* EVIDENCE-BASED ANSWER
Stimulant medication therapy is the most effective treatment for attention deficit/hyperactivity disorder (ADHD) in children, producing significant improvements in symptoms and modest improvements in academic achievement (strength of recommendation [SOR]: A, based on multiple randomized controlled trials [RCTs]). Nonpharmacologic therapies, such as behavior therapy, school-based interventions, and family therapy, are not as effective as stimulants but may add modest benefit to the effects of medication (SOR: B, based on 1 RCT).
While atomoxetine (Strattera) improves the symptoms of ADHD (SOR: A, based on multiple RCTs), stimulant medications other than methylphenidate offer no distinct short-term advantages (SOR: A, based on meta-analyses of multiple RCTs). Combination drug therapies offer no significant advantage to stimulants alone unless a comorbid condition is present (SOR: A, based on a meta-analysis of 20 RCTs).
The combination of methylphenidate and clonidine (Catapres) improves symptoms in children with both ADHD and tics (SOR: B, based on 1 RCT). Clonidine is less effective alone and has significant side effects (SOR: B, based on a meta analysis of nonrandomized trials).
* EVIDENCE SUMMARY
In numerous systematic reviews, RCTs, and meta-analyses, 70% of children responded to stimulant medications with short-term improvements in ADHD symptoms (inattention and hyperactivity/ impulsivity) and academic achievement. A forty-year review looked at 135 trials and 413 RCTs of methylphenidate in over 19,000 children with an average age of 8.8 years (range, 8.3-9.4 years) for an average duration of 6 weeks (range, 3.3-8.0 weeks). (1-3)
Study groups included mostly elementary school-aged male children, with few minorities represented. Comorbid conditions, present in 65% of children with ADHD, were often poorly controlled. Outcome measures varied among studies. (3)
The effect size from stimulant medication in these studies averaged 0.8 for symptom relief and between 0.4 and 0.5 for academic achievement. (Effect size is the difference between the means of the experimental and control groups expressed in standard deviations. An effect size of 0.2 is considered small, 0.5 is medium, and 0.8 is considered moderate to large.)
A large randomized trial of 579 children with ADHD (20% girls) aged 7 to 9.9 years compared outcomes of 4 treatment strategies: stimulant medication, intensive behavioral treatment, combined stimulant medication and behavioral interventions, and standard community care. (4) All children met the DSM-IV criteria for ADHD Combined Type (the most common type of ADHD in this age group). The stimulant medication strategy included an initial dose titration period followed by monthly 30-minute visits. Intensive behavioral treatment involved child, parent, and school personnel components of therapy. Combination therapy added the regimens for medication and behavioral treatment together. Standard community care consisted of usual (nonsystematic) care, evaluated at 6 different sites.
After 14 months of treatment, children in the medication group and the combined treatment groups showed more improvement in ADHD symptoms than children given intensive behavioral treatment or those who received standard community care. When combined with medication, those treated with behavioral therapy showed slight improvement in social skills, anxiety, aggression, oppositional behavior, and academic achievement over medication alone. At the conclusion of the study, 74% of the 212 children on medication were successfully maintained on methylphenidate alone, 10% required dextroamphetamine, and no children required more than one medication. This study found that higher doses of medication with more frequent office follow-up and regular school contact were important features of successful treatment. Only 40% of families were able to complete the intensive behavioral therapy.
Several short-term reviews and meta-analyses show that side effects from stimulant medications are mild and have short duration? More long-term studies are required to evaluate effects on growth. RCTs have limited power to detect rare adverse events that may be better detected by large observational studies. (6)
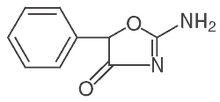
Atomoxetine, a specific norepinephrine reuptake inhibitor, is an FDA-approved alternative to stimulants for ADHD treatment in children and adolescents. Based on 3 RCTs (7) of 588 children between the ages of 7 and 18 years, atomoxetine showed dose-related improvement in ADHD rating scales. Side effects of atomoxetine are similar to stimulants and include mild but significant increases in blood pressure and pulse. (7)
A meta-analysis of 11 non-randomized trials using clonidine for ADHD showed a smaller effect size compared with stimulants. (8) One RCT of 136 children with ADHD and tics showed improvement of both problems with the use of methylphenidate and clonidine, particularly in combination. (9) Second-line medications such as clonidine, pemoline (Cylert), and tricyclic anti-depressants have more potential serious side effects and are not well studied. (10)
* RECOMMENDATIONS FROM OTHERS
The American Academy of Pediatrics recommends that clinicians: 1) manage ADHD as a chronic illness, 2) collaborate with parents, the child, and school personnel to define specific desired outcomes, 3) use stimulant or behavioral therapy to improve these outcomes; if one stimulant is not effective at the highest feasible dose, try another, 4) reevaluate the diagnosis, treatment options, adherence, and possible coexisting conditions if treatment is not achieving the desired outcomes, and 5) follow-up regularly with parents, child, and teachers to monitor for progress and adverse effects. (11)
* CLINICAL COMMENTARY
When patients, parents, and teachers are educated, we achieve better outcomes
Stimulants and atomoxetine improve symptoms of ADHD quite effectively, making office treatment of ADHD a gratifying experience. Like many other diagnoses, there are numerous medications available to treat ADHD. Becoming familiar with a few and regularly prescribing them makes the treatment of ADHD more comfortable for the physician.
Sometimes patients and parents are hesitant to take medication for ADHD. Education about ADHD, along with trials of behavioral therapy, often improves patient satisfaction and compliance with medication. Likewise, children and adolescents may resist medication because of stigma or feeling unfairly labeled with a disease. Because of this, it is helpful to choose a medication with a long duration, so school dosing can be avoided. Artful negotiation with the patient and parent is beneficial.
In my experience, when patients, parents, and teachers are well-educated about ADHD and use behavioral therapy along with medication, we achieve better outcomes. Useful information for physicians and parents regarding medication use and behavioral therapy are described in the American Academy of Pediatrics ADHD Toolkit available at www.nichq.org/resources/toolkit.
Jerry Friemoth, MD, University of Cincinnati
REFERENCES
(1.) Conners CK. Forty years of methylphenidate treatment in Attention-Deficit/Hyperactivity Disorder. J Atten Disord 2002; 6 Suppl 1: S17-S30.
(2.) Connor DF, Fletcher KE, Swanson JM. A meta-analysis of clonidine for symptoms of attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 1999; 38:1551-1559.
(3.) Klassen A, Miller A, Raina P, Lee SK, Olsen, L. Attention-deficit hyperactivity disorder in children and youth: a quantitative systematic review of the efficacy of different management strategies. Can J Psychiatry 1999; 44:1007-1016.
(4.) A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. The MTA Cooperative Group. Multimodal Treatment Study of Children with ADHD. Arch Gen Psychiatry 1999; 56:1073-1086.
(5.) Smith BH, Waschbusch DA, Willoughby MT, Evans S. The efficacy, safety and practicality of treatments for adolescents with attention-deficit/hyperactivity disorder (ADHD). Clin Child Fam Psychol Rev 2000; 3:243-267.
(6.) Treatment of Attention-Deficit/Hyperactivity Disorder. Summary, Evidence Report/Technology Assessment: Number 11, AHCPR Publication No. 99-E017. Rockville, Md: Agency for Health Care Policy and Research; 1999. Available at: www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=hstat1. chapter.14677. Accessed on January 8, 2005.
(7.) Michelson D, Faries D, Wernicke J, et al. Atomoxetine in the treatment of children and adolescents with ADHD. Pediatrics 2001; 108:E83.
(8.) Kavale K. The efficacy of stimulant drug treatment for hyperactivity: a meta-analysis. J Learn Disabil 1982; 15:280-289.
(9.) Tourette's Syndrome Study Group. Treatment of ADHD in children with tics: a randomized controlled trial. Neurology 2002; 58:527-536.
(10.) Spencer TJ, Biederman J, Wilens TE, Faraone SV. Novel treatments for attention-deficit/hyperactivity disorder in children. J Clin Psychiatry 2002; 63 Suppl 12:16-22.
(11.) Clinical Practice Guideline: treatment of the school-aged child with attention deficit/hyperactivity disorder. Pediatrics 2001; 108:1033-1044. Available at: www.aap.org/policy/s0120.html. Accessed on January 8, 2005.
Lisa A. Johnson, MD, Providence St. Peter Hospital Family Practice Residency, Olympia, Wash; Sarah Safranek, MLIS, University of Washington Health Sciences Library, Seattle
COPYRIGHT 2005 Dowden Health Media, Inc.
COPYRIGHT 2005 Gale Group