Vaginal estrogen ring use is expanding for women. Physicians who know the indications for prescribing estrogen therapy and understand the risks and benefit can prescribe estrogen regardless of their specialty. Different estrogen rings perform different tasks (table 1). For example, one vaginal ring, Estring, is indicated exclusively for genitourinary atrophy (GU), while a new one, FemRing, is FDA approved for GU treatment and menopausal symptomatology.
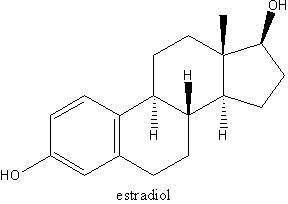
For some time, the Estring vaginal ring, a Silicone ring that releases 2 mcg/d of estradiol for three months, has been indicated for treatment of local GU atrophy in women with or without a uterus. Estring is only indicated for local GU treatment and has not been shown to treat menopausal symptoms. Symptoms of urogenital atrophy include: frank atrophic vaginitis with thin vaginal tissue and loss of vaginal rugae and elevated vaginal pH. (1) Atrophic vulvitis can manifest as kraurosis vulvitis with pruritus. Atrophic urethritis and trigonitis can predispose to urinary tract infection, as well as exacerbation of an overactive bladder. There are no large randomized, controlled trials (RCTs) that have looked at cancer outcomes with the Estring vaginal ring; however, there have RCTs examining estrogen blood levels and endometrial thickness that have not found any significant endometrial effects.
The Femring, which has been available in the United Kingdom for the last few years, is now FDA-approved for use in women with a hysterectomy who desire both local and systemic estrogen therapy delivered via a vaginal ring. Femring is a silastic ring with estradiol used every three months; it is for both vaginal and systemic estrogen therapy. It is indicated for treatment of menopausal symptomatology as well as GU atrophy. Each Femring delivers 50 mcg/d estradiol for three months from a drug reservoir containing 12.4 mg of estradiol acetate (approximately equivalent to systemic estradiol patches of 0.05). It is not approved to prevent or manage osteoporosis like other oral and transdermal estrogen therapies; however, ultralow doses of parental estradiol have been shown to positively affect bone. (1, 2) If adequate estradiol levels and adequate calcium and vitamin D intake are maintained, very low dose oral estrogen has been shown to have salutary effects on bone in older women (table 2). (3)
The Femring was initially approved for women who do not have a uterus for both local and systemic estrogen effect. In women with a uterus, if Femring is used, there is systemic estrogen effect and consequently endometrial stimulation. Therefore, if a woman has a uterus and is using Femring, progestin/progesterone therapy (either low-dose daily or cyclic monthly progestin) is indicated to prevent endometrial hyperplasia. (4,5)
These postmenopausal rings are in contrast to the NuvaRing (containing ethinyl estradiol and etonogestrel), which was the first contraceptive vaginal ring for premenopausal women. The NuvaRing is worn for three weeks and removed for one week during withdrawal menses. Currently there is no estroge- progestin postmenopausal hormone therapy vaginal ring.
Most women can insert and remove vaginal rings without difficulty in either the standing or supine position. The exact position of the vaginal ring is not critical as long as it is placed in the upper one-third of the vagina. Women who have not been sexually active for several years and/or have severe vaginismus and/or introital stenosis would not be candidates for this treatment. However, if these conditions are present in an older woman, local vaginal cream with finger application followed by progressive vaginal dilator use could be tried, followed by vaginal ring use.
As with all vaginal ring use, the woman needs to be instructed to remember to remove the ring and reinsert a new ring. If for some reason the ring falls out or is removed prior to the three-month interval, it can be washed with warm water and reinserted. The external diameter of the ring is 56 mm, which for the majority of postmenopausal women is small enough to be comfortable and yet not too small to fall out of the vagina.
There is no reason to think that the Femring would be any safer then either oral estrogen or transdermal estrogen in that the systemic estrogen effect and the risk for serious adverse consequences, including deep vein thrombosis, would be anticipated to be the same. The FDA has required the same risk labeling on all estrogen products. However, recently a study comparing oral and transdermal estrogen replacement therapy suggested less venous thromboembolism (VTE) with transdermal estrogen. (4) This data suggests, but does not confirm, that transdermal estrogen may be safer than oral estrogen with respect to thrombotic risk. Furthermore, there have been no comparative studies of vaginal estrogen systemic rings versus transdermal estrogen versus oral estrogens in terms of VTE risk. (5) However, the vaginal ring does bypass enterohepatic circulation and in some women, such as those with hypertriglyceridemia, Femring may offer an advantage over oral dosing.
An advantage with this ring is that symptomatic menopausal women who have had a hysterectomy and have adequate pelvic support, and desire both the systemic and local estrogen therapy would only have to think about treatment once a season (every three months). Other dosing regimens not available yet, such as a lower dose of estradiol (releasing 25 mcg/day of estradiol for three months) would be convenient for older women who ingest adequate calcium and vitamin D.
In the future, it would be convenient to have vaginal rings with progestin available (for women who need the progestin opposition for uterine protection), and androgen vaginal rings for women with female androgen deficiency syndrome. Indications for estrogen therapy and the individual risk-benefit equation for hormone use in any woman needs to be reassessed at least annually. (6, 7) The estrogen (Premarin 0.625 mg) arm of the WHI was recently released and shows no increase risk of breast cancer in women who have had a hysterectomy (and don't require progestin opposition.) (8)
References
(1.) Messinger-Rapport BJ, Thacker HL. Prevention for the older woman. A practical guide hormone replacement therapy and urogynecologic health. Geriatrics 2001;56(9):32-42.
(2.) Messinger-Rapport BJ and Thacker HL. Prevention for the older woman. A practical guide to prevention and treatment of osteoporosis." Geriatrics 2002; 57(4):16-8, 21-4, 27.
(3.) Prestwood KM, Kenny AM, Kleppinger A, Kulldorff M. Ultralow-dose micronized 17beta-estradiol and bone density and bone metabolism in older women: a randomized controlled trial. JAMA 2003; 290(8):1042-8.
(4.) Scarabin PY, Oger E, Plu-Bureau G; EStrogen and THromboEmbolism Risk Study Group. Differential association of oral and transdermal estrogen replacement therapy with venous thromboembolism risk. Lancet 2003; 362(9382):428-32.
(5.) Budev MM and Thacker HL. Exogenous female hormone administration and venous thrombosis. Dec. 10, 2003. http://www.clevelandclinicmeded.com/ diseasemanagement/women/exogenous/exogenous.htm. Accessed April 8, 2004.
(6.) Elder J and Thacker HL. Women's Health: Menopause. Cleveland Clinic Foundation Electronic Textbook of Medicine. http://www.clevelandclinicmeded.com/diseasemanagement/women/menopause/ menopause.htm. Accessed April 8, 2004.
(7.) North American Menopause Society. Estrogen and progestogen use in peri- and postmenopausal women: September 2003 position statement of The North American Menopause Society. Menopause 2003; 10(6):497-506.
(8.) Anderson GL, Limacher M, Assaf AR, et al; Women's Health Initiative Steering Committee. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy. The Women's Health Initiative randomized controlled trial. JAMA 2004; 291(14):1701-12.
Dr. Thacker is assistant professor of internal medicine, Ohio State University School of Medicine, Columbus, and clinical associate professor of medicine, Penn State College of Medicine, Hershey, PA. She is also section head of women's health and staff physician, departments of general internal medicine and obstetrics and gynecology, The Cleveland Clinic Foundation, Cleveland, Ohio. Disclosure: Dr. Thacker discloses that she serves on the speakers' bureaus of the Pfizer, Wyeth-Ayerst, Eli Lilly, and Merck corporations.
COPYRIGHT 2004 Advanstar Communications, Inc.
COPYRIGHT 2004 Gale Group