Periprosthetic bone loss after total joint arthroplasty is a major clinical problem resulting in aseptic loosening of the implant. Among many cell types, osteoblasts play a crucial role in the development of peri-implant osteolysis. In this study, we tested the effects of calcitriol (1[alpha],25-dihydroxy-vitamin-D^sub 3^) and the bisphosphonate pamidronate on titanium-particle-and TNF-[alpha]-induced release of interleukin-6 and suppression of osteoblast-specific gene expressions in bone-marrow-derived stromal cells with an osteoblastic phenotype. We monitored the expression of procollagen [alpha]1[1], osteocalcin, osteonectin and alkaline phosphatase mRNAs by Northern blots and real-time reverse transcription and polymerase chain reaction analyses. The release of various cytokines was also analysed by ELISA.
We found that calcitriol or pamidronate could only partially recover the altered functions of osteoblasts when added alone. Only a combination of these compounds restored all the tested functions of osteoblasts. The local delivery of these drugs may have therapeutic potential to prevent or to treat periprosthetic osteolysis and aseptic loosening of implants.
Particulate wear debris is generated continuously from implant materials used in total joint replacement. Phagocytosis of wear debris produces a permanent signal for many types of cells within the periprosthetic space. Phagocytosis-activated cells such as macrophages, fibroblasts, osteoblasts and osteoclasts then secrete various compounds, including tumournecrosis-factor-alpha (TNF-[alpha]) which has been considered to be one of the most dominant pro-inflammatory cytokines involved in the pathogenesis of periprosthetic osteolysis.1,2
Bone resorption occurs when the extracellular bone matrix is degraded by osteoclasts, or enzymes released by other activated cells, adjacent to the bone. In periprosthetic osteolysis a granulomatous soft tissue, composed predominantly of fibroblasts, macrophages and foreign-body giant cells, develops at the interface of the bone and the prosthesis. These cells are exposed to particles and release various soluble mediators3-6 and enzymes.7-10
The formation of bone is the primary function of osteoblasts. However, wear debris- or TNF-[alpha]-challenged primary human osteoblasts and human osteoblast-like cell lines produce prostaglandin-E^sub 2^ (PGE^sub 2^),11 interleukin (IL)-6,12-15 IL-8 and monocyte chemoattractant protein-1 (MCP-1).16 These mediators are either activators of osteoclasts (PGE^sub 2^ and IL-6)9 or chemotactic factors for leukocytes (IL-8 and MCP-1),16 thereby stimulating bone resorption directly and by way of an aseptic inflammatory cascade. In addition, the exposure of human osteoblasts to particulate wear debris or TNF-[alpha] results in a considerable suppression of the steady-state level of procollagen [alpha]1[1] mRNA followed by reduced synthesis of type-I collagen.12,13,17,18 Furthermore, it has recently been shown that different particles significantly influence the expressions of numerous genes in human osteoblasts.19 Taken together, particle-or cytokine-induced altered osteoblast function (reduced type-I collagen synthesis and increased production of pro-inflammatory mediators) may be a significant contributing factor to the development of periprosthetic osteolysis.
The reversal of altered osteoblast function in the periprosthetic milieu is an important target in the pharmacological management of periprosthetic osteolysis. Phagocytosis of wear debris activates nuclear transcription factor kappaB (NF-[kappa]B) by the activation of protein tyrosine kinases (PTKs) in human osteoblasts. The activated NF-[kappa]B can bind to the promoter region of the procollagen [alpha]1[I] gene and then inhibit the transcription of the [alpha]1 chain.12,18 The inhibition of either PTKs or NF-[kappa]B can completely reverse the negative effect of particles on the expression of procollagen [alpha]1[I].12,18 Furthermore, such diminished expression of procollagen [alpha]1 [I] mRNA and synthesis of type-I collagen can be normalised in vitro using insulin-like growth factor-I (IGF-I) or transforming growth factor beta-1 (TGF-[beta]1).13
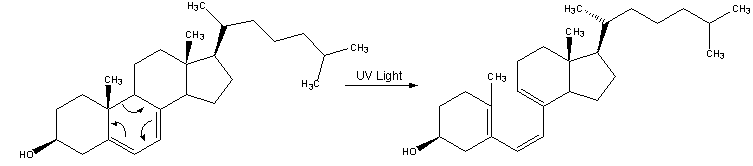
In order to explore the potential efficacy of systemically administered pharmacological agents in the reversal of altered osteoblast functions, we tested the effects of hormonally active calcitriol (1[alpha],2.5-dihydroxy-vitamin-D^sub 3^) and the bisphosphonate pamidronate on titanium-particle- and TNF-[alpha]-induced release of I1-6 and suppression of the synthesis of type-I collagen in the bone-marrow stromal cells with osteoblastic differentiation. We selected titanium particles as a prototype of particle wear debris and TNF-[alpha], a key regulator of the periprosthetic inflammatory cascade, to elucidate the osteohlast-specific responses to these two compounds in the presence or absence of either calcitriol or pamidronate. We monitored the expression of procollagen [alpha]1[I], osteocalcin, osteonectin and alkaline phosphatase mRNAs and the release of various cytokines in these cultures.
Materials and Methods
Particles. The particles used in these studies have been described previously.3,7,13,17 Particles of commercially pure titanium (cp-titanium) with a nominal diameter of 1 to 3 µm were purchased from Johnson Matthey (Danvers, Massachusetts) and size separated by filtration. At least 90% of the particles were smaller than 3 µm in diameter. Polystyrene-based fluorescent Fluoresbrite (0.926 ± 0.027 µm) particles were purchased from Polyscience (Warrington, Pennsylvania). Based on the size distribution, a 0.1% volume/volume (v/v) particle suspension of titanium and Huoresbrite contained approximately 2.2 to 6.7 x 10^sup 8^ particles/ml. The particles were sterilised by irradiation with 2.2 megarads (22 000 gray) from a ^sup 137^Cs source (model 143; JL Sheppherd Irradiator, San Fernando, California) and stored in sterile phosphate-buffered saline (PBS, pH 7.2). Sterile supernatants with or without particles and the conditioned media of cell cultures were endotoxin-free when analysed using the Limulllus assay (E-Toxate; Sigma Chemical Co, St Louis, Missouri).
Cells and cell cultures. Bone-marrow stromal cells with osteoblastic differentiation, henceforth called primary osteoblasts, were isolated from bone-marrow samples obtained from either the iliac crest or vertebral bodies of patients undergoing spinal fusion (Table I). The collection of bone marrow was approved by the Institutional Review Board and written consent was obtained from each patient. The culture conditions, isolation and characterisation of the cells were as described earlier.12,20 Briefly, buffy coat-separated nucleated bone-marrow cells (2 x 10^sup 7^/VT75 tissue-culture flasks; Corning Inc, Corning, New York) were cultured in alpha-minimal essential medium (Gibco; Invitrogen-Gibco Cell Culture Products, Carlsbad, California) containing 10% fetal bovine serum (FBS), 10 nM dexamethasone, 50 µg/ml of ascorbic acid, 100 U/ml of penicillin, 100 µg/ml of streptomycin, 0.25 µg/ml of amphotericin B and 50 µg/ml of gentamicin, all purchased from The Sigma Chemical Company. The first medium change was performed on day 7, also containing 5 mM beta-glycerophosphate (Sigma). Dense colonies of primary cultures were trypsinised, 1 x 10^sup 5^ cells plated in 10 cm size Petridishes (Corning), and cultured to obtain a confluent monolayer culture. All experiments with bone-marrow-derived osteoblasts were carried out using first-passage cultures. At the time of the first passage, aliquots of cells were also seeded in 12-, 24- and 96-well plates (Corning) for measuring the activity of alkaline phosphatase and cell proliferation and for carrying out tests of viability.
Assays for alkaline phosphatase. Confluent cultures of osteoblasts were stained in situ in 12-well plates for positivity of alkaline phosphatase using Napthol-AX and either Fast-Blue BB or Fast-Red Violet LB (both from Sigma) reagents according to the manufacturer's instructions. Cells were washed with sterile PBS and then incubated with 1 mM Naphthol-AX phosphate and 2 mM Fast-Blue BB or Fast-Red Violet LB in 0.1 M Tris-hydrochloric acid buffer (pH 9.1). After incubation for 30 minutes at 37°C in the dark, the cultures were washed with PBS and the number of alkaline-phosphatase-positive cells were counted under transmission light microscopy (Nikon Diaphot Invert; Fryer, Huntley, Illinois).
In order to analyse further the ratio of alkaline-phosphatase-positive cells, fluorogenic Fast-Red Violet LB21 and ELF-97(22) (Molecular Probes Inc, Eugene, Oregon) were applied according to published protocols since these reagents have a high specificity for alkaline phosphatase. The stained cells were then analysed by fluorescent microscopy (Nikon) and fluorescence-activated cellsorter (FACS) analysis (FACScan; BD PharMingen, San Diego, California) using Cell Quest software (BD PharMingen). The FACS method provides an accurate and highly reproducible assay to determine the fraction of alkaline-phosphatase-positive cells in individual cultures (10 000 cells were analysed in each measurement).
Treatment of cells. The confluent cultures of cells were subjected to serum starvation (0.3% FBS) for 24 hours before treatment. The culture media were then replaced with fresh medium containing 0.3% FBS and various compounds. Proliferation and viability assays, FACS analysis and total RNA extractions were carried out on the cultured cells. The tissue-culture media were collected at various time points, centrifuged and stored at -80°C. All analyses were performed to achieve at least five complete sets of experiments from five different individuals. Critical parts of the experiment, whenever additional cells/cultures of the same individual and/or from pooled samples were available, were repeated to confirm the results further and to exclude individual differences or possible technical errors using one (single) cell culture per assay. The results of repeats from the same individual were incorporated in statistical analyses, but those obtained from pooled cell cultures were not.
The following compounds were used either alone or in combination with particles. Calcitriol (Sigma) was used in concentrations ranging from 0.01 µM to 1 µM. Pamidronate (Bedford Laboratories, Bedford, Ohio) was used in concentrations ranging from 0.1 µg/ml to 100 µg/ml. TNF-[alpha] (R&D Systems Inc, Minneapolis, Minnesota) was used in concentrations ranging from 1 ng/ml to 50 ng/ml. Titanium particles were applied in concentrations ranging from 0.0125% to 0.2% v/v. In experiments in which pamidronate and/or calcitriol were combined with either titanium particles, TNF-[alpha] or both, pretreatment for three hours with calcitriol and/or pamidronate was utilised and then either titanium particles, TNF-[alpha] or both were added subsequently to the cultures. Various concentrations listed above were tested in preliminary experiments using primary osteoblast cell cultures.23 Only the most effective concentrations within the viable range were used.
Viability tests and ^sup 3^H-thymidine incorporation. The Trypan Blue exclusion test was used in situ in 24 well plates to determine cell viability as described previously.12,13,17 Tests of viability were performed in duplicate and at least 200 cells were counted. The proliferation of cells was measured by incorporation of ^sup 3^H-thymidine (Amersham International, Arlington Heights, Illinois) into DNA in a 96-well microplate system. Trypsinised cells were harvested (Tomtec Inc, Orange, Conneticut) at different time points after incubation in ^sup 3^H-thymidine (1 µC of ^sup 3^H-thymidine per well).
Measurement of cytokines and osteoblast-specific proteins in culture media. The concentrations of cytokine in the supernatants of osteoblast cultures were measured by sandwich enzyme-linked immunosorbent assays (ELISA) in 96-well microtitration plates following the manufacturer's instructions. High-sensitivity assay kits for TNH-[alpha] (assay range from 0.5 to 32 pg/ml), IL-1[beta], IL-6 (sensitivity range for both from 0.12 to 8.0 pg/ml) and TGF-[beta]1 (range from 31 to 2000 pg/ml) were purchased from R&D Systems. Secreted osteocalcin was measured by NovoCalcin and type-I collagen by Procollagen-C ELISAs purchased from Metra Biosystems (Mountain View, California).
RNA extraction and Northern blot hybridisation. Total RNA was isolated from confluent cultures as previously described.7,17 Approximately 10 µg of total RNA were denatured in 50% formamide, 17.5% formaldehyde and 20 mM 3-(N-morpholino) propane-sulphonic acid at pH 7.0, 5 mM sodium acetate and 1 mM EDTA at pH 8.0, electrophoresed in 1% agarose gel and transferred to Gene-Screen Plus membranes (New England Nuclear, Boston, Massachusetts). The membranes were stained with ethidium bromide and the level of 28S and 18S ribosomal RNA quantified by an Imagel Software package (Meta Imaging Series, Universal Imaging Corp, West Chester, Pennsylvania). The blots were hybridised with ^sup 32^P-dCTP-labelled specific cDNA probes at a concentration of 3 × 10^sup 6^ cpm/ml (specific activities; 2 to 6 7times; 10^sup 8^ cpm/µg cDNA).7 Human-specific cDNA probes (plasmids) were purchased from the American Type Culture Collection (ATCC, Manassas, Virginia). The following recombinant plasmid DNAs were used as probes: a 1.8 kilobase (Kb) long cDNA probe for procollagen [alpha]1[I] (Hf677; ATCC #61322), a 2.0 Kb probe for osteocalcin (ATCC #86269), a 1.8 Kb for osteonectin (ATCC #78193), a 1.5 Kb probe for alkaline phosphatase (ATCC #59633) and a 0.7 Kb probe for glyceraldehyde-3-phosphate dehydrogenase (GAPDH, ATCC #57234). After hybridisation, the blots were washed and exposed to Kodak XAR-5 film (Kodak, Rochester, New York) at -70°C or the original Northern blot was analysed by STORM Phosphorlmager using Image-Quaint image-analysis software (Molecular Dynamics, Sunnyvale, California). For the purpose of comparison of our previous and current studies, we normalised all Northern hybridisation results to the levels of 28S and I8S ribosomal RNA.12,13,17,18
Reverse transcription (RT) of RNA and quantitative real-time polymerase chain reaction (PCR). The first-strand cDNA was synthesised from 2 µg of total RNA priming by the oligo(dT) using Superscript RT kit (Invitrogen, Carlsbad, California). The target cDNAs were amplified by quantitative real-time PCR using Cepheid Smart Cycler (Cepheid, Sunnyville, California). The primer pairs and their annealing temperatures used in real-time PCR analyses are given in Table II. The DNA-intcrcalating SYBR-Green I (Molecular Probes Inc, Eugene, Oregon) fluorescent dye was used to detect the PCR products. To verify that equal amounts of RNA had been added in each PCR reaction, real-time PCR amplification of the GAPDH housekeeping gene was performed in each sample. The relative differences between the samples at different time points were determined using the delta-delta cycle threshold ([Delta][Delta]CT) method as described in the Applied Biosystems' protocol for real-time PCR (Applied Riosystems, Foster City, California). First, a [Delta]CT value was calculated for each sample by subtracting the cycle threshold (CT) value of GAPDH from the CT value of the corresponding sample. The [Delta][Delta]CT value was then calculated by subtracting the [Delta]CT of the control (untreated) from the [Delta]CT of a treated sample. In order to determine the differential expressions of various samples compared with untreated controls, the [Delta][Delta]CT values were converted to fold differences (compared with the control).
Statistical analysis. Descriptive statistics were used to determine group means and standard deviations. The paired Student's t-test was performed between groups of interest. Linear regression was used to describe the relationship between the ratio of alkaline-phosphatase-positive cells and age. Analysis of covariance was used to determine whether the relationship between each outcome varied by gender while controlling for age. The level of significance was set at p
Results
Sample characterisation and yield of alkaline-phosphatase-positive primary osteoblasts. Over a period of three years, 47 bone-marrow samples were cultured and tested for the differentiation of osteoblasts (Table I). As shown in Figure 1, the ratio of alkaline-phosphatase-positive cells significantly declined with age in both women and men (p
Bone-marrow-derived alkaline-phosphatase-positive human osteoblasts phagocytose particles. Bone-marrow-derived alkaline-phosphatase-positive primary human osteoblasts phagocytosed particles in a time-dependent fashion. Both metal (not shown) and polymeric (Fluoresbrite, Figs 2b and 2e) particles were engulfed by primary human osteoblasts analysed either by FACS (Fig. 2e) or fluorescent (Fig. 2b) and transmission light microscopy (not shown). These results were comparable to those which we reported earlier for human osteoblast-like MG-63 cells.13
Effect of participate wear debris, TNF-[alpha], pamidronate and calcitriol on the viability and proliferation of primary human osteoblasts. Although high concentrations of titanium particles (>0.5% v/v) may induce apoptotic cell death,19,25 we did not detect reduced cell viability between the range of 0.0125% and 0.2% v/v in primary osteoblast cultures. In contrast to cell viability, the uptake of ^sup 3^H-thymidine, used as a marker for cell proliferation, dramatically declined in the presence of particles in both a time- and dose-dependent manner (Fig. 3).
Higher concentrations (50 ng/ml) of TNF-[alpha] significantly reduced cell viability, especially in long-term (>72 hours) experiments in primary osteoblast cultures. As shown in Figure 3, even a non-toxic concentration of 20 ng/ml of TNF-[alpha] (>95% viability) still decreased the proliferation of primary human osteoblasts.
Pamidronate had no effect on the viability of primary osteoblasts in a range of concentration between 0.1 and 100 µg/ml whereas calcitriol dramatically reduced the viability at or above a concentration of 1 µg. Pamidronate increased and calcitriol (in a non-toxic range of concentration) inhibited the proliferation of osteoblasts in a time- and close-dependent manner (Fig. 3).
Expression of osteoblast-specific genes as a response to titanium particle or TNF-[alpha] stimulation. Previously we reported that there was a consistent suppression of the level of procollagen al[I] mRNA in primary human osteoblasts12 and in various human osteoblast-like cells12,13,17,18 after exposure for 48 hours to titanium and other types of phagocytosable particles. In order to elucidate further the effect of particles on human osteoblasts, bone-marrow-derived human osteoblasts were exposed to titanium particles for 24 and 48 hours and then osteoblast-specific gene expression and release of protein were analysed. Titanium particles suppressed the steady-state levels of procollagen [alpha]1 [I] and osteonectin mRNA (Fig. 4) in human bone-marrowderived primary human osteoblasts, but did not show a significant effect on mRNA expression of alkaline phosphatase (Fig. 4) and osteocalcin (not shown) genes. These results were comparable with those found earlier in titanium-stimulated MG-63, HOS or SaOS-2 osteoblast-like cell lines,12,13' except that expression of osteonectin-specific mRNA was never suppressed in osteosarcoma-derived osteoblast-like cells.13
In contrast to the treatment of titanium particles, TNF-[alpha] inhibited the expression of procollagen [alpha]1[I], osteonectin and alkaline phosphatase genes, while the mRNA expression of ostecalcin did not change (Fig. 5).
Recovery of suppressed procollagen [alpha]1[I], alkaline phosphatase and osteonectin gene expressions by pamidronate and calcitriol. Preliminary results have shown that calcitriol can reverse the titanium-induced down-regulation of procollagen [alpha]l[I] gene expression in primary human osteoblasts.23 In addition to calcitriol, we also tested the effect of the pamidronate on the expression of osteoblast-specific genes in the presence or absence of either titanium particles or TNF-[alpha] in cultures of primary human osteoblasts. Both compounds showed distinctive effects on osteoblastspecific gene expression. Calcitriol increased the steady-state levels of mRNA for procollagen [alpha]1 [I] (Figs 4 and 5a), alkaline phosphatase (Figs 4 and 5c) and osteocalcm (Fig 5d), while the expression of osteonectin remained unchanged (Figs 4 and 5b). Pamidronate had no effect on procollagen [alpha]1[I|, osteonectin (Figs 4, 5a and 5b) and osteocalcin (Fig. 5d) gene expression, but significantly suppressed the alkaline-phosphatase mRNA level (Figs 4 and 5c).
The most important observation of these experiments was that particle- (Fig. 4) or TNF-[alpha]- (Fig. 5) induced suppression of osteoblast specific genes was blocked when primary osteoblasts were exposed to either calcitriol or pamidronate. Specifically, titanium-particle-induced inhibition of procollagen [alpha]1[I] gene expression was reversed completely by calcitriol and partially by pamidronate (Fig. 4). The latter also reversed the particle- (Fig. 4) and TNF-[alpha]-induced osteonectin gene suppression (Fig. 5b). TNF-[alpha]-mediated inhibition of either procollagen [alpha]1[I] or expression of alkaline phosphatase were completely abolished by calcitriol, while pamidronate had no effect (Figs. 5a and 5c). TNF-[alpha], however, specifically reduced the effect of calcitriol on the level of osteocalcin mRNA (Fig. 5d).
Since neither pamidronate nor calcitriol alone was able to restore completely all suppressed osteoblast-specific gene expression measured in our study, the combination of the two compounds was applied. Osreoblasts were pretreated simultaneously with pamidronate and calcitriol for three hours, and co-challenged with titanium particles and/or TNF-[alpha] for 24 and 48 hours. These experiments showed that the combination of pamidronate and calcitriol reversed the titanium- and TNF-[alpha]-induced suppression of all of the osteoblast-specific genes tested (Fig. 6).
The release of type-I collagen in osteoblast cultures correlated well with the mRNA levels in the corresponding cultures. As type-I collagen forms 90% of the organic extracellular bone matrix, we tested not only the level of mRNA for procollagen [alpha]1[I] but also the release of type-I collagen into the conditioned media of human osteoblasts in the presence or absence of titanium particles, TNF-[alpha], pamidronate and calcitriol. Similar to mRNA expression (Figs 4 to 6), titanium particles (p = 0.03) and TNF-[alpha] significantly (p = 0.007) reduced the amount of secreted type-I collagen (Fig 7a). Calcitriol significantly (p = 0.006) increased the production of type-I collagen and diminished the suppressive effects of both titanium particles and TNF-[alpha] on the synthesis of type-I collagen (Fig. 7a). By contrast, pamidronate had no effect on the release of type-I collagen when it was added alone. However, pamidronate prevented the suppression of the production of type-I collagen in the presence of the titanium particles (Fig 7a). Taken together, these two compounds were able to reverse the altered synthesis of type-I collagen suppressed by either titanium particles or TNF-[alpha] (Fig. 7a), thus improving the potential of the synthesis of bone matrix.
Titanium particle- or TNF-[alpha]-induced IL-6 release is reduced by either pamidronate or calcitriol. To characterise further the effect calcitriol and pamidronate on primary osteoblasts treated with titanium particles and TNF-[alpha], the levels of various cytokines were measured in the conditioned media of cultures of primary osteoblasts. Among the cytokines and growth factors tested (TNF-[alpha], IL-1[beta], IL-6 and TGF-[beta]1), only the basal secretion of IL-6 became significantly (p
Both calcitriol and pamidronate substantially suppressed the basal secretion of IL-6 (Fig. 7b). Titanium- and TNF-[alpha]-induced up-regulation of the release of IL-6 was inhibited by pamidronate, while calcitriol could only partially reduce the effect of titanium or TNF-[alpha] on the release of IL-6 (Fig. 7b). These findings are particularly interesting since IL-6 has been shown to induce the differentiation and activation of osteoblasts.9 Therefore, the inhibition of wear debris- or TNF-[alpha]-induced release of IL-6 by either pamidronate or calcitriol may have a beneficial effect on the normalisation of bone turnover by reducing the osteoclast-activating effects of osteoblasts.
Discussion
Aseptic loosening of an implant associated with focal periprosthetic osteolysis is one of the most common long-term complications of total joint replacement. Although the pathogenesis of this process has not been completely elucidated, the interaction between particulate wear debris and the cells of the periprosthetic milieu has been shown to be the most critical element. As our understanding of the complexity of the cellular response to wear debris is increasing, the possibility of developing pharmacological approaches to prevent or reverse the altered cellular functions in the periprosthetic space is becoming more realistic. The analysis of basic signal transduction pathways induced by wear-debris phagocytosis in various cell types and the identification of different molecules and mechanisms involved in wear-debris-induced bone resorption1,2,12,18,26-36 provide target molecules for the pharmacological prevention of periprosthetic bone loss. A few promising pharmacological compounds have already been tested in various animal models of wear-debris-induced osteolysis.36-41 However, most of these studies focus on the catabolic (bone resorption) aspect of bone turnover and ignore the anabolic (bone formation) processes.
Osteoblasts undergo crucial changes in the presence of wear debris and TNF-[alpha]. We have shown that titanium particles and TNF-[alpha] suppress the bone-forming capacity of human osteoblasts by decreasing the synthesis of hone matrix molecules while simultaneously increasing the osteoclast-activating potential of these cells by up-regulating the secretion of IL-6. This can clearly exacerbate osteoclastic bone resorption.
Bisphosphonates, including pamidronate, and vitamin-D metabolites have been widely used in various metabolic bone diseases such as Paget's disease, osteoporosis, osteolytic metastases and multiple myeloma.42,43 In our study, we have shown that pamidronate and calcitriol can normalise titanium particle- and TNF-[alpha]-induced altered osteoblast function at least in in vitro conditions. Most of the beneficial effects of bisphosphonates are due to their ability to inhibit the bone-resorptive properties of osteoclasts. The mechanisms responsible for this action have been described although some details still remain unclear.42 Recently, a small number of studies have indicated that bisphosphonates directly affect various functions of osteoblasts which may also contribute to the positive impact of bisphosphonates on bone turnover.44-46 For example, it has been shown that they influence the proliferation of osteoblasts. This effect, however, seems to be cell type-dependent since the proliferation of calvaria-derived primary mouse osteoblasts was increased,45 whereas the proliferation of an immortalised osteoblast-like cell type was decreased.44 Our results support the first observation above45 since we have also detected increased proliferation of primary human osteoblasts in the presence of pamidronate (Fig. 3).
Pamidronate has also been shown to be able to influence the bone-forming properties of osteoblasts by regulating the synthesis of various osteoblast-specific proteins such as type-I collagen and alkaline phosphatase.44,46 In our study, the positive effects of pamidronate on the expression of osteoblast-specific genes was particularly evident in that the suppressive effect of titanium particles and/or TNF-[alpha] on the expression of procollagen [alpha]1[I] and osteonectin genes in primary human osteoblasts was reversed (Figs 4 and 5).
Bisphosphonates are also capable of decreasing the development and activity of osteoclasts indirectly through their effects on osteoblasts. Recently, new members of the TNF family such as the receptor activator of nuclear factor-kappaB, RANK ligand (RANKL) and the decoy receptor osteoprotegerin (OPG) for RANKL have been described and have been found to be essential regulators of bone remodelling, and the differentiation and activation of osteoclasts.4 Under physiological conditions, osteoblasts express RANKL which interacts with osteoclast-expressed RANK, thus activating the osteoclast. In the presence of pamidronate, osteoblasts produce a significant amount of OPG which neutralises RANKL thus inhibiting the function of osteoclasts.46 This finding may be particularly important since it has been shown that RANKL/RANK is associated with periprosthetic osteolysis29 and that the blockade of the RANKL/RANK system by OPG gene therapy successfully diminishes wear-debris-induced osteolysis in an animal model.41
Bisphosphonates may also directly inhibit the function of osteoclasts via the osteoblast through an additional mechanism. Osteoblasts secrete significant amounts of IL-6 when exposed to titanium particles or TNF-[alpha] (Fig. 7b).12,13 The secreted IL-6 can act directly on osteoclasts in a paracrine manner.48 More importantly, the secreted IL-6, complexed with functional soluble IL-6 receptor, can mediate the autocrine effects of IL-6 on osteoblasts through the gp130-JAK (Janus kinase)-STAT (signal transducer and activator of transcription) pathway,49 a signalling mechanism by which IL-6 may up-regulate the expression of RANKL.50 By contrast, pamidronate completely diminished titanium- and TNF-[alpha]-induced secretion of IL-6 (Fig. 7b) thus inhibiting IL-6-dependent activation of osteoclasts. Based on the complexity of the effect of pamidronate on the function of osteoblasts (discussed above), it can be hypothesised that osteoblastic cells may be required for the complete antiresorptive effect of bisphosphonates.
Pamidronate exerts its positive effects on hone turnover by directly inhibiting the development and activity of osteoclasts and also by normalising altered osteoblast functions. It has been reported that different bisphosphonates inhibited periprosthetic osteolysis in various animal models.51-53 Furthermore, the bisphosphonates, pamidronate and aledronate have already been used on patients with implants in order to maintain normal periprosthetic bone stock.54,55 However, none of these studies has investigated the cellular mechanisms of the action of hisphosphonates on human osteoblasts which may at least in part, mediate the beneficial effects of hisphosphonates.
In our study, calcitriol, which is the most potent vitamin-D metabolite, effectively reversed several altered osteoblast functions induced by titanium particles or TNF-[alpha]. The effects of calcitriol on osteoblasts have been well characterised.56 It exerts its effect through its nuclear vitamin-D receptor (VDR) and plasma-membrane receptors distinguishing a genomic and a non-genomic rapid mechanism, respectively. Various cell types, including osteoblasts, have been shown to respond very rapidly, from seconds to minutes, to calcitriol challenge, a process which increases the intracellular calcium level and activates various intracellular signalling mechanisms including protein kinase A (PKA) and protein kinase C (PKC) pathways.43,57 The genomic VDR is present in numerous types of cells, thus, calcitriol can activate a variety of target organs and cells.43 Furthermore, it has been shown that the non-genomic effects may influence the genomic actions by activating protein kinases which, in turn, phosphorylate the VDR complex changing the transcriptional activity of VDR on numerous genes.43,57
The overall effect, either genomic, non-genomic or a combination, largely depends on the vitamin-D derivative applied.43 In our study, calcitriol increased the transcription and synthesis of the bone matrix molecules tested, except for osteonectin. Importantly, calcitriol reversed the suppressive effects of titanium particles and TNF-[alpha] on procollagen [alpha]1[I] and alkaline phosphatase genes, theoretically restoring the bone-forming capability of osteoblasts (Figs 4 and 5). Moreover, calcitriol was able to reduce the titanium particle- and TNF-[alpha]-induced secretion of IL-6 which, in turn, can reduce the osteoclast-activating function of osteoblasts as described above for bisphosphonates (Fig. 7b).
While these direct positive effects of calcitriol on osteoblasts are promising, the role of vitamin-D metabolites in the treatment of diseases affecting hone turnover is controversial.43 Calcitriol is a potent stimulator of bone resorption by increasing the differentiation and activation of osteoclasts in lower doses. On the other hand, high doses of calcitriol increase the activity of osteoblasts thus maintaining positive remodelling balance. The use of a high dose for long-term treatment, however, may result in hypercalcemia and hypercalcuria because of excessive intestinal calcium absorption.43 Nonetheless, it has been shown that the combination of calcitriol and bisphosphonates reduces the amount of calcitriol needed to achieve positive effects on bone metabolism,58 thus reducing possible side-effects.
In conclusion, we have shown that wear debris (titanium particles) and TNF-[alpha], two key factors in the development of periprosthetic osteolysis, significantly alter the normal function of osteoblasts. Neither pamidronate nor calcitriol alone was able to reverse completely all of the altered osteoblast functions which were induced by titanium particles and TNF-[alpha]. Pamidronate, for example, was more effective in reversing the expression of the osteonectin gene and reducing the secretion of IL-6 whereas calcitriol was a more potent inducer of procollagen [alpha]1[I], alkaline phosphatase and osteocalcin gene expressions.
Importantly, the combination of pamidronate and calcitriol could completely normalise altered osteoblast function-induced by titanium particles, TNF-[alpha], or both (Fig. 6). Therefore, based on this in vitro investigation, combination therapy with pamidronate and calcitriol may have the potential to prevent or to treat periprosthetic osteolysis and minimise the possible calcaemic side-effects of treatment with calcitriol.
We wish to thank Dr. G. F. Muschler for helping us to establish the method for the isolation of bone marrow-derived osteoblasts, S. Velins, MLA for her assistance and a number of visitors of the Departments of Orthopaedic Surgery and Biochemistry of Rush University, Chicago for their valuable discussions. This work was supported by the grants of the National Institutes of Health and Zimmer Inc (Warsaw, Indiana).
No other benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
1. Merkel KD, Erdmann JM, McHugh KP, et al. Tumor necrosis factor-[alpha] mediates orthopedic implant osteolysis. Am J Pathol 1999;154:203-10.
2. Schwarz EM, Lu AP, Goater JJ, et al. Tumor necrosis factor-[alpha]/nuclear transcription factor-[kappa]B signaling in penprosthetic osteolysis. J Orthop Res 2000;18:472-80.
3. Giant TT, Jacobs JJ, Molnar G, et al. Bone resorption activity of particulate-stimulated macrophages J Bone Miner Res 1993;8:1071-9.
4. Blaine TA, Rosier RN, Puzas JE, et al. Increased levels of tumor necrosis factor-[alpha] and interleukm-6 protein and messenger RNA in human peripheral blood monocytes due to titanium particles. J Bone Joint Surg [Am] 199B;78-A:1181-92.
5. Shanbhag AS, Jacobs JJ, Black J, Galante JP, Giant TT. Human monocyte response to paniculate biomaterials generated in vivo and in vitro. J Orthop Res 1995;13:792-801.
6. Nakashima Y, Sun D-H, Trindade MC, et al. Induction of macrophage C-C chemokine expression by titanium alloy and bone cement particles. J Bone Joint Surg [Br] 1999;81-8:155-62.
7. Yao J, Giant TT, Lark MW, et al. The potential role of fibroblasts in periprosthetic osteolysis: fibroblast response to titanium particles. J Bone Miner Res 1995;10:1417-27.
8. Nakashima Y, Sun D-H, Maloney WJ, et al. Induction of matrix metalloproteinase expression in human macrophages by orthopaedic paniculate debris in vitro J Bone Joint Surg [Br] 1998;80-8:694-700
9. Teitelbaum SL. Bone resorption by osteoclasts. Science 2000;289:1504-8.
10. Kusano K, Miyaura C, lnada M, et al. Regulation of matrix metalloprotemases (MMP-2, -3, -9, and -13) by interleukin-1 and interleukin-B in mouse calvaria: association of MMP induction with bone resorption. Endocrinology 1998;139:1338-45.
11. Dean DD, Schwartz Z, Liu Y, et al. The effect of ultra-high molecular weight polyethylene wear debris on MG-63 osteosarcoma cells in vitro. J Bone Joint Surg [Am] 1999;81-A:452-61.
12. Vermes C, Roebuck KA, Chandrasekaran R, et al. Paniculate wear debris activates protein tyrosine kinases and nuclear factor-kappa B which downregulates type I collagen synthesis in human osteoblasts. J Bone Miner Hes 2000;15:1756-65.
13. Vermes C, Chandrasekaran R, Jacobs JJ, et al. The effects of paniculate wear debris, cytokmes, and growth factors on the functions of MG-63 osteoblasts. J Bone Joint Surg [Am] 2001;83-A:201-11.
14. Takei H, Pioletti DP, Kwon SY, Sung KL. Combined effect of titanium particles and TNF-alpha on the production of II-6 by osteoblast-like cells. J Biomed Mater Res 2000;52:382-7.
15. Shida J, Trindade MCD, Goodman SB, Schurman DJ, Smith RL Induction of interleukin-6 release in human osteoblast-like cells exposed to titanium particles in vitro Calcif Tissue Int 2000;67:151-5.
16. fFritz EA, Giant TT, Vermes C, Jacobs JJ, Roebuck KA. Titanium particles induce the immediate early stress responsive chemokines IL-8 and MCP-1 in osteoblasts. J OrthopRes 2002;20:490-8.
17. Yao J, Cs-Szabo G, Jacobs JJ, Kuettner KE, Giant TT. Suppression of osteoblast function by titanium particles. J Bone Joint Surg [Am] 1997;79-A:107-12.
18. Roebuck KA, Vermes C, Carpenter LR, et al. Downregulation of procollagen [alpha]1[I] mRNA expression by titanium particles correlates with NF-[kappa]B activation and increased Rel A and NF-[kappa]B1 binding to the collagen promoter. J Bone Miner Res 2001;16:501-10.
19. Pioletti DP, Leoni L, Genini D, et al. Gene expression analysis of osteoblastic cells contacted by orthopaedic implant particles J Biomed Mater Res 2002;61:408-20.
20. Majors AK, Boehm CA, Nitto H, Midura RJ, Muschler GF. Characterization of human bone marrow stromal cells with respect to osteoblastic differentiation. J Orthop Res 1997;15:546-57.
21. Kamalia N, McCulloch CA, Tenenbaum HC, Limeback H. Direct flow cytometric quantification of alkaline phosphatase activity in rat bone marrow stromal cells. J Histochem Cytochem 1992;40:1059-65
22. Telford WG, Cox WG, Stiner D, Singer VL, Doty SB. Detection of endogenous alkaline phosphatase activity in intact cells by flow cytometry using the fluorogenic ELF-97 phosphatase substrate. Cytometry 1999;37:314-19
23. Vermes C, Chandrasekaran R, Dobai J, et al. Pamidronate and 1,25-dihydroxy-vitamin-D3 inhibit tumor necrosis factor-alpha (TNF-[alpha])- and wear debris-induced interleukin-6 (IL-6) release and recover suppressed type I collagen synthesis in bone marrow-derived primary human osteoblasts [abstract]. Arthritis & Rheumatism 2001; 44:5355.
24. Muschler GF, Nitto H, Boehm CA, Easley KA. Age- and gender-related changed in the cellularity of human bone marrow and the prevalence of osteoblastic progenitors. J Orthop Res 2001;19:117-25.
25. Pioletti DP, Takei H, Kwon SY, Wood D, Sung K-LP. The cytotoxic effect of titanium particles phagocytosed by osteoblasts. J Biomed Mater Res 1999;46:399-407
26. Horowitz SM, Algan SA, Purdon MA. Pharmacologie inhibition of paniculateinduced bone resorption J Biomed Mater Res 1996:31:91-6.
27. Blaine TA, Pollice PF, Rosier RN, et al. Modulation of the production of cytokines in titanium-stimulated human peripheral blood monocytes by pharmacological agents. J Bone Joint Surg [Am] 1997;79-A:1519-28.
28. Nakashima Y, Sun D-H, Trindade MCD, Maloney WJ, et al. Signaling pathways for tumor necrosis factor-alpha and interleukin-6 expression in human macrophages exposed to titanium alloy particulate debris in vitro. J Bone Joint Surg J [Am] 1999; 81-A:603-15.
29. Haynes DR, Crotti TN, Potter AE, et al. The osteoclastogenic molecules RANKL and RANK are associated with penprosthetic osteolysis. J Bone Joint Surg [Br] 2001;83-B:902-11
30. Zhang X, Morham SG, Langenbach R, et al. Evidence for a direct role of cyclo-oxygenase 2 in implant wear debris- induced osteolysis. J Bone Miner Res 2001;16:660-70
31. Pollice PF, Rosier RN, Looney RJ, et al. Oral pentoxifylline inhibits release of tumor necrosis factor-alpha from human peripheral blood monocytes: a potential treatment for aseptic loosening of total joint components. J Bone Joint Surg [Am] 2001;83-A:1057-61.
32. Schwartz Z, Lohmann CH, Vocke AK, et al. Osteoblast response to titanium surface roughness and 1 alpha,25- (OH)(2)D(3) is mediated through the mitogen-activated protein kmase (MAPK) pathway J Biomed Mater Res 2001;56:417-26.
33. Clohisy JC, Teitelbaum S, Chen S, Erdmann JM, Abu-Amer Y. Tumor necrosis factor-alpha mediates polymethylmethacrylate particle- induced NF-kappaB activation in osteoclast precursor cells. J Orthop Res 2002;20:174-81.
34. Soloviev A, Schwarz EM, Kuprash DV, et al. The role of p105 protein in NFkB activation in ANA-1 murine macrophages following stimulation with titanium particles. J OnhopRes 2002;20:714-22.
35. Greenfield EM, Bi Y, Ragab AA, Goldberg VM, Van De Motter RR. The role of osteoclast differentiation in aseptic loosening. J Orthop Res 2002;20:1-8.
36. Schwarz EM, Benz EB, Lu AP, et al. Quantitative small-animal surrogate to evaluate drug efficacy in preventing wear debris-induced osteolysis. J Orthop Res 2000;18:849-55
37. Childs LM, Paschalis EP, Zing L, et al. In vivo RANK signaling blockade using the receptor activator of BF- kappaB:Fc effectively prevents and ameliorates wear debris-induced osteolysis via osteoclast depletion without inhibiting osteogenesis. J Bone Miner Res 2002;17:192-9.
38. Childs LM, Goater JJ, O'Keefe RJ, Schwarz EM. Effect of anti-tumor necrosis factor-alpha gene therapy on wear debris-induced osteolysis. J Bone Joint Surg [Am] 2001;83-A:1789-97.
39. Childs LM, Goater JJ, O'Keefe RKJ, Schwarz EM. Efficacy of etanercept for wear debris-induced osteolysis J Bone Miner Hes 2001;16:338-47.
40. Goater JJ, O'Keefe RJ, Rosier RN, Puzas JE, Schwarz EM. Efficacy of ex vivo OPG gene therapy in preventing wear debris induced osteolysis J Orthop Res 2002; 20169-73.
41. Ulrich-Vinther M, Carmody EE, Goater JJ, et al. Recombinant adeno-associated virus-mediated osteoprotegerm gene therapy inhibits wear debris-induced osteolysis. J Bone Joint Surg [Am] 2002;84-A:1405-12.
42. Fleisch H. Bisphosphonates: mechanisms of action. Endocr Rev 1998;19:80-100.
43. Brown AJ. Therapeutic uses of vitamin D analogues. Am J Kidney Dis 2001;38 (Suppl 5):3-19
44. Reinholz GG, Getz B, Pederson L, et al. Bisphosphonates directly regulate cell proliferation, differentiation, and gene expression in human osteoblasts Cancer Res 2000;60:6001-7
45. Mathov I, Plotkin LI, Sgarlata CL, Leoni J, Bellido T. Extracellular signal-regulated kinases and calcium channels are involved in the proliferative effect of bisphosphonates on osteoblastic cells in vitro J Bone Miner Res 2001;16:2050-6
46. Viereck V, Emons G, Lauck V, et al. Bisphosphonates pamidronate and zoledronic acid stimulate osteoprotegerm production by primary human osteoblasts. Biochem Biophys Res Commun 2002;291:680-6
47. Theill LE, Boyle WJ, Penninger JM. RANK-L and RANK: T cells, bone loss, and mammalian evolution. Annu Rev Iminunol 2002;20:795-823.
48. Adebanjo OA, Moonga BS, Yamate T, et al. Mode of action of interleukin-6 on mature osteoclasts: novel interactions with extracellular Ca^sup 2+^ sensing in the regulation of osteoclastic bone resorption. J Cell Biol 1998;142:1347-56
49. Vermes C, Jacobs JJ, Zhang J, et al. Shedding of the inlerleukin-6 (IL-6) receptor (gp80) determines the ability of IL-B to induce gp130-phosphorylation in human osteoblasts. J Biol Chem 2002;277:16879-87.
50. O'Brien CA, Gubrij I, Lin SC, Saylors RL, Manolagas SC. STAT3 activation in stromal osteoblastic cells is required for induction of the receptor activator of NF-kappaB ligand and stimulation of osteoclastogenesis by gp130-utilizing cytokines or mterleukin-1 but not 1,25-dihydroxyvitamin D3 or parathyroid hormone J Biol Chem 1999;274:19301-8
51. Shanbhag AS, Hasselman CT, Rubash HE. Inhibition of wear debris mediated osteolysis in a canine total hip arthroplasty model Clin Orthop 1997;344:33-43.
52. Millett PJ, Allen MJ, Bostrom MP. Effects of alendronate on particle-induced osteolysis in a rat model. J Bone Joint Surg [Am] 2002;84-A:236-49.
53. Astrand J, Aspenberg P. Reduction of instability-induced bone resorption using bisphosphonates: high doses are needed in rats. Acta Orthop Scand 2002;73:24-30.
54. Wilkinson JM, Stockley I, Peel NF, et al. Effect of pamidronate in preventing local bone loss after total hip arthroplasty: a randomized, double-blind, controlled trial J Bone Miner Res 2001;16:556-64.
55. Venesmaa PK, Kroger HP, Miettinen HJ, et al. Alendronate reduces peri-prosthetic bone loss after uncemented primary total hip arthroplasty: a prospective randomized study J Bone Miner Res 2001;16:2126-31
56. van Leeuwen JP, van Driel M, van den Bernd GJ, Pols HA. Vitamin D control of osteoblast function and bone extracellular matrix mineralization. Crit Rev Eukaryot Gene Expr 2001;11:199-226.
57. Baran DT, Quail JM, Ray R, Leszyk J, Honeyman T. Annexin II is the membrane receptor that mediates the rapid actions of 1alpha, 25-dihydroxyvitamm D(3). J Cell Biochem 2000;78:34-46
58. Erben RG, Mosekilde L, Thomsen JS, et al. Prevention of bone loss in ovariectomized rats by combined treatment with nsedronate and 1a.25-dihydroxyvitamin D3. J Bone Miner Res 2002;17:1498-511.
C. Vermes,
R. Chandrasekaran,
J. G. Dobai,
J. J. Jacobs,
G. B. J. Andersson,
H. An,
N. J. Hallab,
J. O. Galante,
T. T. Giant
From Rush
University Medical
Center, Chicago, USA
* J. J. Jacobs, MD
* G. B. J. Andersson, MD, PhD
* H. An, MD
* N. J. Hallab, PhD
* J. O. Galante, MD, DSc
* T. T. Giant, MD, PhD
Department of Orthopaedic Surgery, Rush University Medical Center, 1735 W. Harrison 706, Chicago, Illinois, 60612, USA.
* C. Vermes, MD
Department of Orthopaedic Surgery, University of Pecs, 13 Ifjusag, Pecs 7624, Hungary.
* R. Chandrasekaran, PhD
* J. G. Dobai, MD
Department of Anatomy, Histology and Embriology, Medical and Health Centre, University of Debrecen, Debrecen, Hungary.
Correspondence should be sent to Dr T. T. Giant.
© 2004 British Editorial Society of Bone and Joint Surgery
doi: 10.1302/0301-620X.86B5. 14552 $2.00
J Bone Joint Surg [Br] 2004;86-B:759-70.
Received 29 April 2003; Accepted after revision 24 November 2003
Copyright British Editorial Society of Bone & Joint Surgery Jul 2004
Provided by ProQuest Information and Learning Company. All rights Reserved