Telithromycin (Ketek) is a ketolide antibiotic that was approved by the Food and Drug Administration (FDA) on April 1, 2004. The drug is approved for treatment of acute bacterial exacerbations of chronic bronchitis (ABECB), acute bacterial sinusitis (ABS), and mild-to-moderate community-acquired pneumonia (CAP).1
Community-acquired respiratory tract infections (RTIs) secondary to Streptococcus are a common cause of morbidity and mortality, they account for more than 20 million primary care provider (PCP) visits, and are a major reason for absenteeism from work and school.2 Streptococcus pneumoniae is the most predominant pathogen for RTIs, including CAP, ABECB, and ABS. Also, Haemophilus influenzae and Moraxella catarrhalis contribute to these pathologies.
Since 1896 when Ernest Duschesne discovered and Alexander Fleming (1928) rediscovered that a mold, Penicillium, could severely injure and even kill bacterial pathogens, antibiotics have been saving lives.3 However, bacteria began to mutate almost immediately and shared ways to resist the pharmacodynamic effects of anitbiotics. In fact, only 4 years after penicillin began mass production in 1943, resistant bacteria strains began to appear. Resistance rose in the 1990s because of complacency in the 1980s.4 By 1999, the World Health Organization recognized the severity of the problem and conducted a workshop to strategize a global plan to contain antimicrobial resistance.5
One surveillance study involving 34 United States medical centers showed that among 1,601 clinical isolates of S. pneumoniae, 29.5% were penicillin-resistant, 19.3% were erythromycin-resistant, and 13.2% were tetracycline-resistant.6
* Mechanism of Action
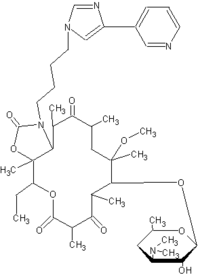
Telithromycin, a ketolide, was developed for the treatment of community-acquired RTIs. The antibacterial activity of telithromycin, like that of the macrolides, is due to interaction with the 50 S subunit of the bacterial ribosome and subsequent inhibition of ribosome assembly and protein synthesis.
The structural modifications of telithromycin render it more active against resistant strains of S. pneumoniae in comparison to macrolides.7-10
In vitro data have demonstrated telithromycin to be active against S. pneumoniae (including multidrug-resistant strains of S. pneumoniae), Staphylococcus aureus (methicillin-and erythromycin-susceptible isolates only), H. influenzae, M. catarrhalis; Chlamydophila pneumoniae, and Mycoplasma pneumoniae.
* Pharmacokinetics
Telithromycin is absorbed rapidly and pharmacokinetic studies suggest 800 mg once a day provides plasma and tissue drug levels effective against specified pathogens implicated in RTIs.7,12-14 Peak plasma concentrations (approximately 2 meg/ml) in fasting, healthy volunteers were attained 1 hour after an 800 mg oral dose of telithromycin with an absolute bioavailability of 57%.7,12 Steady-state plasma concentration was reached within 2 to 3 days of once-daily dosing with 800 mg telithromycin.7,12,13
The mean terminal elimination half-life of telithromycin is 10 hours. Following a single-dose administration of telithromycin (n=18) the maximum plasma concentration (C^sub max^) was 1.9 mcg/mL (SD=0.80) and the AUC was 8.25 mcg.h/mL (SD=2.6), terminal plasma half-life was 7.16 hours (SD=1.3), and the plasma concentration at 24 hours post-dose was 0.03 mcg/mL (SD=0.013). Following multiple doses (n=18), C^sub max^ was 2.27 mcg/mL (SD=0.71), time to C^sub max^ was 1.0 hour (SD=0.5 to 4.0), AUC was 12.5 mcg.h/mL (SD=5.4), terminal plasma half life was 9.81 hours (SD=1.9), and plasma concentration at 24 hours post-dose was 0.07 mcg/mL (SD=0.051). Total in vitro protein binding (primarily due to albumin) is approximately 60% to 70% and does not appear to be modified in the elderly or in patients with hepatic impairment. The volume of distribution after intravenous infusion is 2.9L/kg.12 Several studies demonstrated that telithromycin concentrations in epithelial lining fluid and bronchial mucosa (critical for effective treatment of RTIs) exceeded the minimum inhibitory concentration (MIC) of common respiratory pathogens for 12 to 24 hours.7,14,15
Elimination of telithromycin is complete within 72 hours.7,16 It is primarily metabolized by the liver. Approximately 50% of the liver metabolism is mediated by CYP450 3A4 and the remaining 50% appears to be CYP450 independent. Telithromycin is eliminated via multiple pathways with approximately 7% unchanged in the feces and removed by biliary and/or intestinal secretion.7,12 Approximately 13% of the dose is excreted unchanged in the urine, and 37% is metabolized by the liver. An increase in renal elimination was seen in hepatically impaired patients, suggesting the renal system may compensate for decreases in metabolic clearance. Patients with severe renal impairment (CLcr
In an analysis of 20 elderly subjects who participated in a Phase III study, 14 subjects older than 65 years of age with CAP had a 2.0-fold increase in AUC compared with subjects younger than 65 years of age in a Phase I study. No dosage adjustment was recommended based on age alone.
* Clinical Efficacy
Telithromycin has been studied in all three indications: CAP, ABS, ABECB. In controlled CAP studies the clinical efficacy rates ranged from 88.3% to 94.6% for telithromycin and 88.5% to 94.2% for comparators. In controlled ABS trials, clinical efficacy rates range from 75.3% to 85.2% for telithromycin and 74.5% to 82.0% for comparators. In controlled ABECB trials, clinical efficacy rates ranged from 85.8% to 86.4% for telithromycin vs. 82.1% to 89.2% for comparators, according to the packaging insert.
* Prescriber's Considerations
Ketek tablets come in 400 mg light-orange, oval, film-coated tablets and are available as Ketek Pak 10-tablet cards for $46.15.10,12 Note that this pricing is based on the whole acquisition cost and not an average wholesale price. Average wholesale prices are commonly used for pricing and are only available from a third party. Bottle and unit dose packaging are also available. Recommended dosage for ABECB and ABS is 800 mg (2 x 400 mg tablets) orally, once a day for 5 days. For mild-to-moderate CAP, the therapy should be continued for 7 to 10 days.10,12 Ketek may be taken with or without food.10,2 No dosage adjustments are necessary for patients with hepatic or mild to moderate renal insufficiency or for the elderly.7
Telithromycin is indicated for susceptible strains of microorganism for patients 18 years or older with ABECB due to S. pneumoniae, H. influenzae, or M. catarrhalis; mild-to-moderate CAP due to S. pneumoniae (including multidrug-resistant isolates), H. influenzae, M. catarrhalis, C. pneumoniae or M. pneumoniae; and acute sinusitis due to S. pneumoniae, S. aureus, M. catarrhalis, and H. influenzae. Like all antibiotics, it should only be used to treat infections that are proven, or, at minimum, strongly suspected to be caused by susceptible bacteria to prevent drug-resistant bacteria development.
* Contraindications
Telithromycin is contraindicated in patients with a hypersensitivity to telithromycin (or any of the components in the tablets) or any macrolide antibiotic. Telithromycin is contraindicated in patients taking cisapride or pimozide due to drugdrug interaction.
* Warning
Pseudomembranous colitis is a possible complication from any antibacterial agent, including telithromycin. QTc interval prolongation may occur with telithromycin. Patients with known QTc interval prolongation or with proarrhythmic conditions should not take telithromycin. Aventis Pharmaceuticals reported no cardiovascular morbidity or mortality secondary to QTc prolongation in 4,780 people, including 204 patients with a prolonged QTc baseline in clinical efficacy trials with telithromycin.12 Telithromycin is not recommended for patients receiving Class 1A (quinidine, procainamide) or class III (dofetilide) antiarrhythmic medications.
* Precautions
Telithromycin may cause blurred vision, difficulty focusing, and diplopia. Although this problem reportedly occurred most often after the first or second dose, it may occur after any dose and may last several hours. Patients should be aware of this potential, especially if they plan to drive or engage in possibly hazardous activities. Increased liver enzymes and hepatitis have been reported secondary to telithromycin use. Although this scenario is usually reversible, caution should be used in patients with a history of hepatitis or jaundice associated with the use of telithromycin.12 Telithromycin is not recommended in patients with myasthenia gravis.
* Significant Client/Family History
Practitioners should elicit personal and family history of QTc prolongation or personal history of proarrhythmic conditions such as hypokalemia or clinically significant bradycardia. Patients should also be questioned about any history of myasthenia gravis, liver disease, and medication history, including current use of simvastatin, lovastatin, atorvastatin, pimozide, digoxin, rifampin, midazolam, other benzodiazepines, or other medications that are affected by or effect the CYP3A4 pathways.
* Drug Interaction
CYP3A4 inhibitors such as itraconzaole and ketoconazole had interactions with concomitant telithromycin use. A multiple-dose interaction study with itraconzaole showed that C^sub max^ of telithromycin was increased by 22% and AUC by 54%. A multiple-dose interaction study with ketoconazole showed that C^sub max^ of telithromycin was increased by 51% and AUC by 95%. Grapefruit juice did not affect the pharmacokinetics of telithromycin.12
Telithromycin inhibits the CYP450 3A4 system and, therefore, giving telithromycin with any drug that is metabolized by the CYP450 3A4 system has the potential to increase or prolong the therapeutic and adverse effects of the coadministered medication. Dosage adjustments may be necessary.
Coadministration with CYP 3A4 inducers, such as rifampin, should also be avoided because it may result in subtherapeutic levels of telithromycin and, hence, loss of effect and a potential for development of drug-resistant strains of bacteria.
Simvastatin coadministered with telithromycin had a 5.3-fold increase in simvastatin C^sub max^ and a 8.9 increase in AUG. When administered 12 hours apart, there was a 3.4-fold increase in simvastatin C^sub max^. Therefore, therapy with either simvastatin, lovastatin, or atorvastatin should be suspended during the course of telithromycin treatment. Midazolam given with telithromycin resulted in 2-fold (I.V. administration) to 6-fold (oral administration) increases in the AUC of midazolam. CYP2D6 substrates, such as metoprolol, coad-ministered with telithromycin also resulted in increases of approximately 38% on the C^sub max^ and AUC of metoprolol. There was no effect on the elimination half-life of metoprolol. There were also no pharmacokinetic effects on paroxetine when administered with telithromycin.12
Other drug interactions of note include increases in digoxin and theophylline levels when coadministered with telithromycin (see package insert for details). Drug interaction studies with telithromycin showed no clinically relevant pharmacokinetic interactions with ranitidine or antacids containing aluminum and magnesium hydroxide. Although a drug interaction study with healthy subjects showed no clinically relevant pharmacokinetic interactions with telithromycin and warfarin, consideration should be given to monitoring prothrombin times/INR while patients are receiving these two drugs. Oral contraceptives containing ethinyl estradiol and leonorgestrel given with telithromycin did have a steady-state AUC of levonorgestrel increase of 50%; however, this did not interfere with the antiovulatory effect of the oral contraceptives.12
Other potential drug interactions include elevated levels of carbamazepine, cyclosporine, tacrolimus, sirolimus, hexobarbital, and phenytoin. Ergot alkaloid derivatives such as ergotamine have caused ergot toxicity when given with other macrolide antibiotics.
* Use in Special Populations
Telithromycin is a Pregnancy category C drug. Caution is suggested for nursing women. The safety and effectiveness of telithromycin in patients younger than 18 years old has not been established.
* Adverse Reactions
Phase III clinical trials involved 4,780 patients receiving Ketek 800 mg once daily for 5 days or 7 to 10 days. Most adverse events were mild to moderate in severity and consisted primarily of diarrhea (10.8% telithromycin vs. 8.6% comparators) and nausea (7.9% vs. 4.6%) (see Table: "All Treatment-Emergent Adverse Events (TEAEs) Reported in Controlled Phase III Clinical Studies (Percent Incidence)").17 Refer to the Ketek package insert for adverse events less than 2%.
Incidence of visual treatment-emergent adverse events in controlled Phase III studies were 1.1% for telithromycin vs. 0.28% for comparators.
* Summary
In cases of known or suspected bacterial infections, telithromycin is an effective antimicrobial agent. Telithromycin, the first member of the ketolide antibacterials, is approved for the treatment of adult patients with ABS, ABECB, and mild-to-moderate CAP. It has demonstrated efficacy in these indications in controlled trials and is generally well tolerated with most adverse events being transitory and mild-to-moderate in intensity. Given the efficacy and safety profile of this drug, telithromycin provides a new treatment option for the empiric management of mild-to-moderate community-acquired RTIs.
REFERENCES
1. Doern GV, Brown SD: Antimicrobial susceptibility among community-acquired respiratory tract pathogens in the USA. Data from Protekt US 2000-01. J Infection Jan 2004; 48(l):56-65.
2. Clark JP, Langston E: Ketolides: A new class of antibacterial agents for treatment of community-acquired respiratory tract infections in a primary care setting. Mayo Clinic Proc 2003; 78:1113-1124.
3. Lewis, R: The rise of antibiotic-Resistant Infections: US Food and Drug Administration FDA Consumer Magazine September 1995. Retrieved July 19, 2004, from http://www.fda.gov/fdac/features/795_antibio.html
4. Ibid.
5. World Health Organization. Containing antimicrobial resistance: Review of the literature and report of a WHO workshop on the development of a global strategy for the containment of antimicrobial resistance.Report no who/cds/csr/ drs/99.2. Geneva, Switzerland: World Health Organization; 1999.
6. Doern GV, Brown SD: loc cit.
7. White R. Antibiotic resistance: Where do ketolides fit? Pharmacotherapy 2002 22(1):18-29. 2002 Pharmacotherapy Publications. Retrieved July 19, 2004, from www.medscape.com/ viewarticle/423227.8. Blasi F, Tarsia P, Cosentini R, et al: Newer antibiotics for the treatment of respiratory tract infections. [Review], Current Opinion in Pulmonary Medicine May 2004; 10(3):189-196.
8. Blasi F, Tarsia P, Consentini R, et al: Newer antibiotics for the treatment of respiratory tract infections [Review]. Current Opinion in Pulmonary Medicine May 2004: 10(3):189-196.
9. Ma Z, Nemoto P: Discovery and development of ketolides as a new generation of macrolide antimicrobial agents. Current Medicinal Chemistry 2002;1(1): 15-34. Retrieved July 19, 2004 from http://www.ingenta.com/isis/searching/Expand/ ingenta?pub-infobike://ben/cmcaia/2002/ 00000001/00000001/art00003
10. O'Mara N: New Drug: Telithromycin (Ketek TM). Pharmacist's Letter/Prescriber's Letter Detailed Document # 200606. June 2004): 20(200606). Ca: Therapeutic Research Cent.
11. Zhanel G, Walters M, Noreddin A, et al: The ketolides: a critical review. Drugs 2002; 62(12): 1771-804. Retrieved from http://www.ncbi.nlm. nih.gov/entrez/query.fcgi?cmd-Retrieve&d= PubMed&list_uids=12149046&dopt=Abstract.
12. Aventi sPharmaceuticals: Ketek TM: Telithromycin Tablets. 2004. Retrieved July 1,2004, from www. aventis-us.com/PIs/ketek_txt. html
13. Namour F, Wessels DH, Pascual MH, et al : Pharmacokinetics of the new ketolide telithromycin(HMR 3647) administered in ascending single and multiple doses. Antimicrob Agents Chemother 2001; 45: 170-5.
14. Andrews J, Honeybourne D, Khair O, et al: Penetration of telithromycin (HMR 3647) administered in ascending single and multiple doses. Antimicrobial Agents Chemotherapy 2001; 45:170- 5.
15. Muller-Serieys C, Andrew J, Vacheron, F, et al: Tissue kinetics of telithromycin, the first ketolide antibacterial. JAC 2004 Feb; 53(2); 149-157.
16. Sultan E, Cantalloube C, Patat A, et al: (HMR 3647). Clin Microbiol Infection 2000; 6(suppl 1):203.
17. FDA Package Insert: US FDA, Center for Drug Evaluation and Research, Consumer Drug Information, March 2004. Retrieved Aug. 2004 from http://www.fda.gov/cder/consumerinfo/.
Lynn Wimett, RN, ANP, EdD
Gary Laustsen, RN, PhDc, CFNP
Drug News Co-Editors
Copyright Springhouse Corporation Sep 2004
Provided by ProQuest Information and Learning Company. All rights Reserved