Some macrolides have been found to exert anti-inflammatory effects. Lung diseases such as asthma, panbronchiolitis, cystic fibrosis, and bronchiectasis are thought to respond to the immunomodulatory properties of macrolides. We report three cases of idiopathic bronchiolitls obliterans organizing pneumonia, now called cryptogenic organizing pneumonia, and three cases of radiation-related bronchiolitis obliterans organizing pneumonia that responded to macrolide therapy. An explanation of why macrolides may have anti-inflammatory effects in patients with these syndromes is discussed. These cases help to reinforce accumulating data that macrolides are beneficial as anti-inflammatory agents and organizing pneumonia may be another pulmonary disease that can benefit from such therapy.
Key Words: bronchiolitis obliterans organizing pneumonia; cryptogenic organizing pneumonia; macrolides; treatment
Abbreviations: BOOP = bronchiolitis obliterans organizing pneumonia; CF = cystic fibrosis; COP = cryptogenic organizing pneumonia; DPB = diffuse panbronchiolitis; IL = interleukin
**********
Bronchiolitis obliterans organizing pneumonia (BOOP) is both a pathologic entity and a clinical syndrome. (1,2) Pathologically, if there is no other predominant accompanying histology, it is now classified as organizing pneumonia to avoid confusion with other primary airway disorders. (1). Clinically, it can be idiopathic, also termed cryptogenic organizing pneumonia (COP), or it can accompany many other disorders including connective tissue diseases, drug- or radiation-induced injury, and a variety of other systemic illnesses. When it is seen in association with other diseases, it is still referred to as BOOP. Whether it is idiopathic or occurs with other disorders, corticosteroid therapy is the first line of treatment and usually is very effective. We report three cases of COP and three cases of radiation-related BOOP that improved with macrolide therapy. Some patients were started on macrolides for suspected bacterial infection and subsequently received a pathologic diagnosis of organizing pneumonia. Other patients either refused corticosteroid therapy or could not tolerate the side effects and were administered macrolides as alternative anti-inflammatory treatment. We theorize why this group of antibiotics may be therapeutic in patients with this syndrome.
CASE 1
A 72-year-old man with a history of prostate cancer was well until 3 weeks prior, when cough productive of green sputum developed accompanied by low-grade fever. A chest radiograph showed a right lower lobe infiltrate, and CT of the chest revealed multiple bilateral patchy infiltrates predominately in the lower lobes as well as subcentimeter pulmonary nodules (Fig 1, top). The latter were present for two years and were presumed metastatic from the prostate. Because the nodules were stable, he received no cancer treatment. Although the productive cough improved with 8 days of clarithromycin after it was discontinued, he continued to have low-grade fevers accompanied by night sweats, anorexia with a 5-lb weight loss, and mild dyspnea.
[FIGURE 1 OMITTED]
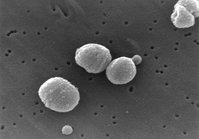
Physical examination was remarkable for oxygen saturation on room air at rest and at exercise of 97% and bilateral basilar rales. The only abnormal laboratory test result was a slightly elevated but stable prostate-specific antigen. After discontinuation of all antibiotics for at least 3 weeks, bronchoscopy with transbronchial biopsy of the right lower lobe was done and showed findings consistent with organizing pneumonia (Fig 2). All stains and culture findings were negative for organisms including bacteria, mycobacteria, and fungus. Since the patient had improved with clarithromycin, he was administered 250 mg bid for 2 months and 250 mg qd for another month. The symptoms completely resolved, and chest CT scan showed clearing of the infiltrates (Fig 1, bottom). Three years after presentation, the patient remained without recurrence, but he was subsequently treated with leuprolide acetate because the pulmonary nodules began to increase in size.
[FIGURE 2 OMITTED]
CASE 2
A 76-year-old man with colon cancer was referred to the pulmonary service for abnormal chest radiograph findings. The patient was status post right hemicolectomy and was receiving chemotherapy for a local recurrence that was complicated by profuse diarrhea and vomiting requiring hospitalization. Two weeks after hospital discharge, although the diarrhea and vomiting had subsided, cough, pleuritic pain, and dyspnea with exertion developed but no fever or chills. There was no history of aspiration with the vomiting. Chest radiography revealed a new patchy infiltrate in the left lower lobe and right lower lobe consolidation.
Physical examination showed oxygen saturation at rest and on room air of 97% and rhonchorous breath sounds at the right base. ACT scan of the chest showed multifocal areas of alveolar infiltrates with an area of consolidation at the right base. The patient was thought to have a community-acquired pneumonia, and he was placed on clarithromycin (500 mg po bid) for 10 days. He improved symptomatically, but a repeat chest radiograph revealed persistent pulmonary abnormalities. Sputum cultures collected before initiation of antibiotics did not reveal any pathologic organisms. Transbronchial biopsy showed chronic inflammation, interstitial fibrosis, and intraalveolar organizing fibromyxoid polyps that were compatible with organizing pneumonia. There was no evidence of any pathologic infectious agents or malignancy. After 4 weeks of clarithromycin treatment, he became asymptomatic and remained on the antibiotic for 3 months (dosage was decreased to 250 mg bid and then qd). His chest radiograph showed complete resolution, and he remained without recurrence 3 years after presentation.
CASE 3
A 65-year-old woman was well until 3 months prior, when she began to experience malaise with nausea, vomiting, and weight loss. She underwent a CT scan of the chest, abdomen, and pelvis that was remarkable for bilateral lower lobe consolidations with air bronchograms, as well as bilateral nodules in the upper lobes. She was placed on clarithromycin and was referred for further evaluation. At the initial visit, the patient had lost 20 lb despite resolution of the vomiting. She denied cough, pleuritic chest pain, shortness of breath, hemoptysis, or fevers but had persistent malaise.
Physical examination was normal. Oxygen saturation at rest and on room air was 98%. Laboratory data were remarkable for a sedimentation rate of 49 mm/h (normal, 0 to 20 mm/h) and normal pulmonary function tests. Prior to any antibiotic therapy, the patient underwent bronchoscopy with transbronchial biopsy that revealed benign lung tissue and no organisms. The patient completed a 3-week course of clarithromycin with clinical and radiographic improvement. Clarithromycin was discontinued; approximately 3 weeks later, malaise, low-grade fevers, and a dry cough developed. Repeat CT scan showed new consolidation of the right upper lobe and new nodular opacities bilaterally. The patient once again was placed on clarithromycin with improvement clinically and radiographically but relapsed after a 3-week course was discontinued.
Video-assisted thoracoscopic wedge biopsy of the right upper and lower lobes revealed findings consistent with organizing pneumonia. All smears and culture findings were unremarkable without antibiotics for at least 1 month. The patient was placed on oral steroids for 6 months and had complete resolution of symptoms and radiographic findings. She remains well 4 years after the diagnosis of BOOP.
CASES 4, 5, AND 6
These cases are thought to represent radiation-related BOOP. (3-5) These patients had tissue that either confirmed the diagnosis and/or ruled out other diagnoses such as infection or malignancy.
Case 4
A 56-year-old woman presented with a nonresolving right-sided infiltrate after radiation to right breast cancer. The patient had a diagnosis of organizing pneumonia on open-lung biopsy that initially improved with corticosteroid therapy. She had clinical relapse with cough and radiographic recurrence when the drug was discontinued. Because the patient had severe side effects from corticosteroids, she was successfully treated with clarithromycin (250 nag bid for 2 months and then decreased to 250 mg qd for 1 month). The antibiotic was discontinued after 3 months because of a skin rash, without clinical or radiographic relapse.
Case 5
A 62-year-old woman had a cough, low-grade fever, and bilateral patchy infiltrates with air bronchograms 8 months after receiving radiation to the cervical spine because of impending spinal cord compression due to metastasis from breast cancer. The patient also received paclitaxel. The physical examination was unremarkable, and the oxygen saturation at rest and on room air was 98% and with exercise was 96%. Although radiation-related BOOP was suspected, transthoracic needle biopsy was done to rule out metastatic lung disease and infection. The cell block was consistent with organizing pneumonia. All culture findings for bacteria, mycobacteria, and fungi were unremarkable. Paclitaxel-induced lung injury was also considered but thought to be unlikely due to the pathology findings. Hence, the drug was continued and the patient had a complete resolution of symptoms and radiographic findings after 7 months of corticosteroid therapy. However, after a very slow steroid taper, the patient relapsed with clinical symptoms and radiographic infiltrates similar to the original findings. Because avascular necrosis of tire right hip had developed with corticosteroid therapy, and because the symptoms were minimal, the patient was placed on clarithromycin, 250 mg bid. Four weeks after starting the antibiotic, the cough resolved and a repeat chest CT scan showed significant improvement in the infiltrates. She received clarithromycin for a total of 6 months.
Case 6
A 67-year-old man with a diagnosis of large cell lymphoma underwent radiation to the cervical and thoracic spine because of metastatic disease in that area. Approximately 2 weeks after the completion of the radiation, the patient had a very bad cough. At about the same time, an abscess on the right big toe developed and was treated with a 2-week course of levofloxacin. The cough did not respond to the drug, and it lasted for 6 weeks, after it was discontinued but then the cough resolved. Four months after completing radiation, the patient underwent an extent-of-disease evaluation to determine the need for further chemotherapy. His last chemotherapy was 5 months prior, with ifosfamide, earboplatin, and etoposide.
Chest CT scan revealed a new right lower lobe paramediastinal nodular infiltrate with multiple air bronchograms and a right middle lobe ground-glass opacity with irregular borders. The latter was outside the radiation portal. Physical examination at that time was unremarkable, including normal pulmonary function test results, except for a decrease in oxygen saturation from 97% at rest to 93% with exercise.
Radiation-related BOOP was considered likely, but because of the concern for recurrence of lymphoma the patient underwent needle biopsy of the right lower lobe nodular infiltrate. Histopathology showed inflammatory cells with no evidence of malignancy, and all smear and culture findings were negative for organisms. The patient had not received antibiotics for approximately 4 months.
Conventional radiation pneumonitis was considered unlikely because the patient never experienced dyspnea, some of the infiltrates were outside the radiation portal, and pulmonary function tests did not show a decrease in diffusing capacity. Recurrent lymphoma and infection were eliminated based on the pathologic findings and a clinical diagnosis of radiation-related BOOP was made.
The patient was treated with clarithromycin, and he had an excellent response with improvement in the right lower lobe and middle lobe infiltrates. However, due to a misunderstanding, the patient abruptly discontinued the clarithromycin with recurrence of the infiltrates, low-grade fever, and significant pleuritic chest pain. Because of the debilitating symptoms, he was started on a course of prednisone once again with clinical and radiographic improvement.
DISCUSSION
Organizing pneumonia is a common nonspecific histologic pattern seen in a wide variety of settings, including infection, granulomatous disease, vasculitis, hemorrhage, eosinophilic pneumonia, drug-induced lung injury, and many others. Pathologically, it is characterized by intraluminal polypoid plugs of granulation tissue extending continuously from the distal air spaces into alveolar ducts and alveoli. Other features include chronic inflammation of the walls of surrounding alveoli, increased foamy macrophages, and preserved lung architecture. When these features are the predominant pathologic findings and there is no other histology suggestive of another process, a pathologic diagnosis of organizing pneumonia is made. (1) Clinically cough is most common; dyspnea if present is mild. Radiographs typically show bibasilar, patchy 'alveolar infiltrates with a peripheral distribution. Although the classification of this syndrome remains controversial, the nomenclature used here is based on the American Thoracic Society/European Respiratory Society consensus statement on idiopathic interstitial pneumonia published in 2002. (1) The term COP is used when these clinical, radiographic, and pathologic findings are idiopathic, and BOOP is used when it is associated with other entities such as radiation or connective tissue diseases.
In these six patients, the diagnosis of organizing pneumonia is presented. Three cases clinically were idiopathic and considered COP, and three cases were thought to be related to radiation. In all cases, there was no evidence of an infectious or malignant etiology. Although in some, lung injury from chemotherapeutic agents was a possibility, the lack of dyspnea and diffuse interstitial infiltrates mitigated against the diagnosis of conventional chemotherapy -induced lung injury. When BOOP was associated with radiation, conventional radiation pneumonitis was unlikely because dyspnea, the hallmark of radiation pneumonitis, was absent and in all cases infiltrates occurred outside the irradiated portal, which is unusual for radiation pneumonitis.
When tissue documentation was obtained, organizing pneumonia was the predominate pathology. No pathologic organisms were isolated in any of the patients, and all patients responded to macrolide therapy at some point during the course of the illness. Although some patients with organizing pneumonia can be asymptomatic and/or improve without treatment, it would be quite unusual for all of our patients to improve spontaneously. In our experience and that of others, (3-6) the majority of patients with diffuse infiltrates due to organizing pneumonia will need treatment. Only 4% of patients with this syndrome will undergo spontaneous remission.
The use of macrolides to treat inflammatory diseases of the lungs is not a new concept. One of the first hints that macrolide antibiotics had anti-inflammatory activity associated with lung disease was in 1970, when Itkin et al (7) reported their experience in the treatment of asthmatic patients with erythromycin and troleandomycin. They found that adding a macrolide to the drag regimen of steroid-dependent asthmatics enabled steroid taper without deleterious effects. Studies (8-10) m from Japan have shown that short-term therapy with oral erythromycin or roxithromycin was associated with significant improvement of bronchial hyperactivity in asthmatics. More recently, long-term clarithromycin was found to have a steroid sparing effect in elderly patients with prednisone-dependent asthma. (11) Initially, macrolides were thought to inhibit theophylline clearance and/or increase the concentration of steroids to explain their beneficial action in asthmatic patients. However, in vivo and in vitro studies (8-27) support the fact that mechanisms other than drug interaction may explain the beneficial effects of macrolides in the treatment of asthma and other inflammatory conditions.
Much of the evidence that macrolides have immunomodulatory effects comes from Japan, where these antibiotics are effective in treating diffuse panbronchiolitis (DPB). (12-17) DPB is a disease of adults that is prevalent in Japan, Korea. and China and is characterized by infiltration of respiratory bronchioles with inflammatory cells. Ever since erythromycin has been used in the treatment of DPB, the 10-year survival rate has increased from 55 to 94%. (16) Although the pharmacologic activity of erythromycin is unknown in DPB, data support the hypothesis that its efficacy depends on mechanisms other than bactericidal activity. Polymorphonuclear cells are believed to play a crucial role in the deterioration of patients with DPB, and macrolides not only reduce the influx of polymorphonuclear cells into the lung but also decrease the production of cytokines involved in the inflammatory cascade, such as interleukin (IL)-8 and IL-1[beta]. (17)
Macrolides, as anti-inflammatory agents, may also have a role in the treatment of bronchiectasis. A double-blind, placebo-controlled trial (18) of low-dose, long-term erythromycin (500 mg bid for 8 weeks) showing improvement in patients with bronchiectasis has been published. In 11 patients who received erythromycin, FE[V.sub.1] and FVC increased while sputum volume over 24 h decreased significantly compared with those receiving placebo. Because erythromycin is unlikely to be bactericidal with these low doses, the authors (18) postulated that its inhibitory effect on stimulated neutrophils and on IL-8 production might be possible mechanisms to explain these findings.
Other in vivo and in vitro anti-inflammatory mechanisms for the macrolides include the following: their ability to inhibit neutrophil oxidation bursts, to decrease elastase activity, to suppress granulocyte macrophage-colony simulating factor, and to reduce or block production of both tumor necrosis factor-[alpha] and certain adhesion molecules such as soluble intercllular adhesion molecule-1. (19-26) The last two are necessary for neutrophil migration.
Clinical and pathologic similarities between DPB and cystic fibrosis (CF) have lead to the investigation of macrolides in the treatment of CF. Wolter et al (27) conducted a 3-month, prospective, placebo-controlled, double-blind trial of azithromycin, 250 mg/d, in 60 adults with CF. The treatment group had statistically significant improvements in FE[V.sub.1] percentage of predicted and FVC compared to the placebo-treated group. Furthermore, the azithromycin group required fewer days of therapy with IV antibiotics and had greater improvements in dyspnea, fatigue, emotional, and mastery domains on the chronic respiratory disease questionnaire compared with those in the placebo study arm.
In vitro studies show that short-term administration of macrolides result in enhancement of the immune response benefiting the treatment of infections, while long-term administration results in immunosuppression possibly helping patients with inflammatory conditions like DPB, CF, and organizing pneumonia. (28) This may explain why many of our patients (cases 1,2, 3, and 6) worsened or relapsed when macrolide therapy was discontinued after 10 to 21 days of initial improvement and why the CF patients of Wolter et al (27) improved with prolonged treatment.
The anti-inflammatory effects of macrolides appear to be dependent not only on duration of therapy but on their structure. The 14- and 15-membered ring structures, such as erythromycin, clarithromycin, and azithromycin, are believed to be the most effective anti-inflammatory macrolides. (19)
There are some BAL data (29) on patients with organizing pneumonia that show a mixed WBC pattern with increased lymphocytes (20 to 40%), neutrophils (up to 10%), and eosinophils (up to 5%). The lymphocyte pattern shows an increase in total lymphocyte count and a decrease in C[D.sub.4]/C[D.sub.8] ratio due to an increase in cytotoxic T-cells. (30) Aoki and Kao (26) demonstrated that erythromycin may exert anti-inflammatory effects on T-cells by inhibiting cytokine gene expression at the level of transcription activation. Keeping in mind the results of the BAL findings, the beneficial effects of macrolides in patients with COP or BOOP related to other disorders may not only be due to their immunosuppressive effect on polymorphonuclear cells and their products but also to their influence on T-cells.
Since BAL findings suggest that organizing pneumonia is an inflammatory disease within the distal airways and the alveoli, it is not surprising that macrolides as anti-inflammatory agents may be therapeutic. There is some scanty clinical evidence that suggests this is the case. Epler et al, (2) Arbetter et al, (4) and Ichikawa et al (31) reported small numbers of patients with this syndrome who improved with macrolide therapy, but details of these cases are not given. We also have several presumptive cases of radiation-related BOOP (not reported here) that have responded to clarithromycin. Because of the waxing-and-waning nature of symptoms, signs, and radiograph findings, the improvement with treatments with macrolides of their patients and some of our patients may have been coincidental. This seems unlikely in most of our cases, since there was a direct correlation between administration of the drug and improvement and, in some cases, relapse when it was stopped. As with other studies (3-5) involving treatment with low dose macrolides, we encountered no major complications. A rash developed in one patient (case 4), which subsided after clarithromycin was discontinued. (5)
Based on our experience, circumstances under which macrolide therapy for organizing pneumonia can be considered include the following: (1) in patients with minimal symptoms and/or minimal physiologic impairment; (2) as adjuvant therapy in patients receiving steroids; steroids can be tapered while initiating and continuing macrolides; and (3) in patients who cannot tolerate steroids. Just as with corticosteroids, macrolides should be continued for a prolonged period of time (3 to 6 months or longer) and tapered to prevent relapse.
Limitations
A limitation of this study is that all patients did not have a definitive diagnosis of organizing pneumonia. When feasible, tissue documentation is optimal, since other more serious disorders can present similar to COP/BOOP in the immunocompromised host.
CONCLUSION
There are accumulating data that reinforce the hypothesis of a direct immunosuppressive effect of maerolides on neutrophil and T-cell functions. Phagocytes and their cytokines, oxidants, and proteolyric enzymes are important effectors in some inflammatory diseases such as asthma, CF, bronchiectasis, and DPB. It is in these pulmonary disorders that macrolides have been shown to have some therapeutic efficacy, not as anti-infectious agents but as anti-inflammatory drugs. We believe our cases add support to the literature that macrolides may act as anti-inflammatory drugs in patients with organizing pneumonia whether it is idiopathic or related to another disorder such as radiation. While the use of macrolide therapy for treatment of COP/BOOP is feasible, the decision to use it should be made on a case-by-case basis. Before any definitive recommendations can be made, more information is needed, such as which patients are likely to respond to macrolide therapy, and the proper dosage and duration of macrolide therapy.
ACKNOWLEDGMENT: The authors thank Dr. Maureen Zakowski for interpretation of the pathology slides and Yvonne Herd for preparation of the manuscript.
REFERENCES
(1) Travis WD, King TE, Bateman ED, et al. ATS/ERS international multidisciplinary consensus classification of idiopathic interstitial pneumonia: general principles and recommendations. Am J Respir Crit Care Med 2002; 165:277-304
(2) Epler CR, Colby TV, McLoud TC, et al. Bronchiolitis obliterans organizing pneumonia. N Engl J Med 1985: 312: 152-158
(3) Bayle JY, Nesme P, Bejui-Thivolet F, et al. Migratory organizing pnemnonitis "primed" by radiation therapy. Eur Respir J 1995; 8:322-326
(4) Arbetter KR, Prakash UB, Tazelaar HD, et al. Radiation-induced pneumonitis in the non-irradiated lung. Mayo Clin Proc 1999; 74:27-36
(5) Stover DE, Milite F, Zakowski M. A newly recognized syndrome - radiation-related bronchiolitis obliterans organizing pnemnonia. Respiration 2001; 68:540-544
(6) Mohktari M, Bach PB, Tietjen PA, et al. Bronchiolitis obliterans organizing pneumonia in cancer: a case series. Respir Med 2092:96:280-286
(7) Itkin IH, Menzel ML. The use of macrolide antibiotic substances in the treatment of asthma. J Allergy 1970; 45:146-162
(8) Tamaoki J, Tagaya E, Sakai A, et al. Effects of macrolide antibiotic on neurally mediated contraction of human isolated bronchus. J Allergy Clin Immunol 1995; 95:853-859
(9) Shimizu T, Kato M, Mochizuki H, et al. Roxithromycin reduces the degree of bronchial hyperresponsiveness in children with asthma. Chest 1994:106:458-461
(10) Shoji T, Yoshida S, Sakamoto H, et al. Anti-inflammatory effects of roxithromycin in patients with aspirin-intolerant asthma. Clin Exp Allergy 1999; 29:950-956
(11) Carey KW, Rubinstein I, Gotfried MH, et al. Long-term clarithromycin decreases prednisone requirements in elderly patients with prednisone-dependent asthma. Chest 2000; 118:1826-1827
(12) Ichikawa Y, Ninomiya H, Koga H, et al. Erythromyein reduces neutrophils and neutrophil-derived elastolytic-like activity in the lower respiratory tract of bronchiolitis patients. Am Rev Respir Dis 1992; 146:196-203
(13) Nagai H, Shishido H, Yoneda R, et al. Long-term low-dose administration of erythromycin to patients with a diffuse panbronchiolitis. Respiration 1991; 58:145-149
(14) Oda H, Kadota J, Kohno S, et al. Erythromycin inhibits neutrophil chemotaxis in bronchoalveolar of diffuse panbronchiolitis. Chest 1994; 1065:1116-1123
(15) Kadota J, Sakito O, Kohno S, et al. A mechanism of erythromycin treatment in patients with diffuse panbronehiolitis. Am Rev Respir Dis 1993; 147:153-159
(16) Kudoh S, Azuma A, Yamamoto M, et al. Improvement of survival in patients with diffuse panbronchiolitis treated with low-dose erythromycin. Am J Respir Crit Care Med 1998; 157:1829-1832
(17) Sakito O, Kadota J, Kohno S, et al. Interleukin 113, tumor necrosis factor [alpha], and interleukin 8 in bronchoalveolar lavage fluid of patients with diffuse panbronehiolitis: a potential mechanism of macrolide therapy. Respiration 1996; 63:42-48
(18) Tsang KW, Ho PI, Chan KN, et al. A pilot study of low-dose erythromycin in bronchiectasis. Eur Respir J 1999; 13:361-364
(19) Wales D, Woodhead M. The anti-inflammatory effects of macrolides. Thorax 1999; 54(suppl 2):58S-62S
(20) Rubin BK, Henke MO. Immunomodulatory activity and effeciveness of macrolides in chronic airway disease. Chest 2004; 125(suppl 2):70S-788
(21) Labro MT, Benna J, Abdelghaffer H. Modulation of human polymorphonuclear neutrophil function by macrolides: preliminary data concerning dirithronaycin, J Antimicrob Chemother 1993; 31(suppl C):51S-64S
(22) Labro MT, Abdelghaffer H. Immunomodulation by macrolide antibiotics. J Chemother 2091; 13:3-8
(23) Ianaro A, Ialenti A, Maffia P, et al. Anti-inflammatory activity of macrolide antibiotics J Pharmacol Exp Ther 2090; 292: 156-163
(24) Yoshinmra T, Kurita C, Yamuzaki F, et al. Effects of roxithromycin on proliferation of peripheral blood mononuclear cells and production of lipopolysaeeharide-induced cytokines. Biol Pharm Bull 1995; 18:876-881
(25) Khair OA, Devalia JL, Abdelaziz MM, et al. Effect of erthromycin on Hacmophilus influenzae endotoxin-induced release of IL-6, IL-8 and sICAM-1 by cultured human bronchial epithelial cells. Eur Respir J 1995; 8:1451-1457
(26) Aoki Y, Kao PN. Erythromycin inhibits transcriptional activation of NF-KB, but not NFAT, through ealeinenrin-independent signaling in T-cells. Antimicrob Agents Chemother 1999; 43:2678-2684
(27) Wolter J, Seeney S, Bell S, et al. Effect of long term treatment with azithromyein on disease parameters in cystic fibrosis: a randomized trial. Thorax 2002; 57:212-216
(28) Levert H, Gressier B, Brunet C, et al. Time and concentration dependent influence of dirithromyein on neutrophil oxidative burst. J Antibiot (Tokyo) 1999; 52:127-133
(29) Nagai S, Aung H, Tanaka S, et al. Bronchoalveolar lavage cell findings in patients with BOOP and related diseases. Chest 1992; 102(suppl 1):32S-37S
(30) Mukae H, Kadota J, Kohno S, et al. Increase of activated T-cells in BAL fluid of Japanese patients with bronchiolitis obliterans organizing pneumonia and chronic eosinophilic pneumonia. Chest 1995; 108:123-128
(31) Ichikawa Y, Ninomiya H, Katsuki M, et al. Low dose erythromycin for treatment of bronchiolitis obliterans organizing pneumonia (BOOP). Kurume Med J 1993; 40:65-67
* From Memorial Sloan-Kettering Cancer Center, New York, NY.
Manuscript received September 8, 2003; revision accepted June 27, 2005.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml).
Correspondence to: Diane E. Stover, MD, FCCP, Memorial Sloan-Kettering Cancer Center, 1275 York Ave, New York, NY 10021; e-mail: stoverd@mskcc.org
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group