg 1972; 36: 584-589
4 Bobechko W, Hirsch C. Auto-immune response to nucleus pulposus in the rabbit. J Bone Joint Surg Am 1965; 47B: 574-580
5 Jaffray D, O'Brien J. Isolated intervertebral disc resorption. Spine 1986; 11: 397-401
6 Maroon J, Onik C. Percutaneous automated discectomy: A new method for lumbar removal. J Neurosurg 1987; 66: 143-146
7 Olmarker K, Rydevik B, Nordborg C. Autologous nucleus pulposus induces neurophysiologic and histologic changes in porcine cauda equina nerve roots. Spine 1993; 18: 1425-1432
8 Powell WS. Rapid extraction of oxygenated metabolites of arachidonic acid from biological samples using octadecylsilyl silica. Pmstaglandins 1980; 20: 947-957
9 Franson RC, Weir DL. Inhibition of a potent phospholipase A^sub 2^ activity in the synovial fluid of patients with arthritis by non-steroidal anti-inflammatory agents. Clin Res 1983; 31: 650A
10 Gertzbein S, Tait J, Devlin SR. Autoimmunity in degenerative disc disease of the lumbar spine. Orthop Clin North Am 1975; 6: 67-73
11 Marshall L, Trethewie E, Curtain CC. Chemical radiculitis. Clin Orthop 1977; 129: 61-67
12 McCarron R, Wimpee M, Hudkins PG. The inflammatory effect of nucleus pulposus. A possible element in the pathogenesis of low back pain. Spine 1987; 12: 760-764
13 Olmarker K, Byrod G, Cornefjord M. Effects of methyl-predonisolone on nucleus pulposus-induced nerve root injury. Spine 1994; 19: 1803-1808
14 Kayama S, Konno S, Olmarker K. Incision of the anulus fibrosus induces nerve root morphologic, vascular and functional changes. An experimental study. Spine 1996; 21: 2539-2543
15 Olmarker K, Nordgorg C, Larsson K. Ultrastructural changes in spinal nerve roots induced by autologous nucleus pulposus. Spine 1996; 21: 411-414
16 Chen C, Cavanugh JM, Song Z, et al Effects of nucleus pulposus on nerve root neural activity, mechanosensitivity, axonal morphology, and sodium channel expression. Spine 2004; 29: 17-25
17 Nachemson A. Intradiscal measurements of pH in patients with lumbar rhizopathies. Acta Orthop Scand 1969; 40: 23-42
18 Pennington J, McCarron R, Laros GS. Identification of IgG in the canine intervertecral disc. Spine 1988; 13: 909-912
19 Saal J, Franson R, Dobrow R. High levels of inflammatory phospholipase A2 activity in lumbar disc herniations. Spine 1990; 15: 674-678
20 Liu J, Roughley P, Mort JS. Identification of human intervertebral disc stromelysin and its involvement in matrix degeneration. J Orthop Res 1991; 9: 568-575
21 O'Donnell IL, O'Donnell AL. Prostaglandin E2 content in herniated lumbar disc disease. Spine 1996; 21: 1653-1656
22 Pruzanski W, Vadas P. Phospholipase A^sub 2^: A mediator between proximal and distal effectors of inflammation. Immunol Today 1991; 12: 143-146
23 Saal J. The role of inflammation in lumbar pain. Spine 1995; 20: 1821-1827
24 Vadas P, Pruzanski W. Biology of disease. Role of secretory phospholipase A^sub 2^ in the pathology of disease. Lab Invest 1986; 55: 391-404
25 Gronblad M, Virri J, Ronkko S, et al Controlled biochemical and immunohistochemical study of human synovial-type (Group II) phospholipase A^sub 2^ and inflammatory cells in macroscopically normal, degenerated, and herniated human lumbar disc tissues. Soine 1996; 21: 2531-2538
26 Caspar C, Mullins L, Hartman V. Laser assisted disc decompressions: a clinical trial of the Holonium: YAG laser with side firing fiber. J Clin Laser Med Surg 1995; 13: 27-31
27 Choy D, Ascher P, Saddekni S, et al. Laser-assisted disc decompression: A clinical trial of the holonium: YAC laser with side-firing fiber. Spine 1992; 17: 949-956
28 Cottlob C, Kopchok G, Peng S, et al Holonium: YAG laser ablation of human intervertebral disc: Preliminary evaluation. Lasers Surg Med 1992; 12: 86-91
29 Quigley M, Shih T, Elrifai A, et al Percutaneous laser discectomy with the ho: YAG laser. Lasers Surg Med 1992; 12: 621-624
30 Smith L. Enzyme dissolution of the nucleus pulposus in humans. J Am Med Assoc 1964; 187: 137-140
31 Schaffer J, Kambin P. Percutaneous posterolateral lumbar discectomy and decompression with a 6.9-milimeter cannula. J Bone Joint Surg Am 1991; 73-A: 822-831
32 Hijikata S, Nakayama T. Percutaneous nucleotomy: A new treatment method for lumbar disc herniation. J toden Hosp 1975; 10: 713-715
33 Onik G, Helms C, Ginsburg L, et al. Percutaneous lumbar diskectomy using a new aspiration probe. Am J Roentgenol 1985; 144: 1137-1140
34 Choy D, Altman P. Fall of intradiscal pressure with laser ablation. Spine State Art Rev 1993; 7: 23-29
Ko-ichi Iwatsuki, Toshiki Yoshimine, Manabu Sasaki, Keitaro Yasuda, Chihiro Akiyama and Rie Nakahira
Department of Neurosurgery, Osaka University Medical School, Suita, Osaka, Japan
Correspondence and reprint requests to: Ko-ichi Iwatsuki, MD, Department of Neurosurgery, Osaka University Medical School, 2-2 Yamadaoka, Suita, Osaka 565-0871 Japan. [kiwatsuki@nsurg.med.osaka-u.ac.jp] Accepted for publication August 2004.
Copyright Maney Publishing Apr 2005
Provided by ProQuest Information and Learning Company. All rights Reserved