Abstract
Incision and drainage combined with antibiotic therapies form the backbone of managing uncomplicated skin and skin structure infections (uSSSIs). An algorithm has been developed to guide the treatment of uSSSIs in the primary care setting in situations where initial empiric therapy is appropriate. This includes instances when a culture is taken, but it is deemed appropriate to begin an antibiotic empirically pending the results of the culture. The panel that developed the algorithm was chaired by Dr. Richard Scher of Columbia University and included thought leaders in the fields of clinical dermatology, dermatologic surgery, infectious disease, pediatric infectious disease, podiatry, and HIV infection.
The panel acknowledged that the initial choice of antibiotic is generally determined by tolerability, ease of administration, cost, and efficacy. The usual choices for initial empiric therapy include cephalosporins, penicillinase-resistant penicillins, and [beta]-lactam/[beta]-lactamase inhibitor combinations. Currently marketed cephalosporins, penicillinase-resistant penicillins, and [beta]-lactam/[beta]-lactamase inhibitor combinations lack activity against methicillin-resistant Staphylococcus aureus (MRSA), and the increasing prevalence of community-acquired MRSA (CA-MRSA) was a major consideration when designing the treatment algorithm. Many CA-MRSA skin infections present as abscess, and drainage is the most important component of therapy in this setting. When the history and physical exam suggest CA-MRSA infection, and there is no fluctuant collection of purulent material to be drained, a sulfa drug or tetracycline is generally the best choice for initial empiric therapy.
Introduction
Up to 17% of dermatology-related clinic consultations involve bacterial skin infections. (1) When skin and skin structure infections (SSSIs) are not complicated, therapy is most often directed against Staphylococcus aureus and Streptococcus pyogenes, the most likely causative organisms. Incision and drainage combined with antibiotic therapies form the backbone of managing uncomplicated (u) SSSIs. (2) When selecting the most appropriate antimicrobial agent, decisions must take into account spectrum of activity, pharmacokinetics, patient characteristics, new treatment options, bacterial resistance, history of allergy, and the risk that the infection is due to methicillin-resistant S. aureus (MRSA).
USSSIs can often be managed successfully in the office setting. A treatment algorithm for initial empiric therapy of uSSSIs has been developed (Figure 1). (3) In some patients, empiric treatment may be initiated without a culture, or it may be initiated while awaiting the results of culture.
The purpose of this paper is to summarize current concepts in the initial empiric treatment of uSSSIs in the ambulatory care setting and to present the initial draft of a treatment algorithm modified for dermatologists who treat uSSSIs.
Therapy
The goals of therapy for uSSSIs are to (1) promptly eradicate the pathogen to obtain early resolution and a low recurrence rate of the infection, (2) minimize the emergence of resistant organisms, and (3) treat the infection safely with well-tolerated agents. Patient history, physical examination data, and (readily available) laboratory data form the basis for diagnosis as well as the decision as to whether the infection is complicated or uncomplicated (Figure 1). Some patients who are immunocompromised, diabetic, or who have significant comorbidities are considered high risk, but it is important to note that skin and skin structure infections in most well-controlled diabetics and most patients with HIV behave no differently than in patients without these disorders.
To Culture or Not To Culture
Results of culture tests confirm the presence of an organism, but the diagnosis of infection remains a clinical assessment. Since most uSSSIs are caused by S. aureus or S. pyogenes, some have questioned whether every infection requires a culture. Generally, physicians weigh the expected benefits of culture and sensitivity testing against the cost to obtain this information. Cultures are not recommended when lesions are not clinically infected and may not be practical when an organism is difficult to isolate. They are generally appropriate when pus is present or when the risk is high for complications, methicillin-resistant S. aureus, or both. Even when a culture is obtained, it may be in the best interest of a given patient to start empiric therapy while awaiting culture results. It is then appropriate to begin empiric therapy on the basis of clinical data and reevaluate the patient when culture results become available. (3) If the culture demonstrates a resistant organism, but the patient is improving clinically, the isolated organism may not be the true pathogen. Alternatively, other interventions such as drainage may result in cure with or without antibiotic therapy to which the organism is sensitive. In either case, it is the patient who is ultimately treated, not the lab result.
Antibiotic Therapy
The recent susceptibility data reported by Sader and colleagues (4) provide a clinical basis for recommending cephalosporins, penicillinase-resistant penicillins, and [beta]-lactam/[beta]-lactamase inhibitor combinations as first choices for the initial empiric treatment of SSSI (Figure 1). Due to their broad-spectrum activity, ease of use, and tolerability, cephalosporins have dominant market share as first-line therapies for uSSSIs. Amoxicillin/clavulanate, though effective, is associated with a higher incidence of gastrointestinal side effects. (3) Semisynthetic penicillins are typically dosed 4 times daily, which may limit compliance.
First generation cephalosporins provide good Gram-positive coverage. Although most third generation cephalosporins are noted for their efficacy against Gram-negative pathogens, cefdinir--an extended-spectrum cephalosporin--is also quite active against gram-positive bacteria such as methicillin-sensitive S. aureus and S. pyogenes. (3) Cefdinir has shown greater potency than older cephalosporins (16-fold better than cephalexin when the MI[C.sub.90] is measured). (4) Since cefdinir, cefixime, ceftibuten, and cefuroxime have no side chains in common with penicillins, they would not be expected to cross react in patients with allergy to penicillin or amoxicillin. (3)
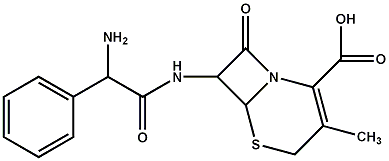
[FIGURE 1 OMITTED]
For children, cefdinir shows comparable efficacy, less likelihood of diarrhea, and better taste than amoxicillin/clavulanate. (5,6)
All antibiotics have some limitations. Fluoroquinolone use is limited by emergent resistance, association with arthropathies in children, increased risk for emergence of MRSA (levofloxacin and ciprofloxacin), and increased risk for Achilles tendon rupture in older adults. (3) Lincosamides (eg, clindamycin) are associated with a significant incidence of diarrhea and have been associated with pseudomembranous colitis. They are commonly reserved for patients with allergy to penicillin or those for whom other antibiotics are unsuitable. It is important to note that erythromycin resistance may be a marker for inducible lincosamide resistance. The trimethoprim/sulfamethoxazole combination is not as effective against streptococci and its use may be limited because of allergy to sulfa drugs. A new oxazolidinedione, linezolid, is best suited for oxacillin-resistant staphylococci, vancomycin-resistant enterococci, and severe cases of MRSA. Some data have suggested that outcomes may be better than with vancomycin in some settings, but the drug is very expensive. Topical antibiotics such as mupirocin are useful for elimination of nasal staphylococcal colonization and the treatment of superficial pyodermias. Some topical antibiotics have been associated with allergic contact dermatitis. (3)
Incision and drainage remains the most important intervention in the treatment of abscesses. (2) A recent study (7) suggests that for pediatric patients with community-acquired (CA) MRSA, incision and drainage was associated with clinical improvement in most of 69 pediatric patients, even those who did not receive MRSA-active antibiotics. (Skin and soft-tissue abscesses were less than 5 cm in diameter.)
Methicillin-Resistant S. Aureus
A major factor in deciding whether to culture is the risk of MRSA. Since MRSA was first identified in the 1960s as a nosocomial pathogen, these organisms--which are not susceptible to [beta]-lactam antibiotics as a class (8)--have been found among hospitals worldwide and risk factors have been identified (Table 1). Since the 1990s, reports have described regional outbreaks of CA-MRSA among wrestlers, (9) child care centers, (10) children without known risk factors, (11) injected-drug users, (12-14) prison inmates, (15) men who have had sex with men, (15) adults aboard a naval ship, (16) professional football players, (17) and healthy people not associated with health care institutions. (2,8,11,18-24)
Unlike nosocomial MRSA infections, CA-MRSA infections are resistant to both [beta]-lactam and macrolide antibiotics, and those with skin infections usually present with abscesses or cellulitis. (17,23) Outside of the skin, MRSA may also cause necrotizing fasciitis and pneumonitis, life-threatening conditions requiring immediate treatment. (18) When the risk of MRSA is high and there is no pus to drain, empiric therapy should be directed toward MRSA. In the setting of skin infections, sulfa and tetracyclines are most commonly chosen. Other options for the treatment of MRSA infections include vancomycin, linezolid, lincosamides, and fluoroquinolones (Figure 1). Emerging resistance has been associated with fluoroquinolones.
New Treatment Algorithm
The current algorithm for the ambulatory care setting (Figure 1) offers guidance for initial empiric antibiotic therapy for uSSSIs, recommends nonpharmacologic therapy such as drainage, and topical antibiotic agents when appropriate, and includes suggestions for treating refractory infections. New algorithms are being developed that include pathways important to dermatologists and podiatrists who treat a wide range of skin infections. Important topics to be addressed include antibiotic prophylaxis of wound infections and bacterial endocarditis, the choice of therapy in patients with a history of penicillin or first generation cephalosporin allergy, and the treatment of foot ulcers in the diabetic patient. An initial draft of one new algorithm is shown in Figure 2.
It must be emphasized that collections of purulent material--abscesses--must be drained. Drainage is the single most important aspect of treatment in these patients, and antibiotic therapy is secondary. For SSSI without collections of purulent material, antibiotics become the primary intervention.
The importance of drainage in the setting of MRSA infection is suggested by the results of Lee and colleagues (7) in which pediatric patients with community-acquired MRSA showed clinical improvement with abscess drainage, even without effective antibiotic therapy. In a more recent analysis of patients with confirmed community-acquired MRSA, Fridkin and colleagues (8,23) found that, counter-intuitively, outcomes of most patients started on an MRSA-resistant antibiotic were more favorable than patients started on other therapies. The authors attributed this surprising result to the fact that most patients receiving MRSA-resistant agents had abscesses that had been incised and drained, indicating that drainage takes precedence over antibiotic therapy in patients with CA-MRSA.
[FIGURE 2 OMITTED]
An algorithm for dermatologists should take into account that dermatologists are more likely than primary care physicians to (1) treat complicated (c) SSSIs as well as uSSSIs, (2) drain complex abscesses by surgery, (3) treat refractory infections and MRSA infections, and (4) prescribe perioperative antibiotic therapy.
An algorithm for dermatologists should reference guidance for preventing bacterial endocarditis. (26) Prophylaxis for cutaneous surgery and for endocarditis are discussed in detail by Mark S. Nestor, MD, PhD in this supplement.
Conclusions
The treatment of SSSIs--uncomplicated and complicated--remains a challenge, particularly with the increasing prevalence of MRSA and the development of new therapeutic choices. New algorithms should be developed and current algorithms revised to reflect changes in resistance patterns and new treatment options for both primary care physicians and specialists treating SSSIs.
Dr. Elston is a consultant for and serves on the Speakers Bureau of Abbott Laboratories.
References
1. Schaper NC, Apelqvist J, Bakker K. The international consensus and practical guidelines on the management and prevention of the diabetic foot. Curr Diab Rep. 2003;3:475-479.
2. Iyer S, Jones DH. Community-acquired methicillin-resistant Staphylococcus aureus skin infection: a retrospective analysis of clinical presentation and treatment of a local outbreak. J Am Acad Dermatol. 2004;50:854-858.
3. Scher RK, Elston DM, Hedrick JA, Joseph WS, Maurer T, Murakawa GJ. Treatment options in the management of uncomplicated skin and skin structure infections. Cutis. 2005;75(1 Suppl):3-23.
4. Sader HS, Streit JM, Fritsche TR, Jones RN. Potency and spectrum reevaluation of cefdinir tested against pathogens causing skin and soft tissue infections: a sample of North American isolates. Diagn Microbiol Infect Dis. 2004;49:283-287.
5. Steele RW, Thomas MP, Begue RE et al. Compliance issues related to the selection of antibiotic suspensions for children. Pediatr Infect Dis J. 2001;20:1-5.
6. Powers JL, Gooch WM 3rd, Oddo LP. Comparison of the palatability of the oral suspension of cefdinir vs. amoxicillin/clavulanate potassium, cefprozil and azithromycin in pediatric patients. Pediatr Infect Dis J. 2000;19 (12 Suppl):S174-S180.
7. Lee MC, Rios AM, Aten MF, et al. Management and outcome of children with skin and soft tissue abscesses caused by community-acquired methicillin-resistant Staphylococcus aureus. Pediatr Infect Dis J. 2004;23:123-127.
8. Fridkin SK, Hageman JC, Morrison M, et al. Methicillin-resistant Staphylococcus aureus disease in three communities. N Engl J Med. 2005;352:1436-1444.
9. Lindenmayer JM, Schoenfeld S, O'Grady R, Carney JK. Methicillin-resistant Staphylococcus aureus in a high school wrestling team and the surrounding community. Arch Intern Med. 1998;158:895-899.
10. Adcock PM, Pastor P, Medley F, Patterson JE, Murphy TV. Methicillin-resistant Staphylococcus aureus in two child care centers. J Infect Dis. 1998;178:577-580.
11. Herold BC, Immergluck LC, Maranan MC, et al. Community-acquired methicillin-resistant Staphylococcus aureus in children with no identified predisposing risk. JAMA. 1998;279:593-598.
12. Centers for Disease Control and Prevention. Soft tissue infections among injection drug users--San Francisco, California, 1996-2000. JAMA. 2001;285:2707-2709.
13. Fleisch F, Zbinden R, Vanoli C, Ruef C. Epidemic spread of a single clone of methicillin-resistant Staphylococcus aureus among injection drug users in Zurich, Switzerland. Clin Infect Dis. 2001;32:581-586.
14. Charlebois ED, Bangsberg DR, Moss NJ, et al. Population-based community prevalence of methicillin-resistant Staphylococcus aureus in the urban poor of San Francisco. Clin Infect Dis. 2002;34:425-433.
15. Centers for Disease Control and Prevention (CDC). Outbreaks of community-associated methicillin-resistant Staphylococcus aureus skin infections--Los Angeles County, California, 2002-2003. MMWR Morb Mortal Wkly Rep. 2003;52:88.
16. LaMar JE, Carr RB, Zinderman C, McDonald K. Sentinel cases of community-acquired methicillin-resistant Staphylococcus aureus onboard a naval ship. Mil Med. 2003;168:135-138.
17. Kazakova SV, Hageman JC, Matava M, et al. A clone of methicillin-resistant Staphylococcus aureus among professional football players. N Engl J Med. 2005;352:468-475.
18. Miller LG, Perdreau-Remington F, Rieg G, et al. Necrotizing fasciitis caused by community-associated methicillin-resistant Staphylococcus aureus in Los Angeles. N Engl J Med. 2005;352:1445-1453.
19. Carleton HA, Diep BA, Charlebois ED, Sensabaugh GF, Perdreau-Remington F. Community-adapted methicillin-resistant Staphylococcus aureus (MRSA): population dynamics of an expanding community reservoir of MRSA. J Infect Dis. 2004;190:1730-1738.
20. Vandenesch F, Naimi T, Enright MC, et al. Community-acquired methicillin-resistant Staphylococcus aureus carrying Panton-Valentine leukocidin genes: worldwide emergence. Emerg Infect Dis. 2003;9:978-984.
21. Morin CA, Hadler JL. Population-based incidence and characteristics of community-onset Staphylococcus aureus infections with bacteremia in 4 metropolitan Connecticut areas, 1998. J Infect Dis. 2001;184:1029-1034.
22. Naimi TS, LeDell KH, Como-Sabetti K, et al. Comparison of community- and health care-associated methicillin-resistant Staphylococcus aureus infection. JAMA. 2003;290:2976-2984.
23. Cohen PR, Kurzrock R. Community-acquired methicillin-resistant Staphylococcus aureus skin infection: an emerging clinical problem. J Am Acad Dermatol. 2004;50:277-280.
24. Young DM, Harris HW, Charlebois ED, et al. An epidemic of methicillin-resistant Staphylococcus aureus soft tissue infections among medically underserved patients. Arch Surg. 2004;139:947-951.
25. Chambers HF. Community-associated MRSA--resistance and virulence converge. N Engl J Med. 2005;352:1485-1487.
26. Dajani AS, Taubert KA, Wilson W, et al. Prevention of bacterial endocarditis: recommendations by the American Heart Association. Clin Infect Dis. 1997;25:1448-1458.
Address for Correspondence
Dirk M. Elston MD
Geisinger Medical Center
100 N Academy Ave
Danville, PA 17822-9800
Phone: 570-271-8050
e-mail: dmelston@geisinger.edu
Dirk M. Elston MD
Geisinger Medical Center, Danville, PA
COPYRIGHT 2005 Journal of Drugs in Dermatology, Inc.
COPYRIGHT 2005 Gale Group