Study objectives: Patients with COPD are at risk of experiencing a deterioration in arterial oxygen saturation (Sa[O.sub.2]) during sleep, which is generally most pronounced during rapid eye movement (REM) sleep. Increased cholinergic tone has been suggested as a contributing factor to this decrease in Sa[O.sub.2]. Therefore, we investigated whether 4-week treatment with ipratropium bromide inhalation solution 0.02% (qid) could improve sleep characteristics in COPD.
Design: Randomized, placebo-controlled, double-blind, two-arm parallel study of 4 weeks of treatment with ipratropium bromide solution or placebo.
Setting: Multicenter investigation.
Patients: Thirty-six patients with moderate-to-severe COPD ([FEV.sub.1] < 65% of predicted).
Measurements and results: Evaluation included polysomnographic, pulmonary function, and subjective quality of sleep (visual analog scale [VAS]) assessments. It was found that 4 week of treatment with ipratropium bromide solution in patients with COPD led to the following: (1) a significant (p = 0.05) improvement in mean nocturnal Sa[O.sub.2] with the more severe the nocturnal desaturation, the greater the improvement in Sa[O.sub.2]; (2) significant (p = 0.03) improvement in perceived sleep quality (VAS: 5.5 [+ or -] 0.5 after placebo; 7.2 [+ or -] 0.5 after ipratropium); (3) a significant (p = 0.05) increase in REM sleep time (48.6 [+ or -] 6.3 min after placebo; 66.5 [+ or -] 6.4 min after ipratropium) with no effect on other sleep stages or total sleep time; and (4) a significant (p = 0.01) increase in pre-sleep FVC and flow rate at 50% of the vital capacity.
Conclusions: These findings demonstrate that ipratropium bromide therapy can improve sleep Sa[O.sub.2] as well as sleep quality in patients with moderate-to-severe COPD. (CHEST 1999; 115:1338-1345)
Key words: COPD; ipratropium bromide; oxygen saturation; sleep
Abbreviations: ANCOVA = analysis of covariance; IB = ipratropium bromide; REM = rapid eye movement; Sa[O.sub.2] = arterial oxygen saturation; TST = total sleep time; VAS = visual analog scale
Disturbed sleep-related symptoms are common in patients with COPD. In the Tucson Epidemiological Study of Obstructive Airways Disease, 2,187 general population subjects (85% without and 15% with obstructive respiratory disease) were questioned about sleep characteristics. Forty-one percent of patients with obstructive respiratory disease had at least one symptom of disturbed sleep.[1] Matched for age, patients with the diagnosis of chronic bronchitis, chronic bronchitis plus asthma, or emphysema had a greater prevalence of disorders for initiating and maintaining sleep and excessive daytime sleepiness. Additionally, many studies have demonstrated that patients with stable COPD are at risk of developing decrements in arterial oxygen saturation (Sa[O.sub.2]) during sleep.[2-8] These decreases are usually more prominent during rapid eye movement (REM) sleep.[2-5] However, the relationship between Sa[O.sub.2] levels during sleep and sleep disturbances is unclear with conflicting results in the literature.[2-5,8]
Cholinergic tone has a normal circadian rhythm with higher levels during the sleep-related hours.[9,10] In patients with COPD, this may be an important contributing factor to nocturnal oxygen desaturation and disrupted sleep characteristics.
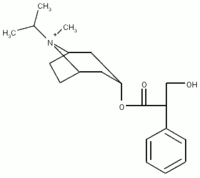
Ipratropium bromide (IB) (Atrovent; Boehringer Ingelheim Pharmaceuticals Inc; Ridgfield, CT) is an anticholinergic agent with well-established bronchodilation properties in patients with COPD.[11] Daytime study has demonstrated that long-term therapy with ipratropium improves baseline pulmonary function and also results in improvement in airway response to acute bronchodilation.[11] However, the effect of ipratropium on sleep quality in COPD patients is not known. Thus, in this study, we evaluated the effect of an anticholinergic medication, IB inhalation solution, over a 4-week period in COPD patients, to determine its effect on sleep stages, perception of sleep quality, nocturnal oxygen saturation, and lung function.
MATERIALS AND METHODS
Subjects
Seventy-five patients with COPD were screened to enroll 36 patients into the study from four centers that met all study criteria. The baseline demographic and respiratory characteristics are summarized in Table 1. The diagnosis of COPD followed the American Thoracic Society definition. [12] This study included both male and female patients between the ages of 40 and 75 years with a history of [is greater than] 10 pack-years of smoking. The [FEV.sub.1] needed to be [is less than] 65% of predicted and relative stability of symptoms was required. Patients were excluded if significant (as determined by an investigator) nonpuhnonary or pulmonary disease other than COPD was present. Specific exclusions were elevated liver or renal function laboratory values greater than two times normal values, a myocardial infarction within 6 months, sleep apnea syndrome (apnea index [is greater than] 10), any respiratory viral infections within 6 weeks of study, and symptomatic prostatic hypertrophy or bladder neck obstruction. Excluded medications included [Beta]-blockers, oral or topical steroids, tricyclic antidepressants, antihistamines, and long-term oxygen therapy. Patients could take a constant twice-daily theophylline preparation (one subject in the placebo group, Table 1). Theophylline treatment was withheld on each test day. Fixed scheduled albuterol was allowed and kept at a constant dosage throughout the study (Table 1). All patients signed Institution Review Board-approved protocol consent forms.
(*) DLCO = diffusion capacity of the lung for carbon monoxide; % pred = percent predicted.
Study Design
The study was a 4-week randomized, double-blind, placebo-controlled, two-arm parallel group design. Following an initial 3-week screening process, patients were randomized into a 4-week treatment phase using IB solution (500 [Micro]g) or placebo (matched to IB in color and taste) via a nebulizer (DeVilbiss 646; Somerset, PA) four times daily. Treatment assignments were made independently in each center using computer-generated random sequences. Treatments were identical in appearance. All clinical personnel, subjects, and employees of the sponsor remained blinded throughout the conduct of the trial.
Polysomnographic evaluations were performed four times during the study. The polysomnographic technique and scoring were standardized between centers with the American Sleep Disorders Association practice parameters[13] and standard scoring.[14] The first evaluation occurred at day 7 of the screening interval and was done for acclimatization. The baseline evaluation occurred at day 14 of the screening process. One week later, the third evaluation occurred following the first dose of IB or placebo and the fourth evaluation occurred at the end of 4 weeks of therapy. Presleep and postsleep pretreatment spirometry values were determined at the baseline visit, after first dose, and after 4 weeks of treatment. A visual analog scale (VAS) used to evaluate subjective sleep characteristics and breathlessness[15] was done after 1 week of the screening period and at study termination.
Treatment
Treatment consisted of oral inhalation from a compressor-driven nebulizer (De Vilbiss 646) administered in accordance with instructions provided by the manufacturer. Treatment was delivered qid for a period of 4 weeks. IB was delivered as a 0.02% inhalation solution (500 [micro]g) in a volume of 0.3 mL. Each dose consisted of 0.3 mL ipratropium solution in 2.0 mL of normal saline solution and was delivered by a compressor-driven nebulizer (De Vilbiss 646) (driving pressure equal to 30 to 45 psi) to the patient for 15 min or until the volume was completely consumed. The placebo solution was 2.3 mL of normal saline solution. At each weekly clinic visit, a new supply of randomized medication was given to each patient. All in-clinic dosing was done under the supervision of laboratory personnel. The compliance of patients with the study therapy was confirmed by the determination of IB in the samples from 24-h urine collection at the last clinic visit.
Statistics
All comparisons between groups (sleep stages, nocturnal oxygen saturation, spirometry, VAS, etc.) were performed using an analysis of covariance model (ANCOVA). The last value observed at a pretreatment visit (baseline) was taken as the covariate and the dependence of the follow-up observation on the baseline observation (slope) was allowed to vary between treatments. The rationale for this model is as follows. No enrollment restrictions were imposed on patients regarding baseline level of dysfunction in the efficacy end points. For example, patients were not required to demonstrate nocturnal oxygen desaturation at baseline. This yielded a diverse study population with differing potentials for response to therapy. Patients with little or no dysfunction at baseline had little potential for improvement, while patients with a large degree of dysfunction at baseline had a large potential for improvement. Since the scales for most of the efficacy measures were bounded, it was thought to be unrealistic to assume a uniform additive improvement across the entire spectrum of baseline dysfunction. An idealized response in such a situation would be to have the treated subjects in the dysfunctional group show maximal improvement while the placebo group show no change.
The workings of the ANCOVA analysis are best illustrated by a scattergram of the follow-up observations (vertical-axis) vs the baseline observations (horizontal-axis) for each patient (Figs 1 and 2). Best fit lines under the least squares criterion are fit to each treatment group. The vertical distance between the lines represents the improvement associated with treatment with IB at a given baseline value. The amount of improvement varies depending on the baseline value at which the comparison is made. For balance, the comparisons reported herein are made at the average baseline value observed over both treatment groups. The follow-up values in each group corresponding to the average baseline value (see arrows in Figs 1 and 2) are termed the least squares means adjusted for baseline. If comparisons of the regression lines were made for a more impaired baseline value, the difference in treatment groups would increase.
[Figures 1-2 ILLUSTRATION OMITTED]
As prespecified in the protocol, posttreatment visits for first dose and 4-week therapy were compared individually with the baseline visit to give an indication of persistence and onset of response. For the nocturnal oxygen saturation, the temporal trend across the follow-up visits was also evaluated in a post hoc fashion using a repeated measures ANCOVA model with baseline visit as the covariate.
Analyses were done using software (SAS version 6.12; SAS Institute, Inc; Cary, NC). Statistical significance is claimed at level 0.05 vs the two-sided alternative. Unless otherwise stated, statistics are given as least square mean adjusted for pretreatment baseline [+ or -] SE. Sample size was estimated based on a study of sleep architecture investigating the effects of protriptyline in a crossover design.[16] In that study, the change in the lowest nocturnal Sa[O.sub.2] observed in 14 patients was 7.1% [+ or -] 6.0% (mean [+ or -] SD). Our trial was originally planned for 25 patients per treatment group to achieve at least 90% power to detect a 7% difference based on a two-sample t test with an SD of 6%. The SD for the ANCOVA model was 5.6%. Thus, even though the original recruitment goal was not obtained, adequate power (94%) was maintained for the actual achieved sample size.
RESULTS
Patients' Demographics and Lung Function on Entry Into the Study
Thirty-six subjects were enrolled into the study. The baseline demographic and respiratory characteristics of these patients are shown in Table 1. One IB-treated patient withdrew secondary to headaches during the treatment phase. In addition, one placebo-treated patient with a concomitant diagnosis of depression suffered an adverse event described as depression of moderate intensity lasting 2 days during the treatment phase. Sleep data collection for this patient was not complete. These two patients were excluded from all analyses prior to unblinding the randomization code.
This was a group of 40- to 75-year-old patients who were diagnosed as having COPD. On entry into the clinical research unit, their [FEV.sub.1] values ranged from 0.51 to 2.91 L. All had a marked reduction in their diffusion capacity of carbon monoxide and their baseline arterial blood gas values showed mild hypoxemia and no retention of carbon dioxide.
Table 1 also demonstrates that there were no statistical differences in patient characteristics between the placebo- and IB-treated groups except for current smokers (p = 0.02).
Sleep Characteristics
As Figure 3 shows, there was no significant effect with regard to time spent in various sleep stages after the first dose of IB; however, there is a trend toward greater time in REM and total sleep time (TST) with IB treatment. This trend is significant with regard to REM sleep after 4 weeks of treatment (66.5 [+ or -] 6.4 min for the IB group vs 48.6 [+ or -] 6.3 min for patients who were receiving placebo, p = 0.05). The TST was increased after treatment with IB but this increase did not reach statistical significance.
[Figure 3 ILLUSTRATION OMITTED]
The awakenings per hour of sleep time for placebo and IB after the first dose were 2.2 [+ or -] 0.4 and 2.8 [+ or -] 0.4, respectively (p = 0.32), and for arousals per hour, the values were 17.6 [+ or -] 1.8 and 14.4 ? 1.8, respectively (p = 0.22). At 4 weeks, there was a trend toward fewer awakenings per hour in the IB-treated group, 1.9 [+ or -] 0.4 vs 3.0 [+ or -] 0.4 for placebo (p = 0.08). The arousals per hour decreased in the IB-treated group, but they were not significantly different from the group receiving placebo, 12.7 [+ or -] 3.2 vs 18.8 [+ or -] 3.2, respectively (p = 0.19).
Figure 4 summarizes mean latency to various sleep stages after the first dose of therapy and after 4 weeks of therapy. After the first dose of therapy, there was a trend toward shortened latency to the sleep stages in favor of IB in comparison to placebo. This trend achieved statistical significance for the latency to stage 2 and the latency to persistent sleep. These trends were not seen after 4 weeks of therapy.
[Figure 4 ILLUSTRATION OMITTED]
Figure 1 shows the effect of therapy on the subjective VAS evaluation of sleep as assessed by the question "How well did you sleep last night?" This question was directed toward the night prior to evaluation in the sleep laboratory, that is, toward the patient's normal sleep pattern while at home. It can be seen that the perception of sleep after 4 weeks of therapy was significantly improved in patients receiving IB (7.2 [+ or -] 0.5 vs 5.5 [+ or -] 0.5, p = 0.03). It should be emphasized that the sleep quality was most improved in those patients who had poor sleep quality at baseline prior to therapy. In the placebo group, the perceived sleep quality was unaltered over the range of perceptions at baseline.
Daytime perception of breathlessness tended to reflect the nighttime perception of sleep quality. The placebo group tended to have more breathlessness at 4.0 [+ or -] 0.5 out of 10; while after IB, breathlessness was at 2.7 [+ or -] 0.5 as evaluated by the VAS (p = 0.07).
Nocturnal Sa[O.sub.2] was significantly improved with the first dose of IB and after 4 weeks of treatment (Table 2). Treatment groups had comparable presleep Sa[O.sub.2] values. Significant differences in favor of IB were seen in the posttreatment mean nightly Sa[O.sub.2] and lowest mean hourly Sa[O.sub.2]. The largest differences were observed in patients with the lowest nocturnal Sa[O.sub.2] at baseline. Analysis of the data in terms of patient's individual changes from presleep values yielded confirmatory results. The relationship of the lowest nocturnal Sa[O.sub.2] after the first dose and after 4 weeks of therapy to the baseline visit values is summarized in Figure 2. The placebo group lies along a 45 [degrees] slope of no change while the IB group shows increased saturation posttherapy. Repeated measures analysis of the temporal trends between the two after treatment evaluation showed higher overall significance for the average of the responses after one dose and after 4 weeks of therapy than is reported for the individual time points in Table 2; however, no significant difference was seen between the after-treatment time points as measured by the interaction of treatment and time.
(*) Baseline values are reported as means [+ or -] SEM; treatment values as least square means adjusted for baseline [+ or -] SEM.
Since the randomization of subjects produced unequal smoking histories (Table 1), reanalysis of the data was performed to take into account this factor. The results of the reanalysis were consistent with the original outcome.
Evaluation of Pulmonary Function
After 4 weeks of treatment with IB, there was an increase in predose, presleep spirometry indexes, achieving statistically significant improvement for FVC (p = 0.01) and flow rate at 50% of the vital capacity (p = 0.01), compared with placebo (Table 3). There were no significant differences in any of the morning-after, predose spirometry indexes.
(*) Baseline values are reported as means [+ or -] SEM. Treatment values as least square means adjusted for baseline [+ or -] SEM. p values are based on two-sided comparison between treatment groups at the specified time point. [FEF.sub.25-75%] = forced expiratory flow between 25% and 75% of the vital capacity; [Vmax.sub.50%] = flow rate at 50% of the vital capacity.
Compliance
To evaluate patient compliance with medication, urine samples were analyzed for the presence and quantity of IB. Based on the 24-h urine samples obtained at the last clinic visit, 85% of the patients in this study were compliant with regard to taking their study medication.
Adverse Events
All adverse events that occurred during the course of the trial were collected and documented. As can be seen in Table 4, the number and distribution of adverse events were similar for both groups. One subject in the IB group developed a persistent headache and stopped the study due to this event. Most adverse events were mild in nature and of short duration.
DISCUSSION
The quality of sleep in many patients with COPD is significantly compromised. As indicated by objective measures such as reduced sleep time, increased sleep stage shifts, and increased arousal frequency, patients with COPD generally sleep poorly. These patients also complain of difficulty with sleep onset and sleep maintenance.[2-4,8] Several studies detected that these patients have a significant and frequent decrease in nocturnal Sa[O.sub.2].[2-8] According to some studies, the most marked reduction in Sa[O.sub.2] occurs during REM sleep.[2-5] Postma and associates[10] reported that an imbalance in the autonomic nervous system is the underlying cause for nocturnal dyspnea and sleep disturbance in patients with chronic airflow obstruction. Thus, long-term therapy with anticholinergic agents, such as IB, may have an effect on sleep quality and objective indexes of sleep architecture.
In this study, we have demonstrated that nebulized IB solution given qid in patients with well-defined, moderate-to-severe COPD resulted in a significant improvement in nocturnal Sa[O.sub.2] as measured during sleep and significant improvement in the perception of sleep quality as assessed by a VAS. In addition, we found that this treatment increased
REM sleep as compared with the placebo group. This was associated with a trend toward fewer awakenings per hour of sleep.
The relationship between nocturnal hypoxemia and altered sleep architecture is not clear. Brezinova and colleagues[3] demonstrated in COPD patients described as "blue and bloated" that brief arousals ([is less than] 1 min in duration) occurred at a rate of 10/h compared with 6/h in a matched control group (p [is less than] 0.05). However, only 8% of these episodes were related to oxygen desaturation or apnea. The increased number of arousals appeared to affect sleep characteristics as they were correlated to low percentages of stages 3 and 4 sleep. Although Fleetham et al[4] did show that arousals were strongly associated with oxygen desaturation in COPD subjects, on subsequent nights, blocking desaturation with supplemental oxygen did not alter the arousal index or sleep quality. Finally, in "blue and bloated" COPD patients, Calverley et al[2] showed that hypoxemia was not related to any sleep variable examined, yet when these individuals slept with supplemental oxygen, the amount of sleep stages 2 to 4 and REM increased. Whether differentiating COPD patients with regard to a characteristic type ("blue and bloated" indicated greater daytime hypoxemia and hypercapnea vs "pink puffer") plays a role in sleep characteristics needs to be better determined. Our study had both COPD "types" enrolled as we were evaluating the effects of IB in a general COPD population. Overall, daytime Pa[O.sub.2] was slightly reduced, but the Pa[CO.sub.2] levels were normal. We did not find that the degree of desaturation was correlated to arousals or sleep stages. Thus, the improved sleep Sa[O.sub.2] with IB may not be the answer for improvement in REM sleep.
To our knowledge, this is the first study to demonstrate improvement in both nocturnal arterial Sa[O.sub.2] and sleep quality in patients with COPD. Previous studies on the effect of oxygen therapy have shown improvement in nocturnal arterial saturation but no changes in sleep quality.[4,17,18] Similarly, there are several studies of the effect of oral theophylline on sleep that have suggested improvements in nocturnal Sa[O.sub.2] but no benefit in sleep quality.[19-21] There are limited data on the effect of [Beta]-agonists on sleep quality in patients with COPD. One study[22] suggested no changes in sleep quality or nocturnal arterial oxygenation with oral salbutamol in patients with moderate COPD.
Although the morning lung function was not significantly improved in our study, this does not rule out improved overnight airway function. That marked improvement in overall control of COPD is not reflected in spirometry has been shown using theophylline. Chrystyn and colleagues[23] showed a large reduction in trapped gas volume with patients receiving theophylline accounting for the improved clinical picture that was not reflected in spirometric measurements. Thus, IB therapy theoretically could have been having a similar type of effect, thereby improving nocturnal Sa[O.sub.2], REM sleep, and being reflected in the patients' daytime symptoms and sleep VAS responses. Another possibility is that the combination of IB and a [[Beta]sub.2]-agonist produced the beneficial effects seen in this study, since 16 of the IB group subjects were also on a fixed schedule of albuterol. This study was not designed to test this effect.
It is of interest that those patients in our study with the greatest oxygen desaturation during sleep on the baseline night had the most improvement in this variable using nebulized IB. This suggests that in this group of patients, the hypoxemia is at least in part related to increased cholinergic tone that is then blocked by IB. If selection of patients into this study had been based on the presence of oxygen desaturation during sleep, it is likely that Sa[O.sub.2] would have been even more significant. The duration of effect for the nebulized form of IB is approximately 4 to 6 h with regard to the daytime effect on [FEV.sub.1].[24] Whether the pharmacokinetics and pharmacodynamics of IB are altered at night is unknown.
The fact that IB therapy improved nocturnal Sa[O.sub.2] in patients with COPD may have important functional consequences. Improved Sa[O.sub.2] could result in a decreased incidence of cardiac arrhythmias[25] and in improvement of pulmonary hypertension and polycythemia.[5] These issues will require further investigation.
Protriptyline, a tricyclic antidepressant, has been shown to significantly improve nocturnal Sa[O.sub.2] in patients with COPD.[16,26] A proposed mechanism of action for this improvement is the significant decrease in REM sleep observed after treatment with protriptyline. Interestingly, IB is associated with increased nocturnal Sa[O.sub.2] in the presence of greater amounts of REM sleep.
From the available evidence, it would seem that the effect of various types of medications on sleep in COPD patients depends on a balance between improved airway mechanics and potential adverse medication side effects, particularly those affecting CNS processes mediating sleep. These potentially negative effects on sleep are likely to be more clinically important in the older COPD patient (who is already more prone to sleep disturbances by virtue of his/her age) than in younger COPD patients. Thus, while [Beta]-agonists and methylxanthines may improve nocturnal Sa[O.sub.2] in COPD patients, the CNS stimulation often noted with both classes of drugs might explain why improvements in sleep quality have not been observed. Since IB has much less potential for crossing the blood-brain barrier, the beneficial effects on airway mechanics result in improvements in both nocturnal oxygenation and sleep quality.
In summary, we have shown that nebulized IB solution improves overnight Sa[O.sub.2], REM sleep, and, importantly, the patients' perception of sleep quality. Since poor sleep quality is a common feature in COPD patients and nocturnal oxygen desaturation can contribute to pulmonary hypertension, IB should be considered in the treatment program for these patients. As longer-acting anticholinergic medications are developed,[27] these agents need to be evaluated in COPD patients for better nocturnal disease control.
ACKNOWLEDGMENTS: The authors gratefully acknowledge the contributions of Dr. T. Roth (Detroit) and V. Mohsenin (New Haven) in the preparation of the protocol and to Stacey Wolff for the assistance in the preparation of the manuscript.
REFERENCES
[1] Klink M, Quan SF. Prevalence of reported sleep disturbances in a general adult population and their relationship to obstructive airways diseases. Chest 1987; 91:540-546
[2] Calverley PMA, Brezinova V, Douglas NJ, et al. The effect of oxygenation on sleep quality in chronic bronchitis and emphysema. Am Rev Respir Dis 1982; 126:206-210
[3] Brezinova V, Catterall JR, Douglas NJ, et al. Night sleep of patients with chronic ventilatory failure and age matched controls: number and duration of the EEG episodes of intervening wakefulness and drowsiness. Sleep 1982; 5:123-130
[4] Fleetham J, West P, Mezon B, et al. Sleep, arousals, and oxygen desaturation in chronic obstructive pulmonary disease. Am Rev Respir Dis 1982; 126:429-433
[5] Douglas NJ, Flenley DC. Breathing during sleep in patients with obstructive lung disease. Am Rev Respir Dis 1990; 141:1055-1070
[6] Kearley R, Wynne JW, Block AJ, et al. The effect of low flow oxygen on sleep-disordered breathing and oxygen desaturation. Chest 1980; 78:682-685
[7] Berry RB, Desa MM, Branum JP, et al. Effect of theophylline on sleep and sleep-disordered breathing in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis 1991; 143:245-250
[8] Cormick W, Olson LG, Hensley M J, et al. Nocturnal hypoxaemia and quality of sleep in patients with chronic obstructive lung disease. Thorax 1986; 41:846-854
[9] Baust W, Bohnert B. The regulation of heart rate during sleep. Exp Brain Rev 1969; 7:169-180
[10] Postma DS, Keyzer JJ, Koeter GH, et al. Influence of the parasympathetic and sympathetic nervous system on nocturnal bronchial obstruction. Clin Sci 1985; 69:251-258
[11] Rennard SI, Serby CW, Ghafouri M, et al. Extended therapy with ipratropium is associated with improved lung function in patients with COPD: a retrospective analysis of data from seven clinical studies. Chest 1996; 110:62-70
[12] American Thoracic Society. Standard for the diagnosis of patients with chronic obstructive pulmonary disease (COPD) and asthma. Am Rev Respir Dis 1987; 136:225-243
[13] American Sleep Disorders Association Polysomnogram Task Force. Practice parameters for the indications for polysomnography and related procedures. Sleep 1997; 20:406-422
[14] Rechtschaffen A, Kales A. Manual of standardized terminology, techniques and scoring system for sleep stage of human subjects. Washington, DC: Public Health Service, 1968
[15] Caroll N, Parker RA, Branthwaite MA. The use of protriptyline for respiratory failure in patients with chronic airflow limitation. Eur Respir J 1990; 3:746-751
[16] Series F, Cormier Y. Effect of protryptyline on diurnal and nocturnal oxygenation in patients with chronic obstructive pulmonary disease. Ann Intern Med 1990; 113:507-511
[17] McKeon JL, Murree-Allen K, Saunders N. Supplemental oxygen and quality of sleep in patients with chronic obstructive lung disease. Thorax 1989; 44:184-188
[18] Goldstein RS, Rachmaran V, Bowes G, et al. Effect of supplemental nocturnal oxygen on gas exchange in patients with severe obstructive airway disease. N Engl J Med 1984; 310:425-429
[19] Mulloy E, McNicholas WT. Theophylline improves gas exchange during rest, exercise and sleep in severe chronic obstructive puhnonary disease. Am Rev Respir Dis 1993; 148:1030-1036
[20] Man GCW, Chapman KR, Habib S, et al. Sleep quality and nocturnal respiratory function with once-daily theophylline (Uniphyl) and inhaled salbutamol in patients with COPD. Chest 1996; 110:648-653
[21] Bandner S, Salmi T. Nocturnal oxygen saturation and sleep quality in patients with advanced chronic obstructive puhnonary disease dunng treatment with moderate dose CR-theophylline. Eur J Clin Pharmacol 1992; 43:125-129
[22] Veale D, Cooper BG, Griffiths CJ, et al. The effect of controlled-release salbutamol on sleep and nocturnal oxygenation in patients with asthma and chronic obstructive pulmonary disease. Respir Med 1994; 88:121-124
[23] Chrystyn H, Mulley BA, Peake MD. Dose response relation to oral theophylline in severe chronic obstructive airways disease. BMJ 1988; 297:1506-1510
[24] Tashkin DP, Ashtosh K, Bleecker ER, et al. Comparison of the anticholinergic bronchodilator ipratropium bromide with metaproterenol in chronic obstructive pulmonary disease: a 90-day multi-center study. Am J Med 1986; 81(suppl 5A): 81-90
[25] Flick MR, Block AJ. Nocturnal vs diurnal cardiac arrhythmias in patients with chronic obstructive pulmonary disease. Chest 1979; 75:8-11
[26] Series F, Cormier Y, La Forge J. Changes in day and night time oxygenation with protriptyline in patients with chronic obstructive lung disease. Thorax 1989; 44:275-279
[27] Maesen FPV, Smeetes JJ, Sledens TJH, et al. Tiotropium bromide, a new long-acting antimuscarinic bronchodilator: a pharmacodynamic study in patients with chronic obstructive pulmonary disease (COPD). Eur Respir J 1995; 8:1506--1513
(*) From the National Jewish Medical and Research Center (Drs. Martin and Bartelson), Denver, CO; Johns Hopkins Asthma and Allergy Center (Dr. Smith), Baltimore, MD; MetroHealth Medical Center (Dr. Hudgel), Cleveland, OH; Harbor UCLA Medical Center (Dr. Lewis), Torrance, CA; and Boehringer Ingelheim Pharmaceuticals Inc (Drs. Pohl and Souhrada and Mr. Koker), Ridgefield, CT.
Supported by a grant from Boehringer Ingelheim Pharmaceuticals Inc, Ridgefield, CT.
Manuscript received December 31, 1997; revision accepted January 7, 1999.
Correspondence to: Richard J. Martin, MD, FCCP, National Jewish Medical and Research Center, 1400 Jackson St, Denver, CO 80206; e-mail: martinr@njc.org
COPYRIGHT 1999 American College of Chest Physicians
COPYRIGHT 2000 Gale Group