Ketorolac is more effective, cheaper, and has fewer side effects
Morphine, titrated intravenously, is the gold standard analgesic for severe pain in emergencies. It is effective and cheap. But morphine has well documented side effects including drowsiness, nausea and vomiting, and respiratory depression. These side effects can be distressing for patients who are already in severe pain and can also interfere with the efficient flow of patients through emergency departments. Staff must spend time observing patients who are experiencing side effects; the length of the patient's stay in the emergency department is prolonged; and some patients need to be admitted for a short time while they recover from the side effects of morphine, thus adding to overall costs.
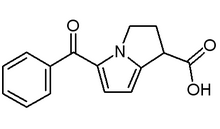
Non-steroidal anti-inflammatory drugs have had the potential to replace opioids in the treatment of severe pain since they became available for use by intravenous injection. The only Cochrane review on this subject shows that non-steroidal anti-inflammatory drugs relieve the pain of renal colic faster when given intravenously than when given by other routes.[1] Ketorolac trometamol given intravenously is as effective as morphine in the management of surgical pain and pain related to cancer, and it has fewer side effects.[2] Gastrointestinal haemorrhage is the most feared risk, but this risk is only slightly higher with ketorolac than with morphine (odds ratio 1.17 (95% CIs 0.99-1.13)); the risk rises sharply if ketorolac is used for more than five days or in patients older than 75 years.[3] Renal problems caused by ketorolac usually resolve when treatment is stopped and should not be an important problem in short term treatment.[2] Yet ketorolac does not seem to have been widely used, probably because of concerns about its cost. The study by Rainer et al (p 1247) in this issue of the journal is, therefore, important because not only does it compare the efficacy of the two analgesics in the emergency setting but costs and benefits as well.[4]
Although small, the study is well designed; the two groups are well matched; and patients had painful injuries. Around two thirds had fractures, including fractures of the femur, tibia, and fibula, not just soft tissue injuries. Ketorolac proved to be as effective as morphine in relieving pain and did so just as quickly. It seemed to have some advantages over morphine in relieving pain associated with activity. This may have practical benefits for patients requiring positioning for radiographs or plaster casts.
As expected, ketorolac produced considerably fewer side effects. Doctors who believe that drowsiness and sleepiness are not so unpleasant, and possibly even desirable for patients with severe pain, may be surprised to find that patients rated ketorolac as significantly better than morphine.
These findings are not unexpected given previous comparisons in other settings. What makes Rainer et al's findings so important is that they address the contentious issue of the added expense of ketorolac. While the cost of the drugs is one factor, it is minor in any overall cost-benefit analysis. Staff time has been shown to be the major driving force in costs in emergency departments, and this was reduced significantly with ketorolac, leading to lower costs overall.[5 6] The more rapid flow of patients through the department could also reduce costs.[7]
Equally important to emergency and primary care physicians is the question of efficiency. With emergency departments in many parts of the world experiencing serious congestion, any intervention that reduces the time patients spend in the department, and the time staff need to devote to them, can only help.[8-10] There is also the question of the quality of care. The significantly shorter time it takes to prepare ketorolac for administration, which was shown in this study and presumably occurs because there is no need for security procedures, should translate into earlier pain relief for patients.
In terms of costs, the main concern raised by this study is the trend towards an excess of admissions among patients given ketorolac. Emergency department costs are only a small part of the overall hospital costs for patients who are admitted, and these patients are much more expensive to treat in emergency departments than patients who are then discharged.[5 6] Thus, even the small increase in the number of admissions that was found to be associated with the use of ketorolac would negate the savings found by Rainer et al. However, the finding of excess admissions is perhaps counterintuitive given the other findings. Patients whose pain is promptly relieved and who recover quickly with few side effects should be more likely to be discharged if their injuries are of the same severity as those given morphine. The authors may be right in suggesting that this trend will disappear in larger studies.
The message from the paper is clear. Clinical evidence from other settings has shown that ketorolac and morphine are equivalent in relieving pain, but there is a distinct benefit favouring ketorolac in terms of side effects. This was not enough to change clinical practice, probably because of the cost of the drug. This latest evidence that the costs and benefits are also likely to favour ketorolac--with the attendant advantages in efficiency, quality of care, and patient satisfaction--should encourage emergency and primary care physicians to use titrated intravenous ketorolac for severe pain in isolated limb injuries. Given its previously reported efficacy as an analgesic for other conditions in the emergency department, the accumulating weight of evidence suggests that intravenous ketorolac will become the analgesic of choice for many emergencies.
[1] Tramer MR, Williams JE, Carroll D, Wiffen PJ, Moore RA, McQuay HJ. Comparing analgesic efficacy of non-steroidal anti-inflammatory drugs given by different routes in acute and chronic pain: a qualitative systematic review. Cochrane Database of Abstracts of Reviews of Effectiveness. The Cochrane Library, 1999. CRD database number: DARE-980293
[2] Gillis JC, Brogden RN. Ketorolac. A reappraisal of its pharmacodynamic and pharmacokinetic properties and therapeutic use in pain management. Drugs 1997;53:139-88.
[3] Strom BL, Berlin JA, Kinman JL, Spitz PW, Hennessy S, Feldman H, et al. Parenteral ketorolac and risk of gastrointestinal and operative site bleeding. A postmarketing surveillance study. JAMA 1996;275:376-82.
[4] Rainer TH, Jacobs P, Ng YC, Cheung NK, Tam M, Lam PKW, et al. Cost effectiveness analysis of intravenous ketorolac and morphine for treating pain after limb injury: double blind randomised controlled trial. BMJ 2000;321:1247-51.
[5] Jelinek GA. Casemix classification of patients attending hospital emergency departments in Perth, Western Australia. Development and evaluation of an urgency-based casemix information system for emergency departments [thesis]. University of Western Australia, 1995.
[6] Erwich-Nijhout MA, Bond MJ, Phillips DG, Baggoley C. The identification of costs associated with emergency department attendances. Emerg Med 1997;9:181-8.
[7] Krochmal P, Riley TA. Increased health care costs associated with ED overcrowding. Am J Emerg Med 1994;12:265-6.
[8] Derlet RW, Richards JR. Overcrowding in the nation's emergency departments: complex causes and disturbing effects. Ann Emerg Med 2000;35:63-8.
[9] Shih FY, Ma MH, Chen SC, Wang HP, Fang CC, Shyu RS, et al. ED overcrowding in Taiwan: facts and strategies. Am J Emerg Med 1999;17:198-202.
[10] Jelinek GA, Baggoley CJ. Financial incentives to change emergency service performance. Med J Aust 1999;171:231-2.
George A Jelinek Professor of emergency medicine
Sir Charles Gairdner Hospital, Nedlands, Western Australia 6009 (g:jelinek@one.net.au)
BMJ 2000;321:1236-7
COPYRIGHT 2000 British Medical Association
COPYRIGHT 2000 Gale Group