Soy protein, when substituted for animal protein in the diet, will lower blood cholesterol. Recent research also provides evidence that soy protein and/or isoflavones may improve endothelial functioning and attenuate events leading to both lesion and thrombus formation.
Introduction
Soy protein, when substituted for animal protein in the diet, will lower blood cholesterol levels. In humans, the primary reduction of cholesterol is noted in the low-density lipoprotein (LDL) cholesterol fraction, whereas highdensity lipoprotein (HDL) cholesterol either remains unchanged or is increased.'2 In addition, a significant reduction in total triglycerides has been reported in several studies and was noted in the meta-analysis by Anderson et al.1 Thus, the literature indicates that the dietary substitution of soy protein for animal protein will promote a decrease in the risk of cardiovascular disease by lowering circulating LDL cholesterol concentrations. This review describes the potential mechanisms by which soy protein lowers cholesterol concentrations and explores what the responsible bioactive component might be.
Potential Mechanisms
Many researchers over the past 30 years have speculated about what the potential mechanism(s) for the cholesterollowering effect of soy protein might be. It has been argued that there is an interruption in intestinal absorption of bile acids and dietary cholesterol when soy protein is consumed (Figure 1). This has been routinely reported in animal studies but not in earlier human studies that measured fecal bile/cholesterol excretion.3-7 More recently, Wong et al.8 found increases in the pool size of chenodeoxycholic acid in humans fed soy protein, but neither cholesterol absorption nor cholic acid pool size was affected. It would be interesting to investigate this area in human trials again.
Another proposed mechanism is that hepatic metabolism of cholesterol and/or lipoproteins is altered when soy protein is ingested (Figure 1). Khosla et al.9 found that removal of LDL from circulation is significantly enhanced in rabbits fed soy protein. Increases in apo B/E receptor activity have also been reported in other animal models.10 In humans, Lovati et al.11 reported a sevenfold increase in monocyte LDL receptor activity in hypercholesterolemic individuals who consumed soy protein. Data from our laboratory indicate that LDL receptor mRNA levels in mononuclear cells were increased 75% in subjects consuming soy protein compared with casein.2 With regard to the metabolism of cholesterol, studies in animals have shown that soy protein consumption increases activities of HMG CoA reductase and cholesterol 7alpha-hydroxylase (see references 6 and 7 for reviews).
Others have speculated that soy protein affects various aspects of the endocrine system. Forsythe12 first postulated that substituting soy protein for animal protein modulates thyroid hormone status within the body. This theory was backed by the knowledge that there is an inverse relationship between circulating thyroxin and total cholesterol concentrations and that increases in thyroxin, accompanied by decreases in cholesterol concentrations, were observed in studies with gerbils. Our laboratory, however, investigated this phenomenon in several studies in animals and humans and did not find consistent results. In one study with gerbils, soy protein concentrate and soy protein isolate significantly reduced total and LDL cholesterol concentrations, but only soy protein isolate increased thyroid hormone concentrations.13
Results are also inconsistent in humans. We found that 50 g soy protein/day significantly increased thyroxin levels to a very modest degree in men.14 However, when 25 g soy protein was fed in a subsequent study, there was no modification of thyroid hormone status, even though hypercholesterolemic subjects did experience a significant drop in total cholesterol concentrations.15,16
In addition to possible influences of soy on thyroid hormone status, soybeans naturally produce estrogenlike molecules, isoflavones, in response to environmental stress to the plant during cultivation.17 These are known to have weak estrogenic activity in biologic systems. Thus, it is increasingly popular to speculate that the mechanism by which soy protein decreases blood cholesterol is via "estrogenic" effects stimulated by ingestion of isoflavones.6.18
Bioactive Components
The bioactive component responsible for changes in blood lipids still remains to be identified, although major steps toward this end have been taken in the past few years. Potential components have been investigated and are reviewed elsewhere.6 This review will focus on amino acids/ peptides, fiber, and isoflavones.
Amino Acids/Peptides
With respect to the intact protein, studies have shown that dietary substitution of amino acids patterned after soy protein produces significantly lower blood cholesterol concentrations compared with amino acids patterned after casein. The extent of cholesterol lowering is, however, not as great compared with values in animals fed intact soy protein.19,20 Further work has shown that various storage proteins from soybeans (e.g., the 7S and 11 S globulins) have pronounced effects on hepatic LDL metabolism in vitro.21
Sugano and associates have found potent effects from a hydrolytic fraction of soy protein.22,23 These researchers have shown that when isolated soy protein is subjected to microbial proteases or pepsin, two distinct fractions are formed: an insoluble, high-molecular-weight fraction and a soluble, lower-molecular-weight fraction. The high-molecular-weight fraction (HMF) is very potent in lowering cholesterol and produces significant reductions compared with the soluble fraction and intact isolated soy protein. According to these authors, the HMF contains hydrophobic peptides that are very good at binding bile acids in vitro.23 In fact, when HMF is fed, fecal weight and both neutral and acidic steroid excretion are enhanced significantly. It is interesting that further treatment of the HMF with water washing improves the cholesterol-lowering ability whereas methanol washing diminishes its effect, and that the effect appears to be independent of the saponin content of the fractions tested. This is a very intriguing area that warrants further exploration.
Fiber
Fiber also has been postulated to be the bioactive ingredient in various soy protein preparations. Lo24 reviewed data on soy fiber and reported that the addition of soy cotyledon fiber to the diets of hypercholesterolemic individuals is effective in reducing total and LDL cholesterol. However, we failed to find augmentation of the cholesterol-lowering effect of soy protein by adding soy fiber to the diets of mildly hypercholesterolemic men in two studies.16,25 Our results indicated that soy protein plus soy fiber was no more effective than soy protein plus cellulose (a fiber known not to affect lipidemia) in lowering blood lipids in mildly hypercholesterolemic men. In addition, a number of studies in humans and animals show that isolated soy protein, which is 90% protein and contains virtually no soy fiber, results in significant depressions in total and LDL cholesterol in both animals and humans.1,26 Thus, the fiber component of soybeans is probably not responsible for the cholesterol-lowering effect of soy protein.
Isoflavones
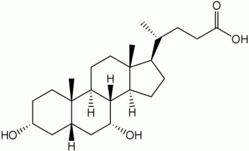
The isoflavones that exist naturally in soy products are composed of 12 different isomers including genistein, genistin, 6"-O-acetylgenistin, 6"-O-malonylgenistin, daidzein, daidzin, 6"-O-acetyldaidzin, 6"-O-malonyldaidzin, glycitein, glycitin, 6"-O-acetylglycitin, and 6"-O-malonylglycitin (Figure 2). The overall quantities and the proportion present are related to the type of soy product and the type of processing employed to produce the product. In manufacturing procedures that use excessive water and/ or organic washings, isoflavone levels are reduced relative to products that are minimally processed.
Because isoflavones have structures similar to mammalian estrogens and they bind with estrogen receptors,27 exhibiting a higher affinity for the beta receptor,28 it has been postulated that they may be responsible for the effects soy protein has on blood lipids. It is well known that mammalian estrogens have a significant impact on blood lipid profiles, promoting decreases in LDL and increases in HDL cholesterol. Estradiol also has a potent cardioprotective effect on blood vessels. Interestingly, similar modifications in blood lipids and blood vessels are noted with soy protein consumption.
Effects Beyond Cholesterol Lowering
Huff et al.29 have shown that replacing casein with soy protein will decrease the extent of atherosclerotic lesion formation in rabbits. Anthony et al.30 and Honore et al.31 also have shown that soy protein decreases lesion formation in nonhuman primates. Their research indicates that the bioactive component of soy responsible for this is likely the isoflavones. In Anthony et al.'s30 work, a diet containing isolated soy protein with naturally occurring isoflavones (soy+) was compared with a diet containing isolated soy protein that had undergone alcohol washing, which removes isoflavones (soy-), and with a diet containing casein as the protein source. They found that nonhuman primates fed the soy+ diet had significant decreases in atherosclerotic plaque compared with groups fed either the casein diet or the soy- diet, which had an intermediate nonsignificant reduction. They also found that the cholesterol-lowering ability of soy protein was lost in the soygroup.
Honore et al.31 showed that one of the key isoflavones, genistein, is responsible for enhancement of vascular reactivity. They also compared a soy+ diet with a soy- diet. Females fed the soy+ diet had dilationary responses to acetylcholine infusion (i.e., the endothelial cells were functioning normally) whereas the soy- diet produced constriction. Genistein was then injected intravenously, which also elicited a dilationary response to acetylcholine in females. Interestingly, in the male nonhuman primates in this study, there was a slight improvement in response to acetlycholine, but it was not statistically significant.
There also is evidence suggesting that genistein has inhibitory effects on activities leading to initial lesion formation as well as thrombus formation (Figure 1). These inhibitory effects may be either independent effects of genistein, perhaps acting as an estrogen, or responses related to suppression of inflammation. Early atherogenesis has been proposed to be a result of inflammation leading to monocyte adhesion.32,33 Furthermore, events subsequent to plaque rupture are associated with a cascade of events leading to thrombus formation and subsequent inflammation.34,35 In both cases, genistein is a wellknown inhibitor of tyrosine kinase.36 Tyrosine kinase is active in the cascade of events that occur in the formation of thrombi as well as in tissues that are actively producing lesions.37,38 Therefore, if the environment is rich in genistein (and possibly other isoflavones), these types of responses may be actively shut down. This should result in depression in plaque formation as well as decreased chance of clot formation upon plaque rupture, thereby attenuating risk of ischemia. This also suggests that isoflavones may be of use in decreasing rates of restenosis via depressing inflammation associated with balloon angioplasty and placement stents.
To complicate matters, it appears that in humans, isoflavones alone will not promote healthy arteries or decreases in blood lipids. In a recent study by Nestel et al.,39 blood lipid profiles were not improved in postmenopausal women consuming tablets containing 80 mg soy isoflavones (aglycone units) compared with women consuming a placebo. Furthermore, vascular reactivity was not improved although systemic arterial compliance was improved. This confirms findings in nonhuman primates presented by Greaves et al.,40 who showed that isoflavone extracts had no impact on blood lipid profiles. In addition, Crouse et al.41 recently presented findings from their human study showing that alcohol-extracted soy protein, as well as casein, was ineffective in lowering LDL cholesterol, whereas soy protein preparations containing at least 38 mg total aglycone isoflavones/25 g protein significantly lowered LDL cholesterol in individuals with high blood lipids upon entry to the study. Conversely, Sirtori et al.,42 in a letter to the editor, stated that the soy flour products used in their studies in Italy did not contain isoflavones. However, it appears that there is some synergy between the protein component and isoflavones related to overall vascular health.
Conclusion
Coronary heart disease is the leading cause of death of Americans and residents of other industrialized societies. In the United States, coronary heart disease was responsible for the deaths of more than 960,000 individuals, or 41.5% of all deaths in 1995.43 Current treatments include dietary modification to alter plasma lipids and, thus, decrease lesion formation. Other lines of treatment include several drugs that are very effective in lowering blood lipids via inhibition of HMG CoA reductase or sequestration of bile acids gastrointestinally. Soy protein may provide a viable alternative for individuals attempting to modify their risk for CHD without taking medication.
Anderson JW, Johnstone BM, Cook-Newell ME. Meta-analysis of the effects of soy protein intake on serum lipids. N Engl J Med 1995;333:276-82
Baum J, Teng HY, Erdman JW Jr, et al. Long-term intake of soy protein lowers the risk of cardiovascular disease and increases mononuclear cell LDL receptor mRNA in hypercholesterolemic postmenopausal women. Am J Clin Nutr (in press)
Fumagalli R, Soleri L, Farini R, et al. Fecal cholesterol excretion in type II hypercholesterolemic patients treated with soybean protein diet. Atherosclerosis 1982;43:341-53
Noseda G, Fragiacomo C, Descovich GC, et al. Clinical studies on the mechanism of action of the soybean protein diet. In: Fumagalli Ft, Kritchevsky D, Paoletti R, eds. Drugs affecting lipid metabolism. Amsterdam: Elsevier/North Holland Biochemical Press, 1980;355-62
Roda E, Mazella G, Cornia GL, et al. Effects of soybean protein-rich diet on biliary lipid composition. In: Barbara L, Miglioli M, Phillips SF, eds. New trends in pathophysiology and therapy of the large bowel. Amsterdam: Elsevier/North Holland Biochemical Press, 1983;309-12
Potter SM. Overview of possible mechanisms for the hypocholesterolemic effect of soy protein. J Nutr 1995;125:606S-11S
Potter SM. Soy protein and serum lipids. Curr Opin Lipidol 1996;7:260-4
Wong WW, Hachey DL, O'Brian Smith E, et al. Mechanisms for the hypocholesterolemic effect of soy protein in normocholesterolemic and hypercholesterolemic men. Proceedings of the Second International Symposium on the Role of Soy in Preventing and Treating Chronic Disease,1996;25
Khosla P, Samman S, Carroll KK. Decreased receptor-mediated LDL catabolism in casein-fed rabbits precedes the increase in plasma cholesterol levels. J Nutr Biochem 1991;2:203-9
Sirtori CR, Galli G, Lovati MR, et al. Effects of dietary proteins on the regulation of liver lipoprotein receptors in rats. J Nutr 1984;114:1493-1500
11. Lovati MR, Manzoni C, Canavesi A, et al. Soybean protein diet increases low-density lipoprotein receptor activity in mononuclear cells from hypercholesterolemic patients. J Clin Invest 1987;80: 1498-1502
12. Forsythe WA Ill. Comparison of dietary casein or
soy protein effects on plasma lipids and hormone concentrations in the gerbil. J Nutr 1986;116:116571
13. Potter SM, Berber-Jimenez MD, Pertile J. Protein from soy concentrate and isolated soy protein alters blood lipids and hormones differently. vI Nutr 1996; 126:2007-11
14. Ham JO, Chapman KM, Essex-Sorlie D, et al. Endocrinological responses to soy protein and fiber in mildly hypercholesterolemic men. Nutr Res 1993;13:873-84
15. Balmir F, Potter SM, Essex-Sorlie D, et al. Endocrinological responses to soy protein and soy fiber in mildly hypercholesterolemic men (25 g study). FASEB J 1993;7:A802
16. Bakhit RM, Klein BP, Essex-Sorlie D, et al. Intake of 25 g soy protein reduces plasma cholesterol in men with elevated cholesterol concentrations. J Nutr 1994;124:213-22
17. Graham TL, Graham MY Signaling in soybean phenylpropanoid responses: dissection of primary, secondary, and conditioning effects of light, wounding and elicitor treatments. Plant Physiol 1996; 110:1123-33
18. Anthony MS, Clarkson TB, Hughes CL Jr, et al. Soybean isoflavones improve cardiovascular risk factors without affecting the reproductive system of peripubertal rhesus monkeys. J Nutr 1996;126:4350
19. Huff MW, Carroll KK. Effects of dietary proteins and amino acid mixtures on plasma cholesterol levels in rabbits. J Nutr 1980;110:1676-85 20. Tasker T, Potter SM. Influence of dietary proteins and amino acid variation on plasma lipids, HMG CoA reductase activity, and reduced glutathione concentrations in inbred versus outbred gerbils. J Nutr Biochem 1993;4:458-62
21. Lovati MR, Manzoni C, Corsini A, et al. Low-density lipoprotein receptor activity is modulated by soybean globulins in cell culture. J Nutr 1992;122: 1971-8
22. Sugano M, Yamada Y, Yoshida K, et al. The hypocholesterolemic action of the undigested fraction of soybean protein in rats. Atherosclerosis 1988;72:115-22
23. Sugano M, Goto S, Tamada Y et al. Cholesterollowering activity of various undigested fractions of soybean protein in rats. J Nutr 1990;120:977-85 24. Lo GS. Physiological effects of physico-chemical properties of soy cotyledon fiber. In: Gurda I, Brine CJ, eds. New developments in dietary fiber. New York: Plenum Press, 1990;49-66
25. Potter SM, Bakhit RM, Essex-Sorlie D, et al. Depression of plasma cholesterol in men by consumption of baked products containing soy protein. Am J Clin Nutr 1993;58:501-6
26. Carroll KK. Review of clinical studies on cholesterol-lowering response to soy protein. J Am Diet Assoc 1991;91:820-7
27. Shutt DA, Cox RI. Steroid and phytoestrogen binding to sheep uterine receptors in vitro. J Endocrinol 1972;52:299-310
28. Kuiper GGJM, Carlsson B, Grandien K, et al. Comparison of the ligand binding specificity and transcript tissue distribution of estrogen receptors and
B. Endocrinology 1997;138:863-70 29. Huff MW, Roberts D, Carroll KK. Long-term effects of semipurified diets containing casein or soy protein isolate on atherosclerosis and plasma lipoproteins in rabbits. Atherosclerosis 1982;41:32736
30. Anthony MS, Clarkson TB, Bullock BC, Wagner JD. Soy protein versus soy phytoestrogens in the prevention of diet-induced coronary artery atherosclerosis of male cynomolgus monkeys. Arterioscler Thromb Vasc Biol 1997;17:2524-31 31. Honore EK, Williams JK, Anthony MS, Clarkson TB. Soy isoflavones enhance coronary vascular reactivity in atherosclerotic female macaques. Fertil Steril 1997;67:148-54
32. Cybulsky Ml, Gimbrone MA. Endothelial expression of a mononuclear leukocyte adhesion molecule during atherogenesis. Science 1991;251: 788-91
33. Ridker PM. Inflammation, infection, and cardiovascular risk: how is food the clinical evidence? Circulation 1998;97:1671-4
34. Entman ML, Ballantyne CM. Inflammation in acute coronary syndromes. Circulation 1993;88:800-3 35. van der Wal AC, Becker AE, van der Loos CM, Das PK. Site of intimal rupture or erosion of thrombosed coronary atherosclerotic plaques is characterized by an inflammatory process irrespective of the dominant plaque morphology. Circulation 1994;89:36-44 36. Ogawara H, Akiyama T, Watanabe S, et al. Inhibition
of tyrosine protein kinase activity by synthetic isoflavones and flavones. J Antibiotic 1989;42:34S 3
37. Raines EW, Ross R. Biology of atherosclerotic plaque formation: possible role of growth factors in lesion development and the potential impact of soy. J Nutr 1995;125(suppl):624-30
38. Wilcox JN, Blumenthal BF Thrombic mechanisms in atherosclerosis: potential impact of soy proteins. J Nutr 1995;125(suppl):631-8
39. Nestel PJ, Yamashita T, Sasahara T, et al. Soy isoflavones improve systemic arterial compliance but not plasma lipids in menopausal and perimenopausal women. Arterioscler Thromb Vasc Biol 1997;17:3392-8
40. Greaves KA, Zhang LZ, Williams JK, et al. Phytoestrogens and intact soy protein administration differ in their effects on plasma lipids and lipoproteins. Proceedings of the Symposium on Phytoestrogen Research Methods,1997 41. Crouse JR III, Terry JG, Morgan TM, et al. Soy protein containing isoflavones reduces plasma concentrations of lipids and lipoproteins. Circulation 1998;97:816
42. Sirtori CR, Gianazza E, Manzoni C, et al. Role of isoflavones in cholesterol reduction by soy proteins in the clinic. Am J Clin Nutr 1997;65:166-71
43. American Heart Association.1998 heart and stroke statistical update. Dallas, TX: American Heart Association, 1997
Dr. Potter is currently with the Department of Nutritional Sciences, Protein Technologies International, St. Louis, MO 03164, USA. She was formerly an Associate Professor of Nutrition at the University of Illinois, where she conducted research on soy and heart disease.
Copyright International Life Sciences Institute and Nutrition Foundation Aug 1998
Provided by ProQuest Information and Learning Company. All rights Reserved