Although aspirin therapy before and after percutaneous coronary intervention (PCI) procedures can improve patient outcomes, ischemic events are still relatively common and can lead to significant morbidity and mortality. The most common ischemic complications of PCI are platelet-related events caused by thrombosis at the site of the procedure and/or embolism of platelet thrombi. Mehta and colleagues studied the effect of adding antiplatelet therapy to aspirin prophylaxis in patients undergoing PCI.
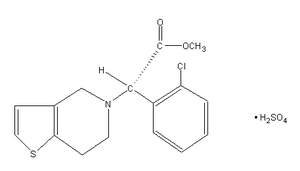
From a large international study of acute coronary syndrome, the authors recruited patients within 24 hours of the onset of symptoms. Patients had to have evidence of new ischemia, such as significant elevation of cardiac enzyme levels, but less than 1-mm ST-segment elevation on electroencephalography. Patients with a recent history of anticoagulation or contraindications to antithrombotic medications were excluded. The patients were randomly allocated to adjunctive therapy with clopidogrel or placebo. All patients received aspirin in a dosage of 75 to 325 mg daily and were scheduled for PCI. Clopidogrel was given as a 300-mg loading dose, followed by daily therapy for an average of six days before PCI and up to eight months after. The main outcomes monitored were cardiovascular death, myocardial infarction, or urgent revascularization procedure within 30 days of PCI.
Data were available for more than 1,300 patients in each treatment group. These patients were well matched in baseline characteristics, and most patients in each group received intracoronary stents. Patients treated with clopidogrel had significantly fewer cardiovascular deaths and myocardial events during the study than patients treated with placebo (8.8 percent and 12.6 percent, respectively). This advantage was apparent in all subgroups of patients examined and was measurable before and after the PCI procedure. Minor bleeding occurred in approximately 2 percent of patients treated with placebo and 3.5 percent of patients treated with clopidogrel. Major bleeding occurred in fewer than 3 percent of patients in each group.
The authors conclude that adding clopidogrel to aspirin therapy reduces the incidence of cardiovascular events in patients undergoing PCI procedures for acute coronary syndrome.
2001;358:527-33.
COPYRIGHT 2002 American Academy of Family Physicians
COPYRIGHT 2002 Gale Group