The authors report a case of pulmonary aspergilloma in which a fungus ball was visualized and a biopsy specimen was obtained at fiberoptic bronchoscopy. The fungus ball was successfully treated with bronchoscopic instillation of ketoconazole. It appears that this approach can be useful in the treatment of patients who are high-risk candidates for pulmonary resection.
Pulmonary aspergilloma usually arises from colonization and proliferation of Aspergillus organisms in a preexisting cavity. A standard chest radiograph showing an intracavitary mass with an air-crescent sign is usually sufficient to make the diagnosis of mycetoma. Visualization of the mycetoma during fiberoptic bronchoscopy is extremely rare.[1]
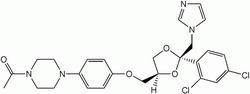
Hemoptysis is the cause of death in 2 to 24 percent of patients with pulmonary aspergilloma.[2] Traditionally, surgical resection has been the treatment of choice in these patients, although morbidity and mortality rates may be as high as 25 and 8 percent, respectively.[2] Antifungal agents have been used in a variety of ways.[2,3] Several investigators have instilled antifungal agents endobronchially or via the transthoracic route into the cavity.[4,5] We report a case of pulmonary aspergilloma in which the fungus ball was visualized on fiberoptic bronchoscopy and which was successfully treated by bronchoscopic instillation of ketoconazole into the cavity.
CASE REPORT
A 34-year-old nonsmoking man presented with a history of recurrent, moderate to massive hemoptysis for 5 months. He had been treated at a private nursing home with blood transfusions and antibiotics. There was no history of fever, chest pain, breathlessness, or weight loss. Three years previously, on the basis of a chest radiograph, a diagnosis of pulmonary tuberculosis had been made, and the patient was treated with rifampicin, isoniazid, and ethambutol for 1 year. There was significant improvement with this treatment, and the patient had been asymptomatic until the present illness.
The patient had evidence of a left upper lobe fibrocavitary lesion. A chest radiograph (Fig 1) showed a left upper lobe cavity with fibrosis. A radiodense shadow was seen inside the cavity, and the air-crescent sign was present. The right upper lobe also showed evidence of fibrosis. Fiberoptic bronchoscopy revealed a yellowish mass protruding in the anterior segment of the left upper lobe. A biopsy specimen from the lesion showed clusters of fungal hyphae suggestive of aspergillosis. The sputum examination was negative for acid-fast bacilli, but showed both Aspergillus flavus and Candida albicans organisms. Fungal serology was positive for A flavus. While in the hospital, the patient was noticed to be jaundiced. Liver function tests revealed a serum bilirubin level of 4 mg/100 ml; SGOT and SGPT of 67 and 175 IU, respectively; and normal serum alkaline phosphatase. He was positive for hepatitis B surface antigen (HBsAg).
Six months later, he presented again, with recurrent streaky hemoptysis. His liver function test results were normal, and he was negative for HBsAg. Similar bronchoscopic findings were noted. During bronchoscopy, he was positioned in the left lateral position, and the bronchoscope was advanced to the opening of the cavity.
Ketoconazole, 400 mg mixed in 10 ml of normal saline solution, was slowly injected into the cavity through the bronchoscope. The bronchoscope was then withdrawn, and the patient was kept in the same position for about 30 min. Over the next 2 days, he coughed out a number of brownish particles averaging about 5 mm in diameter. Histologic examination of these particles showed clusters of fungal hyphae with necrotic tissue.
Repeat bronchoscopy 1 week later showed complete disappearance of the fungus ball. The bronchoscope could be advanced into the cavity, which was lined with granulation tissue. At a few places, golden yellow specks could be seen adhering to its walls. A repeat dose of ketoconazole was injected through the bronchoscope. A follow-up chest radiograph (Fig 2) showed that the mass inside the cavity had disappeared, and the walls of the cavity were well made out. Ketoconazole administration was repeated twice at weekly intervals. There were no complications associated with any of the procedures. No hemoptysis was reported, and no recurrence of the lesion was noted inside the cavity at the 6-month follow-up visit.
DISCUSSION
In patients with aspergilloma, bronchoscopy is usually reserved for identification of the bleeding site prior to the surgery. Bronchoscopic visualization of the fungus ball, as in this case, is very rare.[1,6] We exploited this very observation by adopting an endoscopic approach for treatment.
Medical treatment of aspergillomas has been viewed with skepticism. There have been reports of some success with oral ketoconazole treatment and with percutaneous intracavity instillation of antifungal drugs.[3,5,7] The endobronchial route has been frequently tried for the treatment of aspergilloma. Ramirez[4] reported that mycetoma disappeared or decreased in size with endobronchial instillation of amphotericin B. Ikemoto[8] reported success with intrabronchial instillation of amphotericin B by means of repeated tracheal punctures. Hamamoto et al[9] successfully treated a patient with pulmonary aspergilloma by endobronchial instillation of miconazole with the use of a flexible bronchocatheter. We have found no report of successful treatment of aspergilloma by bronchoscopic instillation of antifungal agents into or near the cavity containing the fungus ball. In the present case, lysis of the fungus ball was achieved rapidly.
We feel that bronchoscopic instillation of an antifungal drug into the segment or subsegmental opening containing the fungus ball is a useful modality in the treatment of a mycetoma, especially in patients who are high-risk candidates for pulmonary resection.
REFERENCES
[1] Smith RL, Morelli MJ, Aranda CP. Pulmonary aspergilloma diagnosed by fiberoptic bronchoscopy. Chest 1987; 92:948-49
[2] Glimp RA, Bayer AS. Pulmonary aspergilloma: diagnostic and therapeutic considerations. Arch Intern Med 1983; 143:303-08
[3] Shale J, Faux JA, Lane DJ. Trial of ketoconazole in non-invasive aspergillosis. Thorax 1987; 42:26-31
[4] Ramirez RJ. Pulmonary aspergilloma: endobronchial treatment. N Engl J Med 1964; 1281-85
[5] Hargis JL, Bone RC, Stewart J, Rector N, Hiller FC. Intracavitary amphotericin B in the symptomatic pulmonary aspergilloma. Am J Med 1980; 68:389-94
[6] Rohatgi PK, Chasse RT. Endoscopic visualization of aspergilloma. Respiration 1991; 58:112-14
[7] Shapiro MJ, Albelda SM, Mayock RL, Mclean GK. Severe hemoptysis associated with pulmonary aspergilloma: percutaneous intracavitary treatment. Chest 1988; 94:1225-31
[8] Ikemoto H. Treatment of pulmonary-aspergilloma with amphotericin B. Arch Intern Med 1965; 115:598-601
[9] Hamamoto T, Watanabe K, Ikemoto H. Endobronchial miconazole for pulmonary aspergilloma [letter]. Ann Intern Med 1983; 98:1030
COPYRIGHT 1993 American College of Chest Physicians
COPYRIGHT 2004 Gale Group