Background: The use of anticoagulant therapy is expanding among the elderly population, in part because of the increasing prevalence of atrial fibrillation. Published data describing the warfarin maintenance dose requirements for this age group are limited. Because warfarin therapy is often initiated in the outpatient setting where significant barriers to daily monitoring exist for this patient population, a better understanding of the factors that predict lower dose requirements may reduce the risk of unanticipated overanticoagulation and hemorrhage.
Objective: To define the effects of age and gender on the warfarin maintenance dose among ambulatory adult patients with an international normalized ratio target between 2.0 and 3.0.
Design: Prospective cohort study and retrospective cohort secondary data source. Setting: One hundred one community-based physician practices with dedicated warfarin management systems and an academic medical center anticoagulation clinic.
Patients: A total of 4,616 patients comprised the prospective cohort, and 7,586 patients comprised the retrospective cohort. Of the 12,202 patients, 2,359 were [greater than or equal to] 80 years of age.
Measurements: Median weekly and daily maintenance warfarin dose.
Results: The warfarin dose was inversely related to age and was strongly associated with gender. The median weekly dose ranged from 45 mg (6.4 mg/d) for men who were < 50 years of age to 22 mg (3.1 mg/d) for women [greater than or equal to] 80 years of age. The weekly dose declined by 0.4 mg/yr (95% confidence interval [CI], 0.37 to 0.44; p < 0.001) and women required 4.5 mg less per week than men (95% CI, 3.8 to 5.3; p < 0.001). Among patients who were > 70 years of age, the often-suggested initiation dose of 5 mg/d will be excessive for 82% of women and 65% of men.
Conclusions: Warfarin dose requirements decrease greatly with age. Older women require the lowest warfarin doses. These observations suggest that, when warfarin is being initiated, the commonly employed empiric starting dose of 5 mg/d will lead to overanticoagulation for the majority of patients in the geriatric age group; lower initiation and maintenance doses should be considered for the elderly.
Key words: anticoagulation; warfarin
Abbreviations: CI = confidence interval; INR = international normalized ratio
**********
The number of elderly patients who are eligible to receive warfarin is steadily expanding, in part because of the increasing prevalence of atrial fibrillation. (1) Atrial fibrillation affects approximately 10% of individuals who are [greater than or equal to] 80 years of age, and it is projected that 4 million individuals in the United States will have atrial fibrillation by the year 2030. (2) Both the risk of stroke in patients with atrial fibrillation and the risk of mortality in patients who experience a stroke increase with age. (3) Warfarin therapy reduces the risk of stroke in patients with atrial fibrillation by 68%.4 However, despite evidence that the benefit of anticoagulation therapy is greatest in patients who are > 75 years of age, advanced age independently predicts warfarin nonuse. (5-8) Warfarin is likely to remain the only widely available oral anticoagulant agent for the foreseeable future.
The fear of hemorrhage and the anticipated difficulty with the control of antieoagulation therapy have been cited as reasons for not prescribing warfarin to elderly patients. (9) Compared to younger patients, older individuals exhibit an enhanced dose response to warfarin, are more likely to become overanticoagulated, and take longer to return to safe international normalized ratio (INR) levels when they have a supratherapeutie INR. (10-16) Furthermore, increasing age and elevated INR have been shown to be risk factors for bleeding among patients receiving anticoagulant therapy. (17-20)
Currently, few data are available to guide clinicians in the dosing of warfarin therapy for the very elderly. The largest published data set included patients who were treated to achieve different target INR intensities and included only 143 individuals who were [greater than or equal to] 80 years of age. (16) An article from The Seventh American College of Chest Physicians Consensus Conference on Antithrombotic and Thrombolytic Therapy (21) stated that "a starting dose of < 5 mg might be appropriate in the elderly," but did not make specific recommendations for the geriatric population. Although prediction models (22) of the maintenance warfarin dose have been published, it is not clear that octogenarians were well-represented in the derivation cohorts, and these models are not easily applied in all clinical settings. Similarly, warfarin initiation nomograms are largely based on younger patients. (23) Two other published nomograms (24,25) incorporated adjustments for age, but were derived from study populations that included only 11 patients who were [greater than or equal to] 80 years of age and 30 patients who were > 75 years of age. Warfarin nomograms are limited not only by the paucity of older patients included in the cohorts from which they were derived, but also by their reliance on daily or alternate-day monitoring of the INR. Such frequent laboratory testing represents a significant burden and may be unrealistic for many elderly patients who are initiating warfarin therapy. Compared to younger patients, older patients are more often dependent on others for transportation and are challenged by physical limitations to mobility. These impediments to frequent testing are especially relevant for those patients who live in less densely populated areas or in less developed countries. An awareness of these common, practical access barriers has prompted the authors of at least one guideline (26) to recommend INR testing "at least weekly during the initiation of oral anticoagulant therapy."
Because warfarin dose requirements are known to decrease with age, the often-suggested empiric starting dose of 5 mg/d will likely result in supratherapeutic INR values for many elderly patients. Systematic overdosing of patients who are [greater than or equal to] 80 years of age may partly explain the observation that the risk for major hemorrhage is highest in older patients and in the early phase of therapy. (27,28)
Given the practical barriers that may limit the use of initiation nomograms, and the uncertainty about whether prediction models and nomograms can be generalized to patients who are > 80 years of age, we sought to describe warfarin maintenance dosing patterns that were experienced in the clinical care of two large, independent, ambulatory patient populations. We have provided the distribution of the warfarin maintenance dose by age, gender, and indication. Additional knowledge of warfarin dose requirements for very elderly individuals will help physicians with empiric dosing decisions. A more informed decision about dosing will likely decrease the risk of excessive anticoagulation, particularly among those patients for whom daily testing is not possible.
MATERIALS AND METHODS
Study Populations
A prospective cohort was assembled as part of a larger study assessing anticoagulation care in the United States. Sites were invited to participate by letter and through a study web site. MI enrolled sites had at least one dedicated provider managing warfarin therapy, usually within the setting of a community-based physician group office practice. Patients were invited to participate at the time of their routine appointment. Study enrollment began in August 2000 and ended in February 2002. All study participants provided written informed consent. During the study period, 6,761 patients were enrolled into the study from 101 sites in 38 states. We included those patients who were [greater than or equal to] 18 years of age, had a physician-specified INR target range of 2.0 to 3.0, and had achieved a stable warfarin dose during the observation period. Health-care personnel (typically, a nurse or pharmacist dedicated to anticoagulation therapy management) from the participating clinic made these decisions.
Encrypted patient-derived data from each site were transmitted weekly to an independent data-coordinating center (McKessonHBOC BioServices; Rockville, MD). Missing data fields and data-entry errors were flagged and resolved prior to data transfer. Study investigators were blinded to the identification and location of the participating practices and patients. Nearly all sites had experience using the designated data-entry system (CoumaCare; Bristol-Myers Squibb; Princeton, NJ) before the study began. The designated software program has been used by many anticoagulation therapy management services for clinical purposes (eg, patient tracking, data entry, and record keeping). The software does not make dosing or follow-up recommendations.
Variables of interest included age, gender, ethnicity, indication for oral anticoagulant therapy, physician-specified INR target range, INR values and dates of testing, warfarin dose at each visit, and the presence of other medical diagnoses, specifically, COPD, coronary artery disease, diabetes mellitus, heart failure, hypertension, hyperlipidemia, active malignancy, and prior stroke. The effect of amiodarone was specifically sought out because of the magnitude of its potentiating effect on warfarin. (29-31) Patient weight was routinely recorded in seven of the participating sites. The relationship between weight and gender was explored within this subset of patients.
Retrospective Cohort Secondary Data Source
We additionally assessed the effects of age and gender on warfarin dose in an independent cohort of ambulatory patients who were managed at the Anticoagnlation Therapy Unit of Massachusetts General Hospital. We included all patients who were [greater than or equal to] 18 years of age, had a specified INR target range of 2.0 to 3.0, were followed up during the period from 1993 to 2003, and had achieved a stable warfarin dose. The available data for this cohort included age, gender, indication for oral anticoagulant therapy, INR values, dates of testing, and warfarin dose prescribed. The retrospective cohort decisions about warfarin dosing and follow-up were made by nurses employed in the Anticoagnlation Therapy Unit at the Massachusetts General Hospital.
Statistical Analysis
We defined a stable warfarin dose as a dose that was prescribed twice consecutively after two consecutive in-range INR measurements (ie, 2.0 to 3.0). For each patient, we used the first stable dose observed. The median warfarin dose was calculated across gender and decade of age. Univariate comparisons were performed using t tests and rank sum tests. Nonparametric tests for trend were used to assess the change in median dose with age. (32)
We assessed the independent effects of age and gender for the prospective cohort using multiple linear regression. Variables with the potential to influence the maintenance warfarin dose were included in the model if the p value was < 0.1 in the univariate analysis. A two-sided p value of < 0.05 was considered to be statistically significant. The final model included terms for age, gender, coronary artery disease, diabetes mellitus, heart failure, hypertension, amiodarone use, and venous thromboembolic disease. Analyses were performed using a statistical software package STATA software; (STATA Corp; College Station, TX). For the subset of patients with weight available, we present the median dose and age for men and women stratified by weight to better illustrate the relationships among these variables.
Human Studies Approval
The Western Institutional Review Board (Olympia, WA) provided approval of the registry protocol and the informed consent form. Each participating site director was responsible for obtaining internal human studies approval, if locally required, and to provide evidence that these requirements had been met before the site was enrolled. The study protocol was also approved by the institutional review board at Massachusetts General Hospital.
Role of the Funding Source
The funding source had no role in the collection, analysis, or interpretation of the data, or in the decision to submit the study for publication.
RESULTS
Prospective Cohort
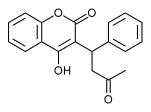
A total of 4,616 patients met the study inclusion criteria. The mean age was 72 years, and 58% of patients were men (Table 1). There were 1,127 patients who were [greater than or equal to] 80 years of age. Sixty-two percent of the cohort was receiving warfarin therapy for stroke prevention in atrial fibrillation, and 15% for venous thromboembolic disease. The maintenance warfarin dose was significantly greater for men compared to women (30 vs 25 mg/wk, respectively; p < 0.0001). Trends of decreasing dose with increasing age were significant overall and within each gender (all p < 0.01) [Fig 1]. The decrements in the median weekly maintenance warfarin dose between the youngest age group (ie, < 50 years) and the oldest age group (ie, [greater than or equal to] 90 years) were 47% for women and 39% for men.
[FIGURE 1 OMITTED]
Similar relationships between both warfarin dose and age, and warfarin dose and gender were seen in patients with atrial fibrillation and in those with venous thromboembolic disease (Table 2). Within each indication, younger men required the highest doses (median daily dose: for atrial fibrillation, 5.4 rag; for venous thromboembolic disease, 6.4 mg), and women who were [greater than or equal to] 80 years of age required the lowest doses (median daily dose: for atrial fibrillation, 3.1 mg; for venous thromboembolic disease, 3.6 mg). Based on our study population, the often-recommended initiation dose of 5 mg/d would exceed the maintenance warfarin dose requirement for approximately 65% of women 60 to 69 years of age, 79% of women 70 to 79 years of age, and 84% of women [greater than or equal to] 80 years of age (Table 3).
The effects of age and gender were independent and did not change in magnitude after controlling for comorbid illness and amiodarone use. For each year of age, the weekly warfarin dose declined by 0.4 mg (95% confidence interval [CI], 0.37 to 0.44 mg; p < 0.001). At any given age, the weekly warfarin dose for women was 4.5 mg lower (95% CI, 3.8 to 5.3 mg; p < 0.001) than that of men. Amiodarone use was associated with a reduction of 7.3 mg/wk (95% CI, 5.2 to 9.5 mg/wk; p < 0.001) in warfarin maintenance dose. Other less potent factors that were independently associated with warfarin dose included heart failure, coronary artery disease, and diabetes mellitus (Table 4).
Retrospective Cohort
The retrospective cohort consisted of 7,586 patients, 1,232 of whom were [greater than or equal to] 80 years of age. The median daily doses by age and gender for patients with atrial fibrillation or venous thromboembolic disease are presented alongside those of the prospective cohort in Table 2. Similar patterns of change in the median dose by age for women and men were evident in the two cohorts (Fig 1). The proportion of patients requiring a dose of < 35 mg/wk approximates that of the prospective cohort (Table 3).
Relationship of Gender and Weight to Maintenance Warfarin Dose
We examined the median warfarin dose by gender-stratified deciles of weight in the subset of 369 patients from the seven sites where weight was routinely recorded. The sample size was too small for significant dose comparisons within each stratum; however, in seven of the nine weight classes women required lower doses. There was no significant difference in mean age between genders for these strata (Table 5). The exceptions to this trend were the weight class of 150 to 159 lbs, in which the higher dose among women may be explained by the fact that the women were significantly younger than the men (p = 0.017), and the heaviest weight class (ie, those weighing > 234 lbs).
DISCUSSION
A limited amount of data on the dosing of warfarin in an elderly population has been published. The largest such study included only 143 individuals who were [greater than or equal to] 80 years of age and included patients who had been treated to achieve various target intensities. Existing data that form the basis of the current Guidelines (21,23) were largely obtained from younger cohorts. In this study, we report on the maintenance warfarin dose of 12,202 ambulatory outpatients with an INR target range of 2.0 to 3.0. We provide the warfarin dosing experience of 2,359 individuals who were [greater than or equal to] 80 years of age. We were able to assess the independent effects of age and gender through multiple linear regression models that controlled for medical conditions that are prevalent in this population and the known powerful effect of amiodarone.
We found highly significant associations between warfarin dose and age, and warfarin dose and gender in two large cohorts. For each additional year of age, the weekly warfarin dose declined by 0.4 mg. At any given age, the mean weekly warfarin dose for women was 4.5 mg lower than that for men. Among patients with atrial fibrillation as the indication for warfarin therapy, the median daffy dose ranged from 5.4 rag, for men aged 50 to 59 years of age, to 3.1 mg, for women [greater than or equal to] 80 years of age. These findings have important implications for patient safety and quality of anticoagulation control in the outpatient setting where daily or alternate-day monitoring of the INR is not always possible. Based on the actual warfarin maintenance doses observed in our study populations, the often-recommended 5 mg daily warfarin starting dose would be too high for up to 82% of women (and 65% of men) who were > 70 years of age. Thus, our data suggest that the higher rates of bleeding and erratic INR values that have been reported (17-20) in the early phase of warfarin therapy may in part be explained by overly aggressive dosing in the elderly.
The mechanism for increased sensitivity to warfarin with aging is not well-understood. Factors such as hypoalbuminemia (leading to a reduced volume of distribution), decreased dietary vitamin K intake (resulting in a decreased capacity to synthesize functional clotting factors), reduced absorption of vitamin K, and polypharmacy (producing drug-drug interactions that potentiate warfarin) may lead to increased warfarin sensitivity for an individual patient. The pharmacoldnetics of warfarin do not explain the lower dose requirements, because the distribution and elimination half-lives of warfarin change very little with advancing age. (34,35)
Pharmacodynamic changes with age have been studied much less. A negative correlation between age and hepatic drug-metabolizing enzymes has been observed in rat models in vitro, (36,37) and a study (38) of hepatic microsomal enzymes in humans showed a 30% decline in hepatic drug metabolism and cytochrome P450 content with age. Others have suggested an age-related decrease in the diffusion of oxygen within the hepatocyte that compromises the oxygen-dependent mixed-function oxidase enzymes. (39) Changes in hepatic glutathione levels and decreased activity of the nicotinamide adenine dinucleotide phosphate-dependent reductase of vitamin K are other touted hypotheses. (40)
The observation that women, independent of age, require less warfarin than men may be explained partly by differences in mean body size or hepatic fat content, or by intrinsic differences in warfarin metabolism. Reports (41) of sex-related differences in hepatic clearance by cytochrome P450 enzymes warrant further investigation. One set of experiments (42) using an animal model has suggested that the expression of at least some cytochrome P450 enzymes may be regulated by sex steroids.
Our study was based on two large patient populations. Therefore, we were unable to account for individual genetic variation (eg, polymorphism in P450 CYP2C9). However, differences in the CYP2C9 genotype would not be expected to confound our central findings of increased warfarin sensitivity with advancing age and gender. Furthermore, pharmacogenetic testing will not be widely available to assist physicians making time-sensitive treatment decisions in the office setting, and there is currently no evidence describing the specific influence of CYP2C9 genotype on warfarin dosing in individual patients.
The possible effect of weight on warfarin dose could not be completely accounted for in our data set. It is likely that female gender largely subsumes the effect of weight on dose requirement. In our analysis of a small subset of patients, the effect of weight was most evident in the uppermost deciles (ie, > 234 lbs). Overall, our data suggest that gender-related differences in dose are independent of weight.
The data used in our analysis were derived entirely from outpatients who were receiving long-term warfarin therapy. Although our study did not directly address the initiation doses of warfarin for the immediate treatment of an acute arterial or venous thrombosis, our results support a cautious approach to empiric dose selection, particularly in older women. Care must be taken in extrapolating the results from studies of younger cohorts with male predominance in whom initiation doses of 10 mg/d were shown to be safe. (43-47) The median doses listed in Table 2 may be a reasonable empiric choice for some elderly outpatients in whom warfarin therapy is being initiated. It must be remembered, however, that optimal initiation and maintenance doses of warfarin will likely be lower among hospitalized patients, because they are more likely to experience concomitant decreased oral intake, recent surgery, decompensated heart failure, liver impairment, polypharmacy, or other factors associated with reduced warfarin dose requirement. (10,48) Individuals who are sensitive to warfarin would be expected to manifest an early, exuberant anticoagulant response, usually after the second dose. Finally, for patients whose weight deviates significantly from the norm for their age and gender, body mass should also be considered in any empiric dosing decisions.
CONCLUSIONS
This study found that mean warfarin doses declined predictably with age and were lower in women than in men. The average maintenance dose for young men was 6.4 mg/d; for women > 80 years of age, the average maintenance dose was only 3.1 mg/d. These observations suggest that the current initiation and maintenance doses should be modified to reduce the risk of inadequate therapy in young patients, and excessive anticoagulation in elderly patients.
APPENDIX
The following practices and directors participated in the study, with the sites listed in decreasing order of the number of patients enrolled: Lutheran General Hospital, Niles, IL: W. Fried, M. Pubentz; Physicians, Inc., Lima, OH: D. Parker; Idaho Cardiology Associates, Boise, ID: F. Badke; North Clinic, Robbinsdale, MN: V. Krug; Rockwood Clinic P.S.-Main, Spokane, WA: J.S. Pennock; Wenatchee Valley Clinic, Wenatchee, WA: R. Kirby Primm, L. Vaughn; Framingham Heart Center, Framingham, MA: J. Dangel, S.R. Hewett; Clinic Pharmacy Consultants-Brainerd Medical Center, Brainerd, MN: B. Twamley, R. Sorenson; Woodland Healthcare, Woodland, CA: L. Smith, T. Fajerson; Cardiology, PC, Syracuse, NY: S. O'Donnell; Health Care American Corp, Bradenton, FL: C. Hoffman; DuPage Medical Group-Department of Cardiology, Winfield, IL: N. Kinsley; Camino Medical Group, Sunnyvale, CA: S. Edwards; Ohio Valley Heartcare, Evansville, IN: L. Janeira, J. Robb; Desert Medical Group/Oasis IPA, Palm Springs, CA: H.F. Bellaci, J. Bellaci; Anchor Health Center, Naples, FL: M. Means; Sutter Gould Medical Foundation, Modesto, CA: J.E. Baker; Hannibal Clinic Inc., Hannibal, MO: L. Chalton; Saratoga Cardiology, Saratoga Springs, NY: R. Sheldon, D. Kandath; Lima Memorial Hospital, Lima, OH: C.L. Thompson, J. Recker; Staten Island University Hospital, Staten Island, NY: M. Howard; Jacksonville Cardiovascular Clinic, Jacksonville, FL: R.A. Benson; River Valley Healthcare, Silvis, IL: K.Carroll; Family Physician Incorporated, N. Canton, OH: H. Marshall; Internal Medicine of Northern Michigan, Petoskey, MI: P.D. Blanchard; Redmond Internal Medicine, Redmond, OR: D. Palmer, C. Gangan; Grove Hill Medical Center, New Britain, CT: M.S. Werner; Olean Medical Group, Olean, NY: H.D. Storch, T.L. Buzzard; Internal Medicine Associates of Greenville, Greenville, SC: J.S. Moore; Magan Medical Clinic, Covina, CA: R. Sakamoto; Owatonna Clinic-Mayo Health System, Owatonna, MN: T. Price; Dearborn Cardiology, Dearborn, MI: S. Dabbous; Westchester Medical Group, White Plains, NY: B. Newman; Central Cardiology Medical Clinic, Bakersfield, CA: W. Nyitray; Salem Clinic, Salem, OR: M. Smith; East Carolina University, Greenville, NC: C. Estrada; Northwest Primary Care Group, Milwaukie, OR: D. McAnulty, P. Devisser; The William W Backus Hospital, Norwich, CT: S. Johnson; Jefferson city Medical Group, Jefferson City, MO: C. Balcer; Saint Louis University Department of Neurology, St. Louis, MO: S. Cruz-Flores, E. Holzemer; Wellspan Health-Yorktowne, York, PA: J.D. Horton; Mercy Medical Center, Canton, OH: M. Cudnik; Cardiovascular Group, Lawrenceville, GA: B. Craig-Allen; Asheville Cardiology Assoc, Asheville, NC: W. Wharton, A. Moser; Cardiac Consultants Chartered, Bethesda, MD: L. Chappell; Valley Care Health System, Pleasanton, CA: N. Huynh; Bloomington Hospital, Bloomington, IN: K. Kalotta; Samaritan Anticoagulation Service, Corvallis, OR: R. Stockberger; Covenant Clinic, Waterloo, IA: D. Kohls; Dartmouth-Hitchcock Nashua, Nashua, NH: L. Cook; Cardiology Consultants, PC, Hamden, CT: AM. Radoff; Seventh Avenue Family Health Center, Fort Lauderdale, FL: J. Berges; Diagnostic Cardiology, PA, Jacksonville, FL: P.D. Kuhlman; Norlanco Medical Associates, Elizabethtown, PA: J. Rittenhouse; University of Texas Medical Branch, Galveston, TX: H. yon Marensdorff; Bend Memorial Clinic, Bend, OR: M. Hegewald; Memorial Primary Care Center, Hollywood, FL: J. Beck; Batey Cardiovascular Center, Bradenton, FL: D. Calabrila, E.J.Sanchez; Western Montana Clinic, Missoula, MT: W.B. Bekemeyer, D. Ramsey; Winona Clinic, Winona, MN: L. Tschumper; Cardiac Consultants, Lancaster, PA: M. Lesko; Hattiesburg Clinic, Hattiesburg, MS: A.J. Jackson; Bryn Mawr Medical Specialist Association, Bryn Mawr, PA: H. Mayer; River Valley Healthcare, Moline, IL: B. Cady; Cardiovascular Group, Snellville, GA: L. Lesser; Medicor, Bridgewater, NJ: P. Saulino, C. Hartpence; Bond Clinic, PA, Winter Haven, FL: P. Lundsford. K. Bhatia; University of Cincinnati-Pharmacy Anti-coagulation Services, Cincinnati, OH: J. McQueen; Senior Healthcare Center, Gainesville, FL: M.L. Breeser; North Canton Medical Foundation, North Canton, OH: H.M. Schenker; Manor Family Health Center, Millersville, PA: J. Ichter; Cardiology Associates of Central Florida, Ocala, FL: L. McDaniel; Cardiovascular Associates Ltd, Chesapeake, Virgina: S.R. Jones; Woodburn Medical Clinic, Woodburn, OR: F. Golden; Rockwood Clinic North, Spokane, WA: C. Laudenbach, J.S. Pennock; Wachspress, Shatkin & Rainear, Vineland, NJ: L. Assink; Chambersburg Hospital, Chambersburg, PA: D. Grant; Wellspan Pharmacy-Dallastown, Dallastown, PA: T.G. Williams; Pulmonary & Critical Care Associates, Ypsilanti, MI: W.F. Patton; Island Cardiac Specialist, Mineola, NY: P. Ragno; Portland Cardiovascular Institute 2, Portland, OR: R. Chelfky; River Valley Healthcare ACS, Bettendorf, IA: W. Langley; Consultants in Cardiology, Farmington Hills, MI: G.M. McKendrick; Portland Cardiovascular Institute 1, Portland, OR: R. Chelfky; Cleveland Clinic Florida, Weston, FL: B. Fernandez; BiState Medical Consultants, St. Louis, MO: P.M. Stein, C.B. Lomnel; Medical Consultants, PC, Muncie, IN: J. Bow; Cardiovascular Associates of South Florida, Coral Gables, FL: J.S. Palmer; Parkway Cardiology Associates, Oak Ridge, TN: S. Cooke; Northwest Georgia Diagnostic Clinic, Gainesville, GA: J. Jackson; Cardiovascular Associates, Kingsport, TN: L.H. Cox; Heart Place, Dallas, TX: C.N. Bowers; Rockwood Clinic, Spokane, WA: C. Laudenbach; J.S. Pennock; Delaware Heart Group, Newark, DE: C. Bowens; and Abilene Diagnostic Clinic, Abilene, TX: P. Howard.
* From the Department of Medicine (Dr. Garcia), Division of General Internal Medicine, University of New Mexico School of Medicine, Albuquerque, NM; the Department of Medicine (Drs. Regan and Hughes), General Medicine Division, Massachusetts General Hospital, Harvard Medical School, Boston, MA; the Department of Medicine (Dr. Crowther), McMaster University, Hamilton, ON, Canada; and the Department of Medicine (Dr. Hylek), General Internal Medicine Research Unit, Boston University School of Medicine, Boston, MA.
This research was supported by a grant from Bristol-Myers Squibb, Princeton, NJ. Dr. Crowther holds a Canadian Institutes for Health Research Scholarship.
Manuscript received October 19, 2004; revision accepted December 3, 2004.
REFERENCES
(1) Feinberg WM, Blackshear JL, Laupacis A, et al. Prevalence, age distribution, and gender of patients with atrial fibrillation: analysis and implications. Arch Intern Med 1995; 155:469-473
(2) Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the Anticoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA 2001; 285:2370-2375
(3) Hylek EM, Go AS, Chang Y, et al. Effect of intensity of oral anticoagulation on stroke severity and mortality in atrial fibrillation. N Engl J Med 2003; 349:1019-1026
(4) Investigators AF. Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation: analysis of pooled data from five randomized controlled trials. Arch Intern Med 1994; 154:1449-1457
(5) Go AS, Hylek EM, Borowsky LH, et al. Warfarin use among ambulatory patients with nonvalvular atrial fibrillation: the anticoagulation and risk factors in atrial fibrillation (ATRIA) study. Ann Intern Med 1999; 131:927-934
(6) Brass LM, Krumholz HM, Scinto JM, et al. Warfarin use among patients with atrial fibrillation. Stroke 1997; 28:2382-2389
(7) Munschauer FE, Priore RL, Hens M, et al. Thromboembolism prophylaxis in chronic atrial fibrillation: practice patterns in community and tertiary-care hospitals. Stroke 1997; 28: 72-76
(8) Smith NL, Psaty BM, Furberg CD, et al. Temporal trends in the use of anticoagulants among older adults with atrial fibrillation. Arch Intern Med 1999; 159:1574-1578
(9) Kutner M, Nixon G, Silverstone F. Physicians' attitudes toward oral anticoagulants and antiplatelet agents for stroke prevention in elderly patients with atrial fibrillation. Arch Intern Med 1991; 151:1950-1953
(10) Hylek EM, Regan S, Go AS, et al. Clinical predictors of prolonged delay in return of the international normalized ratio to within the therapeutic range after excessive anticoagulation with warfarin. Ann Intern Med 2001; 135:393-400
(11) Fihn SD, Callahan CM, Martin DC, et al. The risk for and severity of bleeding complications in elderly patients treated with warfarin: the National Consortium of Anticoagulation Clinics. Ann Intern Med 1996; 124:970-979
(12) Gurwitz JH, Avorn J, Ross-Degnan D, et al. Aging and the anticoagulant response to warfarin therapy. Ann Intern Med 1992; 116:901-904
(13) Wynne H, Cope L, Kelly P, et al. The influence of age, liver size and enantiomer concentrations on warfarin requirements. Br J Clin Pharmacol 1995; 40:203-207
(14) Wynne HA, Kamali F, Edwards C, et al. Effect of ageing upon warfarin dose requirements: a longitudinal study. Age Ageing 1996; 25:429-431
(15) Redwood M, Taylor C, Bain BJ, et al. The association of age with dosage requirement for warfarin. Age Ageing 1991; 20:217-220
(16) James AH, Britt RP, Raskino CL, et al. Factors affecting the maintenance dose of warfarin. J Clin Pathol 1992; 45:704-706
(17) Landefeld CS, Goldman L. Major bleeding in outpatients treated with warfarin: incidence and prediction by factors known at the start of outpatient therapy. Am J Med 1989; 87:144-152
(18) van der Meer FJ, Rosendaal FR, Vandenbroucke JP, et al. Bleeding complications in oral anticoagulant therapy: an analysis of risk factors. Arch Intern Med 1993; 153:1557-1562
(19) Palareti G, Leali N, Coccheri S, et al. Bleeding complications of oral anticoagulant treatment: an inception-cohort, prospective collaborative study (ISCOAT); Italian Study on Complications of Oral Anticoagulant Therapy. Lancet 1996; 348: 423-428
(20) Hylek EM, Singer DE. Risk factors for intracranial hemorrhage in outpatients taking warfarin. Ann Intern Med 1994; 120:897-902
(21) Ansell J, Hirsh J, Poller L, et al. The pharmacology and management of the vitamin K antagonists: The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004; 126(suppl):204S-233S
(22) Gage BF, Eby C, Milligan PE, et al. Use of pharmacogenetics and clinical factors to predict the maintenance dose of warfarin. Thromb Haemost 2004; 91:87-94
(23) Fennerty A, Dolben J, Thomas P, et al. Flexible induction dose regimen for warfarin and prediction of maintenance dose. Br Med J (Clin Res Ed) 1984; 288:1268-1270
(24) Gedge J, Orme s, Hampton KK, et al. A comparison of a low-dose warfarin induction regimen with the modified Fennerty regimen in elderly inpatients. Age Ageing 2000; 29: 31-34
(25) Roberts GW, Druskeit T, Jorgensen LE, et al. Comparison of an age adjusted warfarin loading protocol with empirical dosing and Fennerty's protocol. Aust N Z J Med 1999; 29:731-736
(26) Fuster V, Ryden LE, Asinger RW, et al. ACC/AHA/ESC Guidelines for the Management of Patients With Atrial Fibrillation: Executive Summary A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines and Policy Conferences (Committee to Develop Guidelines for the Management of Patients With Atrial Fibrillation) Developed in Collaboration With the North American Society of Pacing and Electrophysiology. Circulation 2001; 104:2118-2150
(27) Fihn SD, McDonell M, Martin D, et al. Risk factors for complications of chronic anticoagulation: a multicenter study; Warfarin Optimized Outpatient Follow-up Study Group. Ann Intern Med 1993; 118:511-520
(28) Petitti DB, Strom BL, Melmon KL. Duration of warfarin anticoagulant therapy and the probabilities of recurrent thromboembolism and hemorrhage. Am J Med 1986; 81:255-259
(29) O'Reilly RA. The stereoselective interaction of warfarin and metronidazole in man. N Engl J Med 1976; 295:354-357
(30) O'Reilly RA. Stereoselective interaction of trimethoprim-sulfamethoxazole with the separated enantiomorphs of racemic warfarin in man. N Engl J Med 1980; 302:33-35
(31) Wells PS, Holbrook AM, Crowther NR, et al. Interactions of warfarin with drugs and food. Ann Intern Med 1994; 121: 676-683
(32) Cuzick J. A Wilcoxon-type test for trend. Stat Med 1985; 4:87-90
(33) Hirsh J, Poller L. Practical dosing considerations with warfarin and optimal therapeutic range. In: Poller L, Hirsh J, eds. Oral anticoagulants. London, UK: Arnold, 1996; 167-179
(34) Chan E, McLachlan AJ, Pegg M, et al. Disposition of warfarin enantiomers and metabolites in patients during multiple dosing with rac-warfarin. Br J Clin Pharmacol 1994; 37:563-569
(35) Routledge PA, Chapman PH, Davies DM, et al. Pharmacokinetics and pharmacodynamics of warfarin at steady state. Br J Clin Pharmacol 1979; 8:243-247
(36) Woodhouse KW, James OF. Hepatic drug metabolism and ageing. Br Med Bull 1990; 46:22-35
(37) Schmucker DL. Aging and the liver: an update. J Gerontol A Biol Sci Med Sci 1998; 53:B315-B320
(38) Sotaniemi EA, Arranto AJ, Pelkonen O, et al. Age and cytochrome P450-Linked drug metabolism in humans: an analysis of 226 subjects with equal histopathologic conditions. Clin Pharmacol Ther 1997; 61:331-339
(39) Le Couteur DG, McLean AJ. The aging liver: drug clearance and an oxygen diffusion barrier hypothesis. Clin Pharmacokinet 1998; 34:359-373
(40) Loguercio C, Taranto D, Vitale LM, et al. Effect of liver cirrhosis and age on the glutathione concentration in the plasma, erythrocytes, and gastric mucosa of man. Free Radic Biol Med 1996; 20:483-488
(41) Schwartz JB. The influence of sex on pharmacokinetics. Clin Pharmacokinet 2003; 42:107-121
(42) Niemela O, Parkkila S, Pasanen M, et al. Induction of cytochrome P450 enzymes and generation of protein-aldehyde adducts are associated with sex-dependent sensitivity to alcohol-induced liver disease in micropigs. Hepatology 1999; 30:1011-1017
(43) Kovacs MJ, Rodger M, Anderson DR, et al. Comparison of 10-mg and 5-mg warfarin initiation nomograms together with low-molecular-weight heparin for outpatient treatment of acute venous thromboembolism: a randomized, double-blind, controlled trial. Ann Intern Med 2003; 138:714-719
(44) Gage BF. Randomized trial of warfarin nomograms [letter]. Ann Intern Med 2004; 140:489
(45) Crowther MA, Harrison L, Hirsh J. Randomized trial of warfarin nomograms [letter]. Ann Intern Med 2004; 140:490
(46) Peterson GM, Jackson SL. Randomized trial of warfarin nomograms [letter]. Ann Intern Med 2004; 140:488
(47) White R, Dager W. Randomized trial of warfarin nomograms [letter]. Ann Intern Med 2004; 140:488-489
(48) Ageno W, Turpie AG, Steidl L, et al. Comparison of a daily fixed 2.5-mg warfarin dose with a 5-mg, international normalized ratio adjusted, warfarin dose initially following heart valve replacement. Am J Cardiol 2001; 88:40-44
David Garcia, MD; Susan Regan, PhD; Mark Crowther, MD, MSc; Robert A. Hughes, MD; and Elaine M. Hylek, MD, MPH ([dagger])
([dagger]) A list of practices and directors that participated in the study is located in the Appendix.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml).
Correspondence to: David A. Garcia, MD, Department of Internal Medicine, MSC10 5550, Albuquerque, NM 87131; e-mail: davgarcia@salud.unm.edu
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group