* EVIDENCE-BASED ANSWER
Tramadol (Ultram, generic and with acetaminophen in Ultracet) carries a risk of substance abuse (strength of recommendation [SOR]: B, based on case report surveillance programs). While it appears that tramadol's risk of substance abuse is low (SOR: B, based on case report surveillance programs), tramadol is associated with a withdrawal syndrome usually typical of opioid withdrawal (SOR: B, based on case report surveillance programs, and a prospective descriptive study).
* EVIDENCE SUMMARY
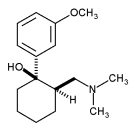
Tramadol is a novel, central-acting synthetic opioid with weak mu-opioid activity, and is approved for treatment of moderate to moderately severe pain in adults. Anecdotally, some clinicians have assumed this popular analgesic's nonscheduled status under the Controlled Substance Act (CSA) means tramadol has no substance abuse potential. (The term "abuse" herein denotes substance abuse or dependence.)
Evidence of tramadol abuse in the US comes primarily from federally operated programs collecting adverse drug event (ADE) data. The MedWatch program of the Food and Drug Administration (FDA) provides a central depository for receiving and compiling postmarketiug voluntary case reports. While passive reporting systems can significantly underestimate serious ADE numbers, these reports are often the first evidence of an ADE after a new drug's release into the market. (1) MedWatch has received 766 case reports of abuse associated with tramadol, as well as 482 cases of withdrawal associated with tramadol from the drug's initial US marketing in 1995 through September 2004. (2,3)
The Drug Abuse Warning Network (DAWN) is a federally operated, national surveillance system that monitors trends in drug-related emergency department visits. Over the period from 1995 to 2002, DAWN reported drug-related emergency department visits mentioning tramadol in more than 12,000 cases. Tramadol case numbers significantly increased 165% during this time. For perspective, during the same period, DAWN found nalbuphine (Nubain, also not CSA scheduled) in 118 cases, propoxyphene drug combinations (CSA Class IV) in more than 45,000 cases, codeine drug combinations (CSA Classes III & V) in about 50,000 cases, and hydrocodone drug combinations (CSA Class III) in around 128,000 cases. (4)
Using data from observational postmarketing studies, investigators have extrapolated a tramadol abuse rate for the general tramadol-exposed population. (5,6) Ortho-McNeil, Ultram's manufacturer, funded a surveillance program that compiled tramadol abuse and withdrawal case reports from 2 sources: (1) periodic surveys for tramadol abuse case reports from a group of 255 substance abuse experts studying and caring for addiction communities, and (2) voluntary ADE case reports from health care professionals and consumers received by Ortho-McNeil. Over 3 years of surveillance, the program received 454 case reports classified as tramadol abuse. Over 5 years of surveillance, 422 cases of substance withdrawal, with primarily opioid withdrawal symptoms, were reported. There are significant threats to the validity and generalizability of the investigators' estimated abuse rate of 1 to 3 cases per 100,000 tramadol-exposed patients. The abuse cases were collected in nonrepresentative samples of the tramadol-exposed population. Tramadol exposure is likely suppressed in addiction communities with access to preferred, more potent or euphoriant opioids than tramadol. Voluntary case reports of tramadol abuse significantly underestimate the actual number of abuse cases in the tramadol-exposed population. In addition, the low survey return rate (49%) further decreases the accuracy of any estimation of tramadol abuse rates.
Prospective studies among patients with known abuse, or at high risk of abuse, reported a tramadol abuse rate, as well as subjective experiences of tramadol withdrawal. A 3-year post-marketing cohort study measured tramadol's nonmedical misuse rates using urine drug testing for tramadol among 1601 participants in 4 US state monitoring programs for impaired healthcare professionals. (7) Tramadol exposure occurred in 140 (8.7%) participants. Thirty-nine (28%) were classified as extensive experimentation or abuse of tramadol. Overall, the rate of extensive experimentation or abuse was 18 cases per thousand person-years. The Hawthorne effect, where awareness of being monitored alters a subject's behavior, may threaten these measured frequency rates' generalizability. Another prospective study assessed the subjective tramadol withdrawal experience in 219 patients with a diagnosis of "Tramadol misuse" who were attending 6 drug detoxification centers in China. (8) Validated drug dependence symptom scales found that while the degree of physical dependence reported was uniformly mild, the majority of patients reported the psychic dependence symptom of tramadol craving.
The FDA's Drug Abuse Advisory Committee performed a formal review of the tramadol abuse evidence in 1998, including the data from Ortho-McNeil's surveillance studies and federal case reporting/surveillance programs. The FDA did not recommend changing tramadol's unscheduled status. (9) The FDA's considered decision to not schedule tramadol as a controlled substance implies its abuse risk to the general population is low in comparison to its novel analgesic benefit.
* RECOMMENDATIONS FROM OTHERS
Ortho-McNeil's revised 2001 product package insert for Ultram states, "Tramadol may induce psychic and physical dependence of the morphine type (mu-opioid). Dependence and abuse, including drug-seeking behavior and taking illicit actions to obtain the drug are not limited to those patients with prior history of opioid dependence" (italics in original, emphasizing 2001 addition). The risk for patients with a history of substance abuse has been observed to be higher. (10)
REFERENCES
(1.) Brewer T, Colditz GA. Postmarketing surveillance and adverse drug reactions: current perspectives and future needs. JAMA 1999; 281:824-829.
(2.) Brinker A, Bonnel RA, Beitz J. Abuse, dependence, or withdrawal associated with tramadol. Am J Psychiatry 2002; 159:881-882.
(3.) Adverse Event Reporting System. Freedom of Information Report. Rockville, Md: Office of Drug Safety, Food and Drug Administration: search November 1997 to September 2004.
(4.) Drug Abuse Warning Network. Emergency Department Trends From DAWN: Final Estimates 1995 to 2002. Available at: dawninfo.samhsa.gov. Accessed on August 25, 2004.
(5.) Cicero TJ, Adams EH, Geller A, et al. A postmarketing surveillance program to monitor Ultram (tramadol hydrochloride) abuse in the United States. Drug Alcohol Depend 1999; 57:7-22.
(6.) Senay EC, Adams EH, Geller A, et al. Physical dependence on Ultram (tramadol hydrochloride): both opioid-like and atypical withdrawal symptoms occur. Drug Alcohol Depend 2003; 69:233-241.
(7.) Knisely JS, Campbell ED, Dawson KS, Schnoll SH. Tramadol post-marketing surveillance in health care professionals. Drug Alcohol Depend 2002; 68:15-22.
(8.) Liu ZM, Zhou WH, Lian Z, et al. Drug dependence and abuse potential of tramadol. Zhongguo Yao Li Xue Bao 1999; 20:52-54.
(9.) FDA Drug Abuse Advisory Committee. The Scientific Evidence for Initiating a Scheduling Action for Ultram (tramadol hydrochloride). 1998. Available at: www.fda.gov._
(10.) Murray L, ed. Physicians' Desk Reference. 58th ed. Montvale, NJ: Thomson PDR; 2004:2496.
* CLINICAL COMMENTARY
Though it may not have high abuse potential, prescribe tramadol cautiously
Although tramadol appears to have a low potential for abuse, the literature does reveal evidence of abuse, addiction, and withdrawal, even in patients without a history of such problems. We do not know if tramadol is less addictive than other narcotics in high-risk patients. For patients at risk for dependence, tramadol is a reasonable alternative to other opioids, but abuse appears more likely in these patients. Tramadol may be most appropriate for treatment of acute painful conditions, but it can be administered chronically under a watchful eye. Providers should prescribe it cautiously, particularly in patients with a history of abuse or addiction, at least until more definitive evidence surfaces.
David M. Schneider, MD, Sutter Medical Center Family Practice Residency Program, Santa Rosa, Calif
Todd McDiarmid, MD, Leslie Mackler, MSLS, Moses Cone Health System, Greensboro, IVC
COPYRIGHT 2005 Dowden Health Media, Inc.
COPYRIGHT 2005 Gale Group