AS A KID, Lynne Matallana recalls telling her mother she hurt--a lot. "I was told to rise above it," she says.
She tried but wasn't always successful. "In my teens, I had a lot of problems with my period," she says. "In my 20s, I was diagnosed with irritable bowel syndrome. In my 30s, I had infertility problems." During a laparoscopy, she woke up during the surgery, which seemed to trigger even more distress, including migraines, sleep problems, restless leg syndrome, and overall pain and fatigue.
After seeing 37 doctors, from internists to neurologists to psychiatrists, Matallana was diagnosed with lupus, treated for eight months with steroids--and got worse. Finally, a young physician fresh out of medical school told her she had fibromyalgia, a chronic condition characterized by fatigue and pain in the tissues of the muscles, ligaments, and tendons.
Fibromyalgia affects between 3 million and 6 million Americans, according to the American College of Rheumatology. Matallana, now 50 and the president and co-founder of the National Fibromyalgia Association based in Orange, Calif., puts the figure as high as 10 million.
The exact cause of the condition isn't known. Those with a family member having the condition are more likely to develop it, as are those with rheumatic diseases. Other contributing factors are thought to include infections, sleep disturbances, abnormalities of the sympathetic nervous system, chemical alterations in the brain, changes in muscle metabolism, hormonal shifts, psychological stress, and/or an injury or trauma.
While there is no cure, people do get well enough to lead full, balanced lives. The key, Matellana explains, is to find the right blend of treatments. Her own recovery regimen focuses on exercise, massage, adequate sleep, and a healthy diet, as well as painkillers and sleeping pills when necessary. "Within a few months of getting the diagnosis, I could tell things were going to get better," says Matellana, who now has enough energy to work a 60-hour week.
Do you have it?
FIBROMYALGIA is an "energy crisis" in the body, declares Jacob Teitelbaum, M.D., director of the Annapolis Center for Effective Chronic Fatigue Syndrome/ Fibromyalgia Therapies. It comes with a laundry list of symptoms, including:
* widespread pain
* fatigue
* sleeplessness
* headaches
* irritable bowel syndrome
* painful menstrual periods
* numbness or tingling in the extremities
* memory problems
* sensitivity to heat or cold
* depression
The frequent presence of depression has led some doctors to dismiss fibromyalgia as purely psychological. But that tendency is diminishing, observes Robert Lahita, M.D., professor of medicine at Mr. Sinai Medical School in New York and chair of medicine at Jersey City Medical Center in New Jersey. "I think more doctors now identify fibromyalgia as a real illness," he says. "I know it's a real illness by my way of thinking."
To aid physicians and patients alike, the ACR has identified 18 "tender points" located in pairs around the neck, shoulders, joints, and pelvis (see page 52). A diagnosis of fibromyalgia can be established if extensive pain has lasted for 90 days or more and at least 11 of the tender points cause pain when 4 kilograms (8.8 pounds) of pressure are applied.
Medical approaches
THERE'S ONE BIG PROBLEM with FDA-approved prescription medications for fibromyalgia. Technically, there aren't any.
"There are no drugs indicated specifically by the FDA for fibromyalgia, so they're prescribed 'off-label,'" says Kim Dupree Jones, R.N., Ph.D., an assistant professor and nurse practitioner at Oregon Health & Science University Schools of Nursing and Medicine in Portland. Non-narcotic painkillers (such as Ultram and Ultracet), sleep aids (Ambien), muscle relaxants (Valium, Klonopin), and inflammation fighters (Advil, aspirin) are sometimes used, based on individual needs.
"I start patients on a program of aerobics, and provide them with an analgesic for pain," says Lahita. "If they are having sleep problems, I put them on a tricyclic antidepressant or one of the other new drugs such as Cymbalta."
Two medications may soon be approved for fibromyalgia: Cypress Bioscience's milnacipran, which boosts the hormone norepinephrine, and Pfizer's pregabalin (Lyrica), already in use for pain associated with diabetic peripheral neuropathy.
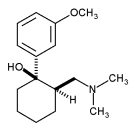
Two more promising treatments are best known as ingredients in over-the-counter cough syrups: guaifenesin and dextromethorphan. R. Paul St. Amand, M.D., an assistant clinical professor of medicine at Harbor-UCLA Medical Center in Torrance, Calif., and author of What Your Doctor May Not Tell You About Fibromyalgia, theorizes that people with the syndrome have a genetic anomaly that inhibits the excretion of phosphates, which build up and block energy production--and that taking 300-milligram supplements of guaifenesin twice a day, generally going up to 600 mg twice a day, promotes the elimination of phosphates. (Patients must avoid a long list of salicylates, including aspirin; see guaidoc.com for details.)
There is some debate here. Robert Bennett, M.D., a professor of medicine at Oregon Health and Science University, evaluated guaifenesin use in fibromyalgia patients; after one year, he found that it was no more effective than a placebo. The National Fibromyalgia Association suggests that patients first try other, clinically effective remedies, but acknowledges guaifenesin could be useful.
As for dextromethorphan, in a study at the University of Florida, it reduced what's known as the "wind up," the snowballing pain response in fibromyalgia patients to minor, repetitive physical contact. Previous research has demonstrated that dextromethorphan blocks the action of a chemical messenger called N-methyl-D-aspartate, which relays pain impulses in the spinal cord. The investigators cautioned people not to self-medicate with dextromethorphan, which can cause confusion at high doses. Similarly, St. Amand warns patients not to use cough mixtures to obtain guaifenesin.
"Right now, the most promising treatment approach is a cocktail of the fewest number of drugs at the lowest dose plus lifestyle changes and stress management," says Dupree Jones.
Natural therapies
IN A MAYO CLINIC SURVEY, 98 percent of the 289 fibromyalgia patients polled said they had used some sort of complementary or alternative medicine. Among the preferred options:
Supplement Formulas
Herbal and dietary supplements can increase energy and minimize fatigue, says Teitelbaum, whose own bout with fibromyalgia started after he contracted a "drop-dead" flu in 1975. He has since authored two books on the subject, and launched a line of supplements available at endfatigue.com. (All royalties are donated to charity.) For sleep problems, he recommends a mixture of herbs: "wild lettuce, Jamaican dogwood, theanine, hops, valerian, and passion flower." For energy, there is a B-complex-based capsule and a drink mix dubbed the Energy Revitalization System that encompasses about 35 important nutrients.
Magnesium and Malic Acid
Because magnesium deficiency has been associated with muscle pain, supplementing can be beneficial. Magnesium combined with malic acid relieved pain and tenderness, according to a study in the Journal of Rheumatology. "Malic acid is a compound that occurs naturally in foods, in fruits in general, and in especially high levels in apples," notes Teitelbaum. "When levels of malic acid are low, the body often has to shift to a very inefficient means of generating energy. This contributes to an abnormal buildup of lactic acid, which can cause muscle pain, achiness, and fatigue." Endfatigue.com offers a powder formula with magnesium and malic acid; an alternative is Fibrocare tablets: Teitelbaum recommends taking two tablets two to three times a day for eight months, and then decreasing to two tablets a day. (Take less if GI upset results.)
Coenzyme Q10 and Ginkgo Biloba
This combination improved quality of life in 64 percent of subjects with fibromyalgia, according to a study published in The Journal of International Medical Research. The subjects took 200 mg of coenzyme Q10 and 200 mg of ginkgo biloba extract daily for 84 days before noting changes.
Acetyl-L-carnitine
Some fibromyalgia sufferers have low levels of acylcarnitine, which plays a crucial role in the body's energy production. Teitelbaum says that taking 500 mg to 1,000 mg of acetyl-L-carnitine (not L-carnitine) daily for eight to 12 weeks can be very helpful.
Essential Fatty Acids
An adequate intake of EFAs from vegetables and fish oil is necessary for the production of series 1 and 3 prostaglandins, which reduce inflammation and improve mood. (Series 2 prostaglandins, produced from animal fats, increase inflammation.) Supplementing with fish oil, flaxseed oil, and/or evening primrose oil can help correct EFA deficiencies.
Ginger
This natural anti-inflammatory can relieve muscle and joint pain, and may inhibit substance P, a pain mediator that's elevated in people with fibromyalgia. A study published in Medical Hypotheses found that taking 1,000 mg of powdered ginger daily reduced muscle pain; tripling the dose brought quicker and better relief, says Teitelbaum.
Essential Oils
Newly available in the United States is 024 Fibromyalgia, a Canadian topical formula that mixes seven essential oils. In a pair of company-sponsored studies, fibromyalgia patients who applied 024 three times a day for five days reported significant pain relief; in a study at Sunnybrook & Women's College Health Sciences Centre in Canada, patients who used 024 for one month reported measurable reductions in pain.
Exercise
Regular physical activity has been shown to improve the health of patients with fibromyalgia. In a review of several studies, published this year in the journal Current Opinion in Rheumatology, the authors found that brisk walking, pool exercise, and other mild aerobic activity improved symptoms and lowered distress.
Massage
"Massage is a mixed blessing: For some it hurts, for some it's good," says Dupree Jones. "It's important to find a massage therapist you trust, one who understands the disease and is careful not to hurt you." Starting from the knees down only works well for some patients.
Trager
This gentle technique of neuromuscular re-education "has been very beneficial for my more severe fibromyalgia patients," says Teitelbaum. (For details, see "Sway Away Headaches," page 96.) Other physical and movement therapies with good results include acupuncture, chiropractic, and yoga.
Acupressure
The Thera Cane (theracane.net) is a curved cane with rubber-tipped extensions that enables patients to use pressure to manipulate painful knots within the muscle. "There are no studies, but many patients love it," says Dupree Jones. "Some people put it on the tender points."
Hypnotherapy
In one session that lasts several hours, Viviane Oberhand, a certified hypnotherapist in Los Angeles, uses related techniques called Neurolinguistic Programming and Time Line Therapy to take doctor-referred clients back to "the root of the trigger" that spawned their pain, helping the client release it without re-experiencing past trauma. "During the session, a shift happens and people let go of their negative emotions at the root--and the pain of fibromyalgia is gone," she says.
Attitude Adjustment
No matter which mix of treatments proves best, adopting a positive but realistic attitude might be the most important tool, says Frances Emma Jenkins, 49, of Manhattan Beach, Calif. After two car accidents, which may have triggered her fibromyalgia, this busy career woman's life became a blur of pain.
Now Jenkins takes painkillers only when needed and leads a healthy lifestyle. But her optimistic outlook aids her just as much. "My mind and my heart are going to control me, not the pain," she says. "The real power is in your mind. You can make it through each day. You may have pain, but don't let the pain imprison you. You have to have a vision for life, and you have to allow the vision to supercede your pain."
For more information, contact the National Fibromyalgia Association (fmaware.org) and the National Institute of Arthritis and Musculoskeletal and Skin Diseases (niams.nih.gov).
COPYRIGHT 2005 Weider Publications
COPYRIGHT 2005 Gale Group