Pain management in the postoperative period usually consists of opioids, other potent analgesics, or both. These medications have been proven to provide good pain control but have a significant number of potential side effects. Some of these side effects include nausea, vomiting, constipation, pruritus, urinary retention, respiratory depression, and sedation. Nonsteroidal anti-inflammatory drugs (NSAIDs) provide anti-inflammatory and analgesic effects, but because most are oral or rectal preparations the ability to use NSAIDs in the postoperative period is limited.
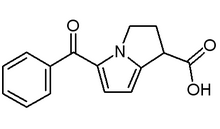
Ketorolac tromethamine is an NSAID that, because of its unique properties, can be administered intravenously, intramuscularly, or orally. Ketorolac has no significant cardiovascular, central nervous system, or autonomic nervous system activity. In addition, ketorolac has an analgesic effect similar to that of the more commonly used opioids and has been shown to be effective in certain postoperative cases. However, because of the normal changes related to volume distribution in gravid patients, its effectiveness in postcesarean patients is questioned. Lowder and associates evaluated the use of ketorolac for postoperative pain management in patients who had undergone cesarean delivery.
The trial was a randomized, double-blind, placebo-controlled study of patients requiring cesarean delivery. Exclusion criteria included patients with bleeding disorders; renal disease; gastrointestinal ulcers, bleeding, or perforation; asthma; known allergy or hypersensitivity to the study drug, aspirin, or other NSAIDs; and breastfeeding status. Patients randomly received ketorolac or placebo soon after the procedure and every six hours for two doses. In addition, they were placed on patient-controlled analgesia (PCA) using various opioids. Pain was assessed every hour for the first four hours after the procedure and then at six, 12, and 24 hours using visual analog scales (VAS). The main outcomes measured included VAS scores, PCA attempts, PCA dosages admin-istered, time to discharge, and preoperative and postoperative hematocrit levels.
The study included 22 patients each in the treatment and placebo arms. The two groups did not differ significantly with regard to demographics, blood loss, or type of anesthesia. In addition, the two groups did not differ with regard to hours of PCA use or time to discharge. Those treated with ketorolac had significant postoperative improvement on VAS scores at two, three, four, six, 12, and 24 hours. When morphine equivalents were compared, patients who received ketorolac had a significantly lower total dosage than those who received placebo. Patients in the placebo group used nearly 50 percent more morphine equivalents than the ketorolac group. When PCA attempts were compared, there was no significant difference between the two groups.
The authors conclude that ketorolac tromethamine is effective in reducing postoperative pain and narcotic use in patients who have undergone cesarean delivery. They add that this medication has been shown to be safe in the postoperative period. They also note that the U.S. Food and Drug Administration currently does not approve the use of ketorolac in breastfeeding patients, even though the American Academy of Pediatrics has found ketorolac to be compatible with breastfeeding.
KARL E. MILLER, M.D. Lowder JL, et al. A randomized, controlled trial to compare ketorolac tromethamine versus placebo after cesarean section to reduce pain and narcotic usage. Am J Obstet Gynecol December 2003;189:1559-62.
COPYRIGHT 2004 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group