Abstract
The authors describe a prospective pilot study designed to investigate the use of topical nasal antifungal spray in addition to systemic steroids and itraconazole in the treatment of allergic fungal sinusitis. Sixteen patients with a history of allergic fungal sinusitis were given fluconazole nasal spray and followed for 3 months. Stabilization or improvement of disease without significant side effects was observed in 12 of the 16 patients who were treated with this protocol. These results indicate that topical fluconazole application may help patients with allergic fungal sinusitis; however; a larger multicenter study with longer patient follow-up is required to validate these initial findings.
Introduction
Allergic fungal sinusitis (AFS) is a form of chronic sinusitis characterized by nasal obstruction, sinus pain, rhinorrhea, and frequent orbital symptoms. Computed tomography (CT) frequently shows unilateral involvement with areas of hyperdensity in the affected sinuses, Histologically, fungal hyphae are not seen in all patients, and there is usually evidence of bony erosion of the sinus walls. Extensive eosinophilic infiltrate may be seen with major basic protein (MBP) in the mucosal site of disease. Conventional treatment consists of sinus surgery with extirpation of the allergic mucus, followed by postoperative ventilation of the sinuses and the use of systemic steroids. Frequent saline nasal irrigation has been used to clear the nasal and sinus cavity. Despite all of these interventions, AFS has a high rate of recurrence.
Fungal sinusitis presents in five major forms, each of which requires a different approach to treatment and has a different prognosis based on the extent of disease. Acute fulminant invasive fungal sinusitis is commonly seen in an immunocompromised host. This disease is clinically aggressive, destroying tissue and bone. Histopathologically, the fungus is angioinvasive and causes widespread necrosis. Treatment is aggressive surgical debridement and the use of antifungal drugs. If the underlying immunocompromised state is not corrected, the prognosis is significantly worse. (1-3)
Chronic invasive fungal sinusitis occurs mainly in diabetic patients, causing a chronic low-grade inflammatory reaction, as well as tissue necrosis. Aggressive surgical debridement and antifungal drugs are again the treatments of choice. However, this disease commonly recurs and has a poor prognosis. (1-3)
Granulomatous invasive fungal sinusitis occurs in an immunocompetent host and is usually unilateral. The organism is invasive but limited to the superficial mucosa and well contained within surrounding granulomas. Surgery followed by antifungal drugs is usually the treatment of choice, and the prognosis is satisfactory in most patients. (1-3)
Fungal ball or sinus mycetoma occurs in a unilateral sinus in an immunocompetent host. Histologically, there is no evidence of tissue invasion or granulomatous inflammation. Surgical removal is the treatment of choice, and patients usually have an uneventful recovery. (1-3)
AFS was first described by Millar et al in 1981, when they reported 5 patients with significant Type I hypersensitivity to Aspergillus and sinus pathology similar to pulmonary findings in patients with allergic bronchopulmonary aspergillosis (ABPA). (4) These patients present with asthma, increased total scrum immunoglobulin E (IgE), pulmonary eosinophilia, specific allergic immune response, and thick, tenacious mucus that causes bronchial obstruction and bronchiectasis. In 1983, Katzenstein et al reviewed 113 consecutive histopathologic specimens from chronic sinusitis surgeries and identified 7 cases of allergic aspergillus sinusitis. (5) They described this a s allergic mucin, which consisted of degenerating eosinophils, desquamated respiratory epithelial cells, and Charcot-Leyden crystals. Fungal stains revealed fungal hyphae but no evidence of tissue invasion. Subsequent case reports described identical findings with other fungi, and the disease was termed allergic fungal sinusitis. (3)
The five major criteria for AFS are evidence of IgE-mediated hypersensitivity, nasal polyposis, characteristic CT findings, eosinophilic mucus, and positive fungal smear or culture. The minor criteria include asthma, unilateral predominance, radiographic bone erosion, fungal culture, Charcot-Leyden crystals, and serum eosinophilia. (1,2,6) Treatment consists of surgery followed by postoperative oral corticosteroids. (7) Conventional treatment consists of ethmoidectomy and middle meatal antrostomy with removal of the allergic mucus followed by postoperative oral corticosteroids. Systemic antifungals have not proved consistently beneficial because the fungi are noninvasive. (8,9)
The goal of this study was to evaluate the role of a topical antifungal spray in the treatment of AFS.
Material and methods
This prospective study was based at a tertiary teaching hospital. Using an open enrollment, patients with a history of AFS were selected because of progression of symptoms during treatment. Participants were advised of the non-FDA-approved use of an FDA-approved drug and given the option to withdraw from the study.
Sixteen patients with a history of AFS were given fluconazole nasal spray and followed for 3 months (table). Of the 16 patients who participated in the study, 8 were men and 8 were women. Their ages ranged from 39 to 74 years. Previous treatment included systemic itraconazole alone in 5 patients and systemic itraconazole and oral prednisone in 8 patients. Three patients did not have any previous treatment.
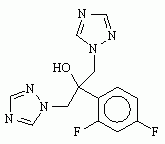
The fluconazole used in the study was formulated by SinuCare, Inc. (Altamonte Springs, Fla.). It consisted of 100 mg of fluconazole in 500 ml of normal saline solution administered as 5 sprays (0.5 cc/spray) in each nostril twice daily.
Patients were followed monthly with nasal endoscopy, and their response to treatment was assessed through the serial nasal endoscopic examinations comparing the presence of polyps and mucosal edema. The patients' symptoms and their perception of response to treatment also were recorded.
Results
Twelve of the 16 patients (75%) had stable disease or a decrease in mucosal edema during treatment with the antifungal nasal spray; 4 patients (25%) had progression of the edema during treatment with the nasal spray.
Three patients (19%) had polyps prior to starting treatment; their polyps did not regress with treatment. Thirteen patients showed no evidence of polyps prior to starting treatment. Ten patients continued to be free of polyps during treatment; however, 3 patients developed polyps during treatment.
Subjectively, 12 patients (75%) perceived no worsening or improvement in their symptoms with treatment. The other 4 patients felt their symptoms were worse during treatment.
Three patients were treated with the nasal spray only. Two showed improvement or were stable; one did not respond to treatment.
Discussion
The initial treatment of AFS is surgical debulking of the affected sinuses an d removal of allergic mucin and reactive hypertrophied or hyperplastic mucosa. Both the fungus and the diseased mucosa are removed, and the obstructed sinuses are reventilated. (7,10) Waxman et al suggested the use of systemic corticosteroids postoperatively, based on the treatment modalities used in ABPA. (11) They looked at 26 patients, 10 of whom received postoperative steroids, and noticed that the patients given steroids had less disease on follow-up endoscopic examination. Kuhn and Javer followed 11 patients with AFS who were given systemic steroids postoperatively and noticed a significant decrease in mucosal discase. (9) Incomplete surgical removal of the pathologic tissue usually renders the patient susceptible to relapse of the disease). (3,7,12)
Antifungal drugs given systemically have not proved effective for treatment of AF S, primarily because the drugs are not secreted into the nasal secretion. The fungus is not invasive; and because the drugs are not secreted into the mucus, fungicidal levels are not achieved in the mucous lining of the nasal cavity and the paranasal sinuses. (3,8,9) In this study, topical antifungals were studied as the only intervention or in combination with systemic and fungals and systemic steroids. In AFS, tissue damage is not caused by invasive fungus but rather by the immunologic hyperreaction associated with the presence of a fungal antigen in an atopic individual. (2,3,12-14) Application of topical antifungals should achieve fungicidal concentrations in the nasal and paranasal sinus mucosa, eradicating the fungus and thus reducing fungal antigen load.
Most of the patients in this study had stable symptoms with application of the topical antifungal spray. We interpreted this as success of the antifungal spray, because the majority of patients in this treatment regimen had no progression of the disease. However, relapses in AFS have been shown to occur as much as 2 years after treatment.
This study followed 16 patients for only 3 months. The next step would be to add a placebo group, utilize a standard quality-of-life questionnaire, and follow the patients longer.
Conclusion
AFS is a difficult disease to treat, because patients often experience multiple relapses. The mainstay of treatment is surgical debridement followed by systemic steroids. Systemic antifungals have not proved effective; however, based on the preliminary findings in this study, there may be a role for topical antifungals. Further investigation is warranted.
References
(1). Bent JP III, Kuhn FA. Diagnosis of allergic fungal sinusitis. Otolaryngol Head Neck Surg 1994;111:580-8.
(2.) deShazo RD, Chapin K, Swain RE. Fungal sinusitis. N Engl J Med 1997;337:254-9.
(3.) Schubert MS. Medical treatment of allergic fungal sinusitis. Ann Allergy Asthma Immunol 2000;85:90-7.
(4.) Millar JW, Johnston A, Lamb D. Allergic aspergillosis of the maxillary sinuses [abstract]. Thorax 1981;36:710.
(5.) Katzenstein AA, Sale SR, Greenberger PA. Allergic Aspergillus sinusitis: A newly recognized form of sinusitis. J Allergy Clin Immunol 1983;72:89-93.
(6.) deShazo RD, Swain RE. Diagnostic criteria for allergic fungal sinusitis. J Allergy Clin Immunol 1995;96:24-35.
(7.) Marple BF. Allergic fungal rhinosinusitis: Surgical management. Otolaryngol Clin North Am 2000;33:409-19.
(8.) Bent JP III, Kuhn FA. Antifungal activity against allergic fungal sinusitis organisms. Laryngoscope 1996;106:1331-4.
(9.) Kuhn FA, Javer AR. Allergic fungal rhinosinusitis: Perioperative management, prevention of recurrence, and role of steroids and antifungal agents. Otolaryngol Clin North Am 2000;33:419-33.
(10.) Marple BF, Mabry RL. Comprehensive management of allergic fungal sinusitis. Am J Rhino11998;12:263-8.
(11). Waxman JE, Spector JG, Sale SR, Katzenstein AA. Allergic Aspergillus sinusitis: Concepts in diagnosis and treatment of a new clinical entity. Laryngoscope 1987;97:261-6.
(12.) Schubert MS, Goetz DW. Evaluation and treatment of allergic fungal sinusitis. II. Treatment and follow-up. J Allergy Clin Immunol 1998; 102:395-402.
(13.) Ence BK, Gourley DS, Jorgensen NL, et al. Allergic fungal sinusitis. Am J Rhinol 1990;4:169-78.
(14.) Kinsella JB, Bradfield J J, Gourley WK, et al. Allergic fungal sinusitis. Clin Otolaryngol 1996;21:389-92.
From the Department of Otolaryngology, Head and Neck Surgery, New York Presbyterian Hospital of Columbia and Cornell University, New York.
Dr. Anand is a consultant for SinuCare, Inc., one of the pharmaaeies used to formulate the nasal spray used in this study, but has no financial interest in the company.
Reprint requests: Dr. Vijay Anand, MD, 205 E. 64th St., New York, NY 10021. Phone: (212) 832-3222; fax: (212) 832-3287; e-mail: Vijayanandmd@aol.com
Originally presented at the Combined Otolaryngology Spring Meeting of the American Rhinological Society, May 11, 2002, Boca Raton, Fla.
COPYRIGHT 2004 Medquest Communications, LLC
COPYRIGHT 2004 Gale Group