More than 90 percent of U.S. adults have serologic evidence of varicella-zoster virus infection and are at risk for subsequent reactivation, in the form of herpes zoster (shingles). The reactivation complication most feared by patients is post-herpetic neuralgia (PHN), a condition of chronic neuropathic pain in the dermatome where reactivation occurred. Gnann and Whitley review the diagnosis and treatment of herpes zoster and discuss the controversial topic of corticosteroid use.
Increasing age is a key risk factor for virus reactivation. The incidence of shingles increases fivefold in persons 75 years and older compared with the general population. Reactivation is also more common among immunosuppressed persons (e.g., persons infected with human immunodeficiency virus, chronic steroid users, organ transplant recipients).
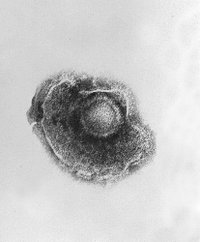
Shingles usually begins with paresthesias that can vary from mild itching to severe pain. A maculopapular rash appears in a dermatome that progresses over days to clusters of clear vesicles and then crusted lesions. Healing typically occurs over two to four weeks and can permanently scar the affected area. PHN is defined as pain persisting for more than 30 days after the onset of the rash. The reported rates vary widely; from 8 to 70 percent of patients with shingles are affected. Increasing age also is associated with higher rates of PHN, with one study quoting a pain prevalence 27-fold higher in patients 50 years and older compared with younger patients, at 60 days post-rash. Severe complications associated with shingles include disseminated disease (e.g., pneumonitis, encephalitis, hepatitis) and acute retinal necrosis. Although more common in immunocompromised persons, severe complications also may occur in patients with normal immune systems.
It has been well established in placebo-controlled trials that antiviral therapy with acyclovir, valacyclovir, or famciclovir decreases the number of skin lesions and the pain experienced with shingles. Valacyclovir and famciclovir are preferred over acyclovir in the treatment of herpes zoster because they have better pharmacokinetic properties and simpler dosing regimens.
The two largest controlled trials of steroids used concomitantly with antiviral therapy for herpes zoster demonstrated faster rates of cutaneous healing and a reduction in acute pain, but no benefit in the incidence or duration of PHN.
Although treatment for shingles is sometimes believed to be optional in younger patients who have uncomplicated shingles, the authors recommend treatment in all older and immunocompromised patients and those with eye involvement. Patients with a larger area of skin involvement and more severe pain at presentation have a higher risk for PHN and also should be considered for treatment.
2002;347:340-6.
COPYRIGHT 2003 American Academy of Family Physicians
COPYRIGHT 2003 Gale Group