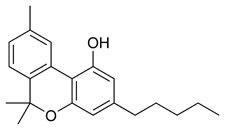
1-Trans-[delta.sup.9]-tetrahydrocannabinol (THC), the main active component of marijuana, has been shown to exhibit anticancer activity (1,2). Galve-Roperh et al. (1) reported that intratumoral administration of THC induces apoptosis of transformed neural cells in culture, and also induces a considerable regression of malignant gliomas in Wistar rats and in mice deficient in recombination activating gene 2. These authors suggest that their "results may provide the basis for a new therapeutic approach for the treatment of malignant gliomas." Regarding this interesting finding, we believe it is important to highlight the previous National Toxicology Program's long-term in vivo bioassay results that showed definite antitumor activity of THC (3,4). This also appears relevant to the current controversy, at least in the United States, regarding the use of marijuana in clinical medicine.
Experimentally, groups of 60-70 male and female rats were administered 0, 12.5, 25, or 50 mg THC/kg body weight (bw), and male and female mice were given 0, 125, 250, or 500 mg THC/kg bw in corn oil by gavage for 104-106 weeks (3,4). During this 2-year period, individual animal body weights were reduced compared to controls, although all groups consumed the same amounts of food. More importantly, survival in all THC groups of male and female rats was significantly greater than the controls. For mice, survival was comparable among groups except for the high-dose males. Clinical findings in the THC groups included lethargy followed by hyperactivity, convulsions, and seizures, which occurred typically during and immediately after dosing or handling.
In both rats and mice, no increased incidences of neoplasms were considered related to the administration of THC (3,4). In fact, for several organ systems the incidences of background tumors in these strains were actually reduced. The incidences of mammary gland fibroadenomas and uterine stromal polyps were decreased in THC groups of female rats, as were incidences of pituitary gland adenomas, interstitial cell adenomas of the testis, and pancreatic adenomas in THC-treated male rats. Concerning nonneoplastic lesions in mice, increases of thyroid gland follicular cell hyperplasia occurred in all THC groups, and increases of forestomach hyperplasia and ulcers occurred in THC groups of male mice; yet, no THC-related tumors were observed to progress from these toxic lesions. This common lack of correlation between toxicity and carcinogenicity has long been known (5-7). Regarding carcinogenic activity of THC in mice, thyroid gland follicular cell adenomas were somewhat increased only in the lowest THC-dosed group of mice (125 mg/kg); thyroid gland follicular cell adenomas were found in 0/62 control males versus 6/60, 3/61, and 1/57 mice treated with 125, 250, and 500 mg THC/kg bw, respectively, and in 4/60 control females versus 9/60, 3/60, and 1/60 mice); these were considered not significantly related to THC (3,4). However, there were significant decreases observed for both benign and malignant liver tumors in male and female mice.
The reduced body weights in these long-term studies may have been contributory to the lowered tumor rates (8-10), as most of the reductions in tumor incidences occurred in hormone-controlled organs (11). This should not detract from the overall antitumor effects of THC observed in both sexes of these species and strains. Until further studies are accomplished, these reductions in tumor incidences in six organs should be considered caused by or associated with administration of THC.
Our 2-year studies (3,4) showed that the observed THC antitumor effects are not confined to the site of injection or administration, and these antitumor effects seem to affect a range of "spontaneous" tumors commonly found in rats and mice. Consequently, the THC-associated antitumor effects are systemically active and are applicable to different tumor types at different organ sites. Again, this lack of specificity might lend credence to the notion that these effects are hormonally mediated and likely related to the observed decreases in body weights. Nonetheless, there were significant reductions in total benign and malignant tumors in all organs combined for both species after THC exposure: in male rats, tumors were found in 98% of controls versus 98, 92, and 90% of groups treated with 12.5, 25, and 50 mg THC/kg bw, respectively; in female rats, tumors were found in 88% of controls versus 82, 86, and 70% of treated groups. Most strikingly, in male mice tumors were found in 73% of controls versus 55, 44, and 30% of male mice treated with 0, 125,250, and 500 mg THC/kg bw, respectively, and in female mice, tumors were found in 77% of controls versus 52, 43, and 27% of treated groups (3,4).
Interestingly, the dose levels used by Galve-Roperh et al. (1) were similar to those used in our studies (3,4). Their findings also agreed with ours in that THC administration did not affect either food or water intake or hematologic profiles and general clinical chemistry of the animals. Perhaps further animal bioassay studies should be done to learn more about the anti-tumor effects of THC. For example, animals could be exposed to known carcinogens (e.g., 9,10-dimethylbenz[a]anthracene exposure resulting in mammary gland tumors) to determine if THC would block this carcinogenic activity, or transgenic animals (12,13) could be used in an attempt to better clarify the mechanism(s) of THC anticarcinogenic activity. More definition of dose-response--antitumor activity relations would be useful, as would studies using paired feeding, to better define the influence of reduced body weight on tumor incidences.
With respect to genetic toxicology (4), THC was not mutagenic in Salmonella typhimurium strains TA97, TA98, TA100, or TA1535 with or without rat and hamster liver S9 fractions. In cultured Chinese hamster ovary (CHO) cells, THC induced sister chromatid exchanges at the highest dose tested in the presence of S9; at this dose level, cell cycle delay indicative of toxicity was observed. THC did not induce chromosomal aberrations in cultured CHO cells with or without S9 metabolic activation enzymes. In vivo, no increase in the frequency of micronucleated erythrocytes was observed in the peripheral blood of male or female mice administered THC by gavage for 13 weeks. Accordingly, THC does not appear to be genotoxic.
Long-term carcinogenesis bioassays have historically and traditionally been used primarily to identify those agents that cause cancer in laboratory animals and hence determine which agents represent a significant cancer risk to humans exposed to these carcinogens (14-16). Conversely, these bioassays can and should also be used to identify potential anticarcinogenic agents (17-19). Thus, in our studies, rats and mice that received THC for 2 years exhibited body weight reductions, enhanced survival rates, and decreased tumor incidences in several sites, mainly organs under hormonal control. These earlier experimental carcinogenesis results on THC (3,4) clearly lend further validity to the notion that cannabinoids may indeed be anticarcinogenic (1,2).
REFERENCES AND NOTES
(1.) Galve-Roperh I, Sanchez C, Cortes ML, del Pulgar TG, Izquierdo M, Guzman M. Anti-tumoral action of cannabinoids: involvement of sustained ceramide accumulation and extracellular signal-regulated kinase activation. Nat Med 6(3):313-319 (2000).
(2.) Piomelli D. Pot of gold for glioma therapy. Nat Med 6(3):255-256 (2000).
(3.) Chan PC, Sills RC, Braun AG, Haseman JK, Bucher JR. Toxicity and carcinogenicity of delta 9-tetrahydro-cannabinol in Fischer rats and B6C3F1 mice. Fundam Appl Toxicol 30(1):109-117 (1996).
(4.) NTP. Toxicology and Carcinogenesis Studies of 1-Trans-[Delta.sup.9]-Tetrahydrocannabinol (CAS No. 1972-08-3) in F344 Rats and B6C3F1 Mice (Gavage Studies). TR 446. Research Triangle Park, NC:National Toxicology Program, 1996.
(5.) Hoel DG, Haseman JK, Hogan MD, Huff J, McConnell EE. The impact of toxicity on carcinogenicity studies: implications for risk assessment. Carcinogenesis 9(11):2045-2052 (1988).
(6.) Huff J. Absence of morphologic correlation between chemical toxicity and chemical carcinogenesis. Environ Health Perspect 101(suppl 5):45-53 (1993).
(7.) Huff J. Chemical toxicity and chemical carcinogenesis. Is there a causal connection? A comparative morphological evaluation of 1500 experiments. IARC Sci Publ 116:437-475 (1992).
(8.) Rao GN, Piegorsch WW, Crawford DD, Edmondson J, Haseman JK. Influence of viral infections on body weight, survival, and tumor prevalence of B6C3F1 (C57BL/6N x C3H/HeN) mice in carcinogenicity studies. Fundam Appl Toxicol 13(1):156-164 (1989).
(9.) Haseman JK, Young E, Eustis SL, Hailey JR. Body weight-tumor incidence correlations in long-term rodent carcinogenicity studies. Toxicol Pathol 25(3):256-263 (1997).
(10.) Haseman JK. The National Toxicology Program experience with dietary restriction: does the manner in which reduced body weight is achieved affect tumor incidence? Int J Toxicol 17(suppl 2):119-134 (1998).
(11.) Huff J, Boyd J, Barrett JC, ads. Cellular and molecular mechanisms of hormonal carcinogenesis: environmental influences. Prog Clin Biol Res 394:1-479 (1996).
(12.) Tennant R. Transgenic mouse models in chemical carcinogenesis studies. Arch Toxicol Suppl 16:261-270 (1994).
(13.) Tennant RW, French JE, Spalding JW. Identifying chemical carcinogens and assessing potential risk in short-term bioassays using transgenic mouse models. Environ Health Perspect 103:942-950 (1995).
(14.) Huff J. Long-term chemical carcinogenesis bioassays predict human cancer hazards. Issues, controversies, and uncertainties. Ann N Y Acad Sci 895:56-79 (1999).
(15.) Huff J. Animal and human carcinogens [Letter]. Environ Health Perspect 107:A341-A342 (1999).
(16.) Huff J. Value, validity, and historical development of carcinogenesis studies for predicting and confirming carcinogenic risks to humans. In: Carcinogenicity Testing, Predicting, & Interpreting Chemical Effects (Kitchin KT, ed). New York:Marcel Dekker, 1999;21-123.
(17.) Douglas JF, Huff J, Peters AC. No evidence of carcinogenicity for L-ascorbic acid (vitamin C) in rodents. J Toxicol Environ Health. 14(4):605-609 (1984).
(18.) Chhabra RS, Huff JE, Haseman J, Hall A, Baskin G, Cowan M. Inhibition of some spontaneous tumors by 4-hexylresorcinol in F344/N rats and B6C3F1 mice. Fundam Appl Toxicol 11(4):685-690 (1988).
(19.) Haseman JK, Johnson FM. Analysis of National Toxicology Program rodent bioassay data for anticarcinogenic effects. Mutat Res 350(1):131-141 (1996).
James Huff Po Chart National Institute of Environmental Health Sciences Research Triangle Park, North Carolina E-mail: huff1@niehs.nih.gov
COPYRIGHT 2000 National Institute of Environmental Health Sciences
COPYRIGHT 2004 Gale Group