Mills GD, Oehley MR, Arrol B. Effectiveness of beta lactam antibiotics compared with antibiotics active against atypical pathogens in non-severe community acquired pneumonia: meta-analysis. BMJ 2005; 330:456-460.
* Clinical Question
In the treatment of patients with community-acquired pneumonia, is there a difference among antibiotics?
* Bottom Line
Strange, but true: Oral beta-lactam antibiotics--amoxicillin, amoxicillin/clavulanate (Augmentin), or a cephalosporin--are as effective in the treatment of community-acquired pneumonia as antibiotics active against atypical pathogens, even in patients infected with Mycoplasma pneumoniae or Chlamydia pneumoniae. These old standbys can be used instead of the more expensive drugs for most patients.
Legionella infection still requires treatment with an antibiotic effective against atypical pathogens, but in these studies only 1.1% of the patients with nonsevere pneumonia had Legionella. These results are backed up by similar findings from clinical practice (Hedlund J, et al. Scand J Infect Dis 2002; 34:887-892). (LOE=1a)
Study Design
Meta-analysis (randomized controlled trials)
Setting
Various (meta-analysis)
Synopsis
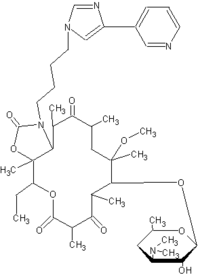
We have to treat some patients with community-acquired pneumonia (CAP) for atypical bacteria, just in case, don't we? This question was answered by the authors of this meta-analysis. They identified 18 studies comparing a beta-lactam antibiotic with an antibiotic active against the atypical pathogens M pneumoniae, Legionella species, and C pneumoniae: macrolides, fluoroquinolones, or ketolides (eg, telithromycin [Ketek]). They used rigorous methods to identify the studies, searching 3 databases for articles published in any language, searching the reference lists of review articles and retrieved studies, and including unpublished research conducted by pharmaceutical companies. Two reviewers independently screened the studies for inclusion. On average, the 6749 patients in the clinical trials were younger than the typical patient with pneumonia (in most studies the average age was between 40 and 55 years) and had a better risk profile.
Neither macrolides, ketolides, or fluoroquinolones were superior to beta-lactam antibiotics. When analyzed separately by type of antibiotic, neither macrolides nor fluoroquinolones were superior, either with regard to cure or mortality rates at the time specified in the study, usually end of treatment or at 10 days. The speed of response, relapse, or length of stay were not compared.
Here's a surprising outcome: There was no difference between beta-lactams and the other drugs in patients who had M pneumoniae or C pneumoniae. The numbers of patients in these subgroups was small: 211 patients had Mycoplasma infections and 115 had Chlamydia infections. The antibiotics active against atypical pathogens were significantly better at producing clinical cures in the treatment of 75 patients with Legionella (relative risk=0.4; 95% CI, 0.19-0.85).
The investigators used a combined endpoint of success, including cure of pneumonia, absence of adverse drug reactions, absence of medical complications, no need for additional visits, no changes in initial treatment, and no hospital admission or death within 30 days. This outcome was achieved by 83.6% of outpatients and 80.7% of hospitalized patients. Readmission rates were similar in the 2 groups (6%-7%). Health-related quality-of-life scores measured at 7 and 30 days were similar in both groups. More outpatients than inpatients reported satisfaction with their overall care (91.2% vs 79.1%; P=.03).
COPYRIGHT 2005 Dowden Health Media, Inc.
COPYRIGHT 2005 Gale Group