Background & objectives: Pretransplantation injection of donor lymphohaemopoetic cells via portal venous route has been shown to improve allograft survival in mice. In the present study, the effect of perioperative portal venous administration of donor splenocytes on skin graft survival was investigated in comparison with intravenous administration of spleen cells in Swiss albino rat skin transplant model.
Methods: Using a single-donor survival study, skin allograft recipients received either no treatment, a single transfusion of donor spleen cells via portal vein or a single transfusion of donor splenocytes into vena cava. Spleen cell transfusion consisted 25×10^sup 6^ viable cells in a volume of 1 ml given just before skin grafting. Skin graft survival was assessed by macroscopic appearance. Rejection was defined as the first day on which the entire surface of the graft was necrotic. Histologically necrosis, increased connective tissue, vascularity and polymorphonuclear leucocyte (PNL) infiltration were evaluated under light microscopy.
Results: In this survival study of skin allografts, with the injection of viable spleen cells into portal vein concomitant to skin grafting, significant prolongation of mean allograft survival was induced (20.3 days), compared with untreated recipients (6.5 days, P>0.001). In the histopathologic evaluation, less PNL infiltration, necrosis, increased vascularity and connective tissue repair were observed in vena porta group with no statistical significance.
Interpretation & conclusion: It may be possible to develop protocols to induce transplantation tolerance based on the historical concept of donor specific antigen administration. However, it appears that donor spleen cell transfusion alone is not sufficient to prevent graft rejection. Thus, more efficient combination treatments are required to induce a state of durable tolerance.
Key words Donor spleen cells - skin allograft - survival - Swiss albino rats
The induction of donor-specific tolerance is critical in organ transplantation, both for the prolonged survival of the transplanted organ, and for the prevention of severe complications of chronic generalized immunosuppression. Pretreatment with donor blood or with donor lymphocytes has been shown to extend the organ allograft survival in animals and in clinical settings1-3.
Increased survival of vascularized organ allografts in rat has been achieved by active host immunization with donor antigen, passive immunization with alloantiserum and a combination of both4. It was shown that spleen cells and infiltrating leukocytes isolated from well-functioning cardiac allografts in immunologically enhanced adult rats suppressed spontaneous blastogenesis of normal syngeneic cells in vitro4.
In animal tolerance models, Billingham etaP induced tolerance to subsequently transplanted skin allografts by first engrafting self-renewing donor strain spleen cells into gestational and neonatal mice before the recipient animal's immune system was developed enough to reject the foreign leukocytes. Later on a number of studies were designed to achieve a long-term allograft survival6'7. Rao et al1 reported that, when the host rats were administrated donor spleen cells via portal vein rather than the systemic vein two weeks before the transplantation, heart graft survival was significantly longer. Many other studies have also shown prolonged allograft survival induced by perioperative portal venous inoculation of donor cells in various animal models8,9.
In the present study, the effect of perioperative portal venous administration of donor splenocytes on the survival of skin allografts, which are among the most difficult tissues to transplant using tolerance induction protocols, was investigated in comparison with intravenous administration of spleen cells, in order to establish a basic model of transplantation to settle combination protocols of tolerance induction to be used in the clinical setting.
Material & Methods
Animals: Sixty Swiss albino male rats, 6-8 wk old (200-260 g), were used. all animals were maintained on standard laboratory chow and water ad libitum, at Ege University Medical Faculty Laboratory. The study protocol was approved by the local Ethics Committee of the institution.
Experimental groups: Thirty rats were randomized into three groups of 10 rats, as recipients; group 1 : full thickness skin grafts were transplanted without any additional procedure, group 2 : full thickness skin grafts were transplanted immediately after the injection of donor spleen cells into vena cava, and group 3 : full thickness skin grafts were transplanted immediately after the injection of donor spleen cells into the portal vein.
Donor operation
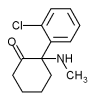
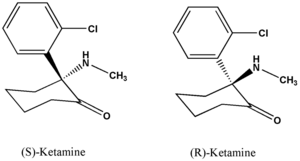
Removal of spleen and skin graft preparation: Donors of spleen cells and skin were male Swiss albino rats. Following the anaesthesia with intramuscular administration of ketamine (Ketalar®, EczacibasiWarner Lambert, Istanbul, Turkey) at a dose of IOO mg/ kg, spleens were removed through midline incision. The skin grafts were prepared as described previously10. Briefly, following the closure of the abdomen, full thickness skin grafts of 1 cm^sup 2^ were removed from the back of donors, and the undersurface was scraped to remove fat and muscle. Prepared skin was placed on sterile filter paper and kept at room temperature.
Spleen cell preparation: The removed spleens were mechanically dispersed and pressed gently through 60gauge mesh stainless steel screen into RPMI-1640 medium (Associated Biomedic Systems, Inc., Buffalo, NY). The spleen cell suspension was centrifuged at 1500 g for 5 min. The supernatant was decanted. The spleen cells were resuspended in tris-buffered ammonium chloride solution at a concentration of 25×10^sup 6^ splenocyts/ ml.
Recipient operation
Skin allograft recipients received either no treatment (group I), a single transfusion of donor spleen cells via portal vein through midline incision (group 3) or a single transfusion of donor splenocytes into vena cava through the thigh vein (group 2). Spleen cell transfusion consisted of 25×10^sup 6^ viable cells in a volume of 1 ml given just before skin grafting. Initially in group 1 and immediately after the splenocyte injection in groups 2 and 3, full thickness skin grafts were transplanted. The dorsal surfaces of anaesthetized recipient rats were shaved and washed with povidon-iodine. A graft bed of 1 cm^sup 2^ prepared by cutting an area of epidermis and dermis down to the level of intrinsic muscle. The grafts, 1 cm^sup 2^ in area, were placed to the prepared bed with 4/0 silk sutures and then, covered with Vaseline impregnated gauze and an adhesive plastic bandage. After four days, the bandage was removed.
Histology. Skin graft survival was assessed and scored daily by macroscopic appearance. Rejection was defined as the first day, on which the entire surface of the graft was necrotic. When necrosis was observed, grafts were excised. Each graft was fixed with formalin, paraffin embedded, stained with haematoxylin-eosin, and examined under light microscopy. In all the grafts with necrosis, the common microscopic finding was an acute graft rejection with complete destruction of the epidermis, with extensive cellular infiltration in the subcutaneous tissue.
Statistical analysis: Statistical analysis was done using non-parametric Kruskal-Wallis test. The duration of allograft survival was compared by the Mann-Whitney U test. In cases for multiple comparisons, the Bonferroni correction was made. P
Results & Discussion
All group of animals were evaluated in terms of graft survival. Graft survival varied between 4-7 days in group 1, 5-7 days in group 2, and 11-25 days in group 3. Though better survival time was achieved in vena cava group compared to control group, it was not statistically significant. There was statistically significant increase in the time of graft survival in group 3 compared to groups 1 and2(P
Under light microscopy, necrosis in both epidermis and dermis with extensive polymorphonuclear leucocyte infiltration (PNL) in deep dermis were seen in all three groups. High density of connective tissue and increased vascularity were observed especially in portal vein group (group 3) of animals with no statistical significance (Figs 1,2).
Much has been reported on the ability to prolong antigen-specific survival of allogenic skin grafts in mice by penetrating grafted animals with antigen delivered by the portal vein11-15. Triger et ?/16 demonstrated that injection of donor antigens directly into the portal venous system of the rat induced immunologie tolerance to an allograft by reducing the immune response. Perioperative portal venous administration of donor spleen cells at a dose of 2×10^sup 9^ was shown to prolong renal allograft survival in a canine kidney transplant model8. In the present study the injection of splenocytes via portal vein increased graft survival time three-fold compared to the control group.
Wang et al", investigated the induction of donor-specific tolerance to skin allografts in rabbits using bone marrow transplantation techniques. Various routes of bone marrow transplantation (i.e., intravenous, portal venous, or intraosseous) were also examined in this study. It was demonstrated that induction of allograft tolerance could be achieved by bone marrow transplantation in a rabbit model17. Pretreatment with intraportally administered ultra violet B-irradiated donor splenocytes prevented rejection of circumferential rat trachea! allograft segments by inducing a donor-specific immune hyporesponsiveness18. Nagano et al19 reported that intraporta! (IP) injection of donor spleen cells (SPCs) prevented liver allograft rejection. Stable chimerism in the spleen was observed in intraportally injected rats up to 28 days after injection not only at the DNA level but also at the cellular level19. No chimerism was detected in other organs (including the thymus, lymph nodes, and liver). The long-term presence of injected allogeneic SPCs in the spleen was demonstrated after IP injection but not after IV injection, and this phenomenon might be one of the mechanisms involved in portal venous immunosuppression. It was shown that the specific tolerance to skin grafts in rat could be achieved by transferring T-enriched thoracic duct lymphocytes from neonatally tolerized rats to sublethally irradiated syngeneic recipients20. Kilshaw and Brent21 induced unresponsiveness to skin allografts in adult mice by treatment with donor strain crude liver extract combined with Bordetalla pertusis vaccine and antilymphocyte serum. This state of unresponsiveness could be adoptively transferred to partially immunosuppressed recipients by splenocytes harvested from mice with long surviving grafts. Though the exact mechanism of immunologie unresponsiveness in unclear, a number of mechanisms for the induction of tolerance, such as immune-regulatory effect of Kupffer cells, induction of anti-idiopathic antibody, production of immunosuppressive factors by the stimulation of allogeneic antigen, and deletion of effector clones have been proposed22"25. The previous studies suggested that for the prolongation of allograft survival, a pre-transplant treatment with portal venous administration of donor splenocytes 7-14 days before transplantation would permit long-term survival16,26-29. To apply this effect to the clinical setting, Tsuji et aP administrated the donor cells at the time of renal allograft surgery in dogs, which required only a short course of intervention, and demonstrated a significantly prolonged renal allograft survival. On the other hand, in the rat model of highly antigenic donor skin allograft, Markees el aP found no statistically significant difference in skin allograft survival, when the simultaneous administration of donor spleen cells was compared with the standard treatment initiated a week in advance of the graft. In our study, the mean survival time for skin allografts that were transplanted following the injection of splenocytes via portal vein (group 3) was found to be significantly more compared to the other two groups. Under light microscopy, necrosis in both epidermis and dermis with wide PNL infiltration in deep clermis was seen in all the three groups. High density of connective tissue and increased vasculanty were observed especially in portal vein group. This situation may probably be explained with long-term reaction.
In conclusion, the present study demonstrated a marked prolongation of skin allograft survival induced by perioperative administration of splenocytes into portal vein. Though the mechanism by which it induces prolonged graft survival is not known, it appears that donor spleen cell transfusion alone is not sufficient to prevent graft rejection. It may be possible to develop protocols to induce transplantation tolerance based on the historical concept of donor specific antigen administration, however, combination treatments are required to induce a state of durable tolerance.
References
1. Sollinger HW, Burlingham WJ, Sparks EM, Glass NR, Beizer FO. Donor-specific transfusions in unrelated and related HLA-mismatched donor-recipient combinations. Transplantation 1984; 38: 612-5.
2. Honian WP, Williams KA, Millard PR, Morris PJ. Prolongation of renal allograft survival in the rat by pretreatment with donor antigen and cyclosporin A. Transplantation 1981; 31 : 423-7.
3. TakiffH, Novak M, Yin L, Iwaki Y, Terasaki Pl. Examination of the clonal deletion hypothesis following transfusions in rat cardiac transplants. Transplantation 1987; 43 : 145-51.
4. Hendry WS, Tilney NL, Baldwin WM 3rd, Graves MJ, Milford E, Strom TB, et al. Transfer of specific unresponsivencss to organ allografts by thymocytes. J Am Soc Nephrol 1999; 10 : 2454-63.
5. Billingham RE, Brent L, Medawar PB. Actively acquired tolerance of foreign cells. Nature 1953; 172 : 603-7.
6. Martinelli GP, Horowitz C, Chiang K, Racelis D, Schanzer II. Pre-transplant conditioning with donor-specific transfusions using heated blood and cyclosporine: preservation of the transfusion effect in the absence of sensitization. Transplantation 1987;43: 140-5.
7. Rao VK, Burris DE, Gruel SM, Sollinger HW, Burlingham WJ. Evidence that donor spleen cells administrated through the portal vein prolong the survival of cardiac allografts in rats. Transplantation 1988; 45 : 1145-6.
8. Tsuj i T, Tashiro S, Tanabe D, Sawada T, Inoue K, Kawamoto S, et al. The effect of perioperative portal venous injection of donor spleen cells on renal allograft survival in dogs. Transplantation 1994; 55 : 883-6.
9. Markecs TG, Phillips NE, Noelle RJ, Shultz LD, Mordes JP, Greiner DL, et al. Prolonged survival of mouse skin allografts in recipients treated with donor splenocytes and antibody to CD40 ligand. Transplantation 1997; 64 : 329-35.
10. Markces TG, Dc Fazio SR, Gozzo .IJ. Prolongation of adult, skin allograft survival by contransplantation of neonatal skin in anti-lymphocyte serum and donor bone marrow cell-treated mice. Transplantation 1990; 50 : 911-4.
11. Qian JH, Hashimato T, Fujiwara H, Hamaoka T. Studies on the induction of tolerance to alloantigens. The abrogation of potentials for delayed-type hypersensitivity responses to alloantigens by portal venous inoculation with allogeneic cells. J lmimmol 1985;134: 3656-61.
12. Kcnick S, Lowry RP, Forbes RDS, Lisbona R. Prolonged cardiac allograil survival following portal venous inoculation of allogeneic cells: what is "hepatic tolerance". Transplant Proc 1987; 19 : 478-80.
13. Gorczynski RM. Immunosupression induced by hepatic portal venous immunization spares reactivity in 1L-4 producing T lymphocytes. Immunol Lett 1992; 33 : 67-77.
14. Gorczynski RM. Wojcik D. A role for non-specific (cyclosporin A) or specific (monoclonal antibodies to ICAM-I, LFA-I and inierleukin-10) immunomodulation in the prolongation of skin allografls after antigen-specific pre-transplant immunization or transfusion. J Immunol 1994; 152 : 2011-9.
15. Gorczyzski RM, Kiziroglu F. Tolerance induction to multiple minor histoincompatible cells is associated with preferential activation ofTh2 cells. Transplantation 1994; 58 : 51-8.
16. Triger DR, Cynamon MH, Wright R. Studies on hepatic uptake of antigen: I. Comparison of inferior vena cava and portal vein routes of immunization, immunology 1973; 25 : 941-50.
17. Wang YB, Ogawa Y, Doi H, Kusumoto K, Jin TN, Ikehara S. Long-term immunologie induction of donor-specific tolerance to skin allografts by bone marrow transplant in rabbits. Plast ReconstrSurg2QQ3; 111 : 298-9.
18. Genden EM, Mackinnon SE, Yu S, Hunter DA, Flye MW. Portal venous ultraviolet B-irradiated donor alloantigen prevents rejection in circumferential rat tracheal allografts. Otolaryngol Head Neck Sitrg 2QQ]; 124 : 481-8.
19. Nagano H, TanigawaT, YoshidaT, OtaH, Akagi K, Hasuike Y, et al. Role of micro-chimerism in inducing immunological tolerance by intraportal injection of donor spleen cells in rats. Cell Transplantation 1995; 4 : 59-60.
20. Dorsch S, Roser B. Recirculating suppressor T cells in transplantation tolerance. J Exp Med 1977; 145 : l 144-57.
21. Kilshaw PJ. Brent L. Further studies on suppressor T cells in mice unresponsiveness to H-2 incompatible skin grafts. Transplant Proc 1977; 9 :117-9.
22. Kamei T, Gallery MP, Flye MW. Kuppler cell blockade prevents induction of portal venous tolerance in rat cardiac allograft transplantation. J Sur g Res 1990; 48 : 393-6.
23. Satoh S, Quian JH, Kokudo S, Ikegami R, SudaT, HamaokaT, el al. Studies on the induction of tolerance to alloantigens: III. Induction of antibodies directed against alloantigen-specific delayed-type hypersensitivity T cells by a single injection of allogeneic lymphocytes via portal venous route. Jlmmunol 1988; 140:717-22.
24. YoshimuraN, Matsui S, HamashimaT, Lee CJ, Ohsaka Y, Oka T. The effects of perioperative portal venous inoculation with donor lymphocytes on renal allograft survival in the rat: I. Specific prolongation of donor grafts and suppressor factor in the scrum. Transplantation 1990; 49 : 167-71.
25. Qian JH, HashimatoT, FujiwaraH, HamaokaT. Studies on the induction of tolerance to alloantigens: the abrogation of potentials for delayed type hypersensitivity responses to alloantigens by portal venous inoculation with allogeneic cells. Jlmmunol 1987; 139: 3656-9.
26. Kenick S, Lisbona R, Marghesco D, Lowry RP. Prolonged cardiac allograft survival following portal venous inoculation of allogeneic cells: immunologically specific entrapment of allogeneic cells within the liver. Transplant Proc 1987; 19:3057-61.
27. Kamei T, Gallery MP, Flye MW. Pretransplant portal venous administration of donor antigen and portal venous allograft drainage synergistically prolongs rat cardiac allograft survival. Surgery 1990; 108: 415-21.
28. Starzl TE. The birth of clinical organ transplantation. JAm Coll Sui-g 2001; 192: 431-46.
29. Margenthaler JA, Landeros K, Kataoka M, Flye MW. Mechanism of portal venous tolerant long-term MHC Class I Ld-specific skin graft survival in transgenic 2CFl mice. Transpl lmmunol2003; 11: 23-9.
Eray Kara*, Gokhan Icoz, Murat Dayangac, Ozer Ilkgul*, Hikmet Ertan, Yaman Tokat & Ender Terzioglu
Department of General Surgery of Ege & Celai Bayar University, *Department of Internal Medicine of Mediterranean University, Izmir-Turkey
Received August 8, 2003
Reprint requests : Dr Eray Kara, Mithatpasa cd. No.: 394/5. Catalkaya Apt. 35260. Karatas-Izmir/Turkey e-mail: craykara@hotmail.com
Copyright Indian Council of Medical Research Mar 2004
Provided by ProQuest Information and Learning Company. All rights Reserved