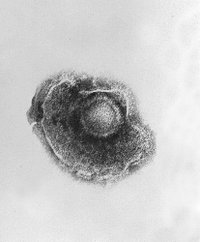
Varicella is a highly contagious condition manifested by fever and a three- to five-day centripetal rash. Vasquez reviewed the current state of varicella epidemiology and vaccination.
Experts recommend live attenuated varicella zoster vaccine for healthy susceptible children (12 months and older), adolescents, and adults because of its 96 to 100 percent efficacy rate. Over the past nine years, widespread use of the varicella vaccine has substantially decreased the rates of chickenpox and vaccine-related complications. Vaccinated persons develop milder symptoms with fewer skin lesions, which are more likely to be macular than vesicular. Residual scarring also is less common. However, atypical cases are making the diagnosis of varicella more difficult. Recent varicella exposure is the most useful clinical diagnostic hint because demonstration of viral antigen in skin scrapings or vesicular fluid is rarely available to the physician. It also is important to exclude similarly presenting conditions (see accompanying table) and to note that breakthrough varicella infection can be communicated to susceptible persons.
The long-term efficacy of the varicella zoster vaccine; the age at which it should be administered; and its use with the measles, mumps, and rubella (MMR) vaccine are controversial. Although postvaccine antibody levels are lower than those following natural infection, the varicella vaccine offers up to eight years of protection. Immunity in vaccinated children may be boosted naturally by subclinical infection. However, small outbreaks of chickenpox in vaccinated children have caused some to suggest that boosters are necessary to maintain long-term effectiveness.
Vaccination may be less effective in children younger than 15 months. However, because children 12 to 15 months of age are at risk and may not return at a later age for vaccination, the present recommendation remains to vaccinate at 12 months of age. Studies have found that children given a varicella vaccine within 30 days or less of receiving an MMR vaccine are at an increased risk of developing breakthrough varicella infection. Therefore, guidelines suggest separating the MMR and varicella zoster vaccines by 28 days if not given simultaneously.
The author concludes that varicella vaccination is highly effective in preventing infection and, although breakthrough infections can occur, varicella eradication is an attainable goal.
Vazquez M. Varicella infections and varicella vaccine in the 21st century. Pediatr Infect Dis J September 2004;23:871-2.
EDITOR'S NOTE: In another article (1) written by Vazquez, expanded recommendations for varicella zoster vaccination are presented. The Advisory Committee on Immunization Practices and the American Academy of Pediatrics recommend vaccinating certain immunocompromised children (e.g., asymptomatic children infected with human immunodeficiency virus) and use of the vaccine for postexposure prophylaxis. (2)--S.S.
REFERENCES
(1.) Vazquez M. Varicella zoster virus infections in children after the introduction of live attenuated varicella vaccine. Curr Opin Pediatr 2004;16:80-4.
(2.) American Academy of Pediatrics Committee on Infectious Diseases. Varicella vaccine update. Pediatrics 2000;105:136-41.
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2005 Gale Group