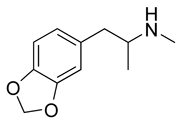
The phenylalkylamine derivatives, 3,4-methylenedioxymethamphetamine (MDMA, ecstasy, XTC, Adam), 3,4-methylenedioxyethamphetamine (MDEA, MDE, Eve), and 3,4-methylenedioxyamphetamine (MDA), are psychostimulants with hallucinogenic properties. MDA is also a metabolite of both MDMA and MDEA. These drugs are ring-substituted amphetamine derivatives that produce hallucinogenic, entactogenic ('love drug'), and stimulating effects.1-3 MDMA was initially developed as an appetite suppressant, however, its use as a therapeutic drug has been very limited.4 Because of its effects as a hallucinogenic psychostimulant with relatively low toxicity, it has emerged over the last two decades as a common recreational psychostimulant or 'club drug' at 'raves'.5 MDMA, MDEA, and MDA are often referred to as 'rave' or 'designer' drugs. They are produced in clandestine laboratories and have an increasing presence on the illicit drug market worldwide. Significant adverse health effects have been reported that include: serotonin neurotoxicity, severe psychiatric disorders, renal failure, malignant hyperthermia, hepatitis, rhabdomyolysis, and disseminated intravascular coagulation.6,8 A number of fatal outcomes associated with severe MDMA intoxication have been reported.9-12
ABBREVIATIONS: Adam = 3,4-methylenedioxymethamphetamine; ecstasy = 3,4-methylenedioxymethamphetamine; Eve = 3,4-methylenedioxyethamphetamine; GC = capillary gas chromatography; GC/MS = gas chromatography/mass spectrometry; HPLC = high performance liquid chromatography; MDA = 3,4-methylenedioxyamphetamine; MDE = 3,4-methylenedioxyethamphetamine; MDEA = 3,4-methylenedioxyethamphetamine; MDMA = 3,4-methylenedioxymethamphetamine; XTC = 3,4-methylenedioxy-methamphetamine.
INDEX TERMS: drug testing; hallucinogenic drugs.
Clin Lab Sci 2005;18(2):119
The analysis of MDMA, MDEA, and MDA can be broken down into several categories. The first is the need to identify the presence of the drugs in tablets that are seized and suspected to contain illicit drugs. The second is the need to detect 'rave' drugs onsite with the intent to determine recent use of the drugs. The third category is the typical laboratory drug screen used to determine either recent or chronic exposure to the drugs. And finally, the fourth category is forensic analysis of postmortem specimens for the presence of the drugs. The specimens, methodology, and instrumentation vary with each of the categories. Table 1 summarizes the methods that have been developed and reported for these categories.
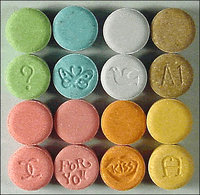
ANALYSISOFTABLETS
Tablets containing MDMA and other psychostimulants are prepared in clandestine laboratories worldwide. The tablets vary in size and typically have logos such as a pitbull, sparrow, butterfly, 'e', or 'X-files' imprinted on the tablets.13 The concentration of the active ingredients varies widely even among tablets from same origin.14 The excipients or inert ingredients found in tablets include glucose, sorbitol, and cellulose.15 Despite variation in concentration of the active ingredients, analysis of the tablets is helpful in identification of the clandestine laboratory that manufactured them. A number of analytical techniques have been applied to the characterization of the seized tablets. Raman spectroscopy of the active components and the excipients in tablets has been successfully used to identify tablets from the same source based on the state of hydration and the drug/excipient ratio.15'18 Another approach is analysis of impurities and byproducts of synthesis by gas chromatography/mass spectrometry (GC/MS), capillary gas chromatography (GC), or high performance liquid chromatography (HPLC).19'20 Isotopic analysis of the tablets for the ratios of deuterium, carbon 13, and nitrogen 15 in the active ingredients has been reported as a characteristic that is unique to the site of manufacture and may be a reliable method of fingerprinting the tablets.21,22 Capillary zone electrophoresis with ultraviolet detection is a rapid method suitable for routine analysis of MDMA content in tablets.23
ONSITE DETECTION OF PSYCHOSTIMULANTS
When individuals at the scene of a 'rave' party, accident, or crime are taken into custody, the need arises for a rapid onsite detection method for MDMA and related drugs. Some immunoassays that have been developed for detection of methamphetamine have high cross reactivity with MDMA and MDA, which make the assays potentially suitable for onsite screens where abuse of psychostimulants is suspected.24 Procedures have been reported for onsite analysis of saliva and sweat.24'27 The concentrations of MDMA and MDA in saliva have pharmacokinetic parameters that are similar to plasma, thus demonstrating that saliva is a useful and less invasive alternative to analysis of plasma.28 Studies have shown that individuals taking a single 100 mg dose of MDMA consistently have detectable levels of MDMA in both sweat and saliva after 1.5 hours. After six hours, most individuals remain positive; however, the number of false negatives begins to increase significantly to almost 20%.25 Drugwipe® has been successfully applied to onsite screens of both saliva wiped from the tongue and sweat collected from armpits.26,27 The drug may be quantified and cutoff limits established with a hand photometer, Drugread®.26
DETECTION OF ILLICIT PSYCHOSTIMULANTS IN DRUG SCREENS
Laboratory drug screens for detection of MDMA, MDEA, and MDA typically measure the presence of these substances in plasma, urine, saliva, or hair.29~31 The methods used for detection range from relatively rapid basic immunoassays to the more sophisticated and more labor intensive methods such as liquid chromatography with tandem mass spectrometry (LC/MS/MS).29,30 Plasma and saliva concentrations indicate recent drug abuse less than 24 hours, whereas urine concentrations reflect drug intake within the previous 48 hours.27 Analysis of hair provides a historical perspective that suggests chronic abuse of the drugs.31 After a single 100 mg dose of MDMA, the concentration of the drug peaks at 1.5 hours after intake with concentrations ranging from 135 to 233 ng/ mL in plasma and from 1729 to 6510 ng/mL in saliva. After 24 hours, the MDMA levels in plasma and saliva decrease to mean concentrations of 14 ng/mL and 126 ng/mL, respectively.28 In urine, significant concentrations of MDMA are detectable up to 48 hours yielding a positive screen in urine while the results for plasma and saliva are negative.26,27
Immunoassays for amphetamine and methamphetamine generally have high cross reactivity with related drugs and have been successfully applied to urine screens for the detection of MDMA and MDA.30 The assays have sufficient sensitivity for reliable detection of the drugs at the established cutoff of 500 ng/mL and agree well with results confirmed by GC/MS. The high cross reactivity of immunoassays with structures similar to amphetamine and methamphetamine may result in false positives for MDMA when other substances such as ephedrine or pseudoephedrine are present.30
Capillary electrophoresis with electrochemical and fluorescence detection has been successfully applied to the analysis of MDMA in urine with detection limits of 4 ng/mL with an electrochemical detector and 50 ng/mL with a fluorescence detector.32,33 Chromatographic techniques such as HPLC with fluorescence detection have been used for measurement of MDMA in plasma and urine with a detection limit of 25 ng/mL.34 Mass spectrometry methods including GC/MS and LC/MS/MS have been reported for the analysis of plasma and saliva for MDMA and its metabolites with detection limits of 6 ng/mL and 2 ng/mL, respectively.28,29
Hair analysis has been studied as a specimen that may be useful for determination of past chronic exposure to illicit drugs.31 Hair is a complex structure that grows approximately one cm/month. During its growth, hair is exposed to substances present in the capillary blood circulation near the follicle and substances excreted in sweat at the base of the follicle. Drugs in contact with hair penetrate and embed in the core of the hair stock and remain in the stock for an extended period of time. In the hair stock, drugs are relatively protected from the environment; however, extensive washing of the hair will cause some loss of the embedded drugs. Also, external contact with drugs in powder or liquid form will cause penetration of the hair stock.31 Nevertheless, it has been shown to be a useful indicator of chronic drug use and is widely accepted as a suitable specimen for drug screens including the detection of MDMA and MDA.35 All methods for hair analysis require digestion of the hair sample followed by extraction of the drugs. The accepted cutoff for a positive hair sample is 0.1 ng/mg.36 Most methods developed for the analysis of drugs in hair use GC/MS instrumentation to obtain the necessary sensitivity.37-42 Hair samples range in weight from 10 to 50 mg. Other methods that have been successfully applied to hair analysis for MDMA include capillary electrophoresis, radioimmunoassay, HPLC, and ion mobility spectrometry.31,36,43,44
FORENSICANALYSIS OF PSYCHOSTIMULANTS
Analysis of postmortem specimens for the presence of psychostimulants such as MDMA, MDEA, and MDA typically involves extraction of the drugs from tissues including liver, muscle, and brain as well as from urine, central blood, peripheral blood, and vitreous humor.45 Varying degrees of putrefaction and postmortem redistribution of drugs further complicate the analysis. While hair and urine are suitable forensic specimens to determine the presence of the drugs, peripheral blood and vitreous humor are reported to provide the best estimate of the blood concentration at the time of death.45-48
There are various analytical techniques available for initial screening, confirmation, and quantification of forensic specimens such as thin-layer chromatography (TLC), HPLC, and GC/MS.45-47 TLC is a common initial screening technique when a method capable of detecting a broad-spectrum of drugs in urine specimens is required. Identification is based on Rf value and the color characteristics following exposure to specific staining reagents. The Toxi-Lab A® system for the detection of basic and neutral drugs in urine specimens is able to differentiate sympathomimetic amines such as ephedrine, pseudoephedrine, and phenylpropanolamine from illicit dugs such as amphetamine, methamphetamine, MDMA, and MDA. Sensitivity for most of the drugs in this class using this procedure is approximately 500 ng/mL.
Immunoassays may also be applied to forensic drug screens for the presence of MDMA and related metabolites.30 However, as mentioned earlier, immunoassay techniques for the detection of amphetamine and methamphetamine have variable amounts of antibody cross reactivity to other structurally related sympathomimetic amines including pseudoephedrine and ephedrine.30 Antibody cross reactivity is variable and dependent on both the concentration of the structurally related analyte present in the specimen as well as the source of the antibodies used for detection. Higher levels of antibody cross reactivity occur with polyclonal antibody assays in comparison to monoclonal antibody assays. Monoclonal antibody assays are more specific and exhibit less cross-reactivity to structurally related compounds and should be used when high selectivity is desired. Application of immunoassay techniques for the analysis of postmortem specimens poses a problem due to decomposition occurring during the postmortem interval. This may result in the production of biogenic amines such as beta-phenethylamine or tyramine that have the potential to produce a false positive with amphetamine immunoassays due to the cross reactivity with these analytes. Due to the lack of specificity associated with immunoassays for identification of the specific psychostimulants present in the sample, confirmation of positive immunoassay results should be made using an alternate analytical methodology. GC/MS analysis with selective ion monitoring is the analytical methodology routinely utilized for drug confirmation and quantification. Derivatization of the drugs with heptafluorobutyric anhydride, pentafluoropropionic anhydride, or trifluoroacetic anhydride prior to analysis improves chromatographic behavior and reduces fragmentation so that higher mass fragments can be used for GC/MS selective ion monitoring which allows a more definitive identification and confirmation of the drugs.
CONCLUSION
A wide range of analytical methods have been developed for analysis of MDMA and related psychostimulants. Analysis by GC/MS is the technique that has been reported the most often and has been applied to the widest range of specimen types. No doubt this is due to the high specificity combined with high sensitivity that is found in GC/MS applications. However, there are a number of alternate methods using technologies such as immunoassay, HPLC, and electrophoresis that have sufficient sensitivity and specificity for detection of MDMA in routine screening applications in the laboratory. Furthermore, these alternative methods are more easily automated and more suitable for high volume applications.
REFERENCES
1. Nichols DE. Differences between the mechanism of action of MDMA, MBDB, and the classic hallucinogens. Identification of a new therapeutic class: entactogens. J Psychoactive Drugs 1986;18:305-13.
2. Steele TD, McCann UD, Ricaurte GA. 3,4-methylenedioxymethamphetamine (MDMA, 'ecstasy'): pharmacology and toxicology in animals and humans. Addiction 1994;89:539-51.
3. Hermle L, Spitzer M, Borchardt D, and others. Psychological effects of MDE in normal subjects. Are entactogens a new class of psychoactive agents? Neuropsychopharmacology 1993;8(2):171-6.
4. Climko RP, Roehrich H, Sweeney DR, and others. Ecstacy: a review of MDMA and MDA. Int J Psychiatry Med 1986; 16:359-72.
5. Arria AM, Yacoubian GS Jr, Post E, and others. The pediatrie forum: ecstasy use among club rave attendees. Arch Pediatr Adolesc Med 2002;156:295-6.
6. Parrott AC. Recreational ecstasy/MDMA, the serotonin syndrome, and serotonergic neurotoxicity. Pharmacol Biochem Behav 2002:71:837-44.
7. McCann UD, Eligulashvili V, Ricaurte GA. (+/-)3,4-methylenedioxymethamphetamine ('ecsrasy')-induced serotonin neurotoxicity: clinical studies. Neuropsychobiology 2000;42:11-6.
8. McCann UD, Slate SO, Ricaurte GA. Adverse reactions with 3,4-methylenedioxymethamphetamine (MDMA; 'ecstasy'). Drug Saf 1996:15:107-15.
9. Fineschi V, Masti A. Fatal poisoning by MDMA (ecstasy) and MDEA: a case report. Int J Legal Med 1996;108:272-5.
10. IwersenS, Schmoldt A. Two very different fatal cases associated with the use of methylenedioxyethylamphetamine (MDEA) : Eve as deadly as Adam. ClinToxicol 1996;34:24l-4.
11. Randall T Ecstasy-fueled 'Rave' parties become dances of death for English youths. JAMA 1992;268:1505-6.
12. Henry JA, Jeffreys KJ, Dawling S. Toxicity and deaths from 3,4-methylenedioxymethamphetamine ('ecstasy'). Lancet 1992;340:384-7.
13. Schneider RC, Kovar KA. Analysis of ecstasy tablets: comparison of reflectance and transmittance near infrared spectroscopy. Forensic Sci Int 2003:134:187-95.
14. Sherlock K, WolffK, Hay AW, and others. Analysis of illicit ecstasy tablets: implications for clinical management in the accident and emergency department. J Accid Emerg Med 1 999; 16:194-7.
15. Bell SE, Burns DT, Dennis AC, and others. Composition profiling of seized ecstasy tablets by Raman spectroscopy. Analyst 2000:125:1811-5.
16. Bell SE, Burns DT, Dennis AC, and others. Rapid analysis of ecstasy and related phenethylamines in seized tablets by Raman spectroscopy. Analyst 2000;125:54l-4.
17. Bell SE, Barren LJ, Burns DT, and others. Tracking the distribution of 'ecstasy' tablets by Raman composition profiling: a large scale feasibility study. Analyst 2003:128:1331-5.
18. Ryder AG. Classification of narcotics in solid mixtures using principal component analysis and Raman spectroscopy. J Forensic Sci 2002:47:275-84.
19. ChengWC, PoonNL, ChanMF. Chemical profiling of 3,4-methylcnedioxymethampheramine (MDMA) tablets seized in Hong Kong. J Forensic Sd 2003:48:1249-59.
20. Palhol F, Boyer S, Naulet N, and others. Impurity profiling of seized MDMA tablets by capillary gas chromatography. Anal Bioanal Chem 2002:374:274-81.
21. Carter JF, Titterton EL, Murray M, and others, lsotopic characterisation of 3,4-methylenedioxyamphetamine and 3,4-methylenedioxymethylamphctamine (ecstasy). Analyst 2002;127:830-3.
22. Palhol F, Lamoureux C, Naulet N. 15N isotopic analyses: a powerful tool to establish links between seized 3,4-methylenedioxymethamphetamine (MDMA) tablets. Anal Bioanal Cliem 2003:376:486-90.
23. Frost M, Kohler H, Blaschke G. Analysis of 'ecstasy' by capillary electrophoresis. Int J Legal Med 1996;109:53-7.
24. Fay J, Fogerson R, Schoendorfer D, and others. Detection of methamphetamine in sweat by EIA and GC-MS. J Anal Toxicol 1996;20:398-403.
25. Pichini S, Navarro M, Pacifici R, and others. Usefulness of sweat testing for the detection of MDMA after a single-dose administration. J Anal Toxicol 2003;27:294-303.
26. Pichini S, Navarro M, Farre M, and others. On-site testing of 3,4methylenedioxymethamphetamine (ecstasy) in saliva with Drugwipe and Drugread: a controlled study in recreational users. Clin Chem 2002;48:174-6.
27. Pacifici R, Farre M, Pichini S, and others. Sweat testing of MDMA with the Drugwipe analytical device: a controlled study with two volunteers. J Anal Toxicol 2001;25:144-6.
28. Navarro M, Pichini S, Farre M, and others. Usefulness of saliva for measurement of 3,4-methylenedioxymethamphetamine and its metabolites: correlation with plasma drug concentrations and effect of salivary pH. Clin Chem 2001;47:1788-95.
29. Wood M, De Boeck G, Samyn N, and others. Development of a rapid and sensitive method for the quantitation of amphetamines in human plasma and oral fluid by LC-MS-MS. J Anal Toxicol 2003;27:78-87.
30. Stout PR, Klette KL, Wiegand R. Comparison and evaluation of DRI methamphetamine, DRT ecstasy, Abuscreen ONLINE amphetamine, and a modified Abuscreen ONLINE amphetamine screening immunoassays for the detection of amphetamine (AMP), methamphetamine (MTH), 3,4-methylenedioxyamphetamine (MDA), and 3,4-methylenedioxymethamphetamine (MDMA) in human urine. J Anal Toxicol 2003;27:265-9.
31. Tagliaro F, Manetto G, Crivellente F, and others. Hair analysis for abused drugs by capillary zone electrophoresis with field-amplified sample stacking. Forensic Sci Int 1998;92:201-11.
32. BackofenU, MatysikFM, HoffmannW, and others. Analysis of illicit drugs by nonaqueous capillary electrophoresis and electrochemical detection. Fresenius J Anal Chem 2000;367:359-63.
33. Fang C, Chung YL, Liu JT and others. Rapid analysis of 3,4-methylenedioxymethamphetamine: a comparison of nonaqueous capillary electrophoresis/fluorescence detection with GC/MS. Forensic Sci Int 2002;125:142-8.
34. Herraez-Hernandez R, Campins-Falco P, Verdu-Andres J. Sensitive determination of methylenedioxylated amphetamines by liquid chromatography. Analyst 2001;126:581-6.
35. Kintz P, Cirimele V. Interlaboratory comparison of quantitative determination of amphetamine and related compounds in hair samples. Forensic Sci Int 1997;84:151-6.
36. Tagliaro F, Valentini R, Manetto G, and others. Hair analysis by using
radioimmunoassay, high-performance liquid chromatography and capillary electrophoresis to investigate chronic exposure to heroin, cocaine and/or ecstasy in applicants for driving licenses. Forensic Sci Int2000;107:121-8.
37. Pujadas M, Pichini S, Poudevida S, and others. Development and validation of a gas chromatography-mass spectrometry assay for hair analysis of amphetamine, methamphetamine, and methylenedioxy derivatives. J Chromatogr B Analyt Technol Biomed Life Sci 2003:798:249-55.
38. Kintz P, Cirimele V, Tracqui A, and others. Simultaneous determination of amphetamine, methamphetamine, 3,4-methylenedioxyamphetamine, and 3,4-methylenedioxymethamphetamine in human hair by gas chromatography-mass spectrometry. J Chromatogr B Biomed Appl 1995:670:162-6.
39. Alien DL, Oliver JS. The use of supercritical fluid extraction for the determination of amphetamines in hair. Forensic Sci Int 2000:107:191-9.
40. Cooper GA, Alien DL, Scott KS, and others. Hair analysis: self-reported use of'speed' and 'ecstasy' compared with laboratory findings. J Forensic Sci 2000:45:400-6.
41. UhI M. Determination of drugs in hair using GC/MS/MS. Forensic Sd Int 1997:84:281-94.
42. Rothe M, Pragst F, Spiegel K, and others. Hair concentrations and self-reported abuse history of 20 amphetamine and ecstasy users. Forensic Sci Int 1997:89:111-28.
43. Tagliaro F, De Battisti Z, Groppi A, and others. High sensitivity simultaneous determination in hair of the major constituents of ecstasy (3,4-methylenedioxymethamphetamine, 3,4-methylenedioxyamphetamine, and 3,4-methylene-dioxyethylamphetamine) by high-performance liquid chromatography with direct fluorescence detection. J Chromatogr B Biomed Sci Appl 1999:723:195-202.
44. Keller T. Miki A. Regenscheit P, and others. Detection of designer drugs in human hair by ion mobility spectrometry (IMS). Forensic Sd Int 1998:94:55-63.
45. De Letter EA, Bouche MP, Van Bocxlaer JF, and others. Interpretation of a 3,4-methylenedioxymethamphetamine (MDMA) blood level: discussion by means of a distribution study in two fatalities. Forensic Sci Int 2004:141:85-90.
46. Clauwaert KM, Van Bocxlaer JF, De Letter EA, and others. Determinarion of the designer drugs 3, 4-methylenedioxymethamphetamine, 3,4-methylenedioxyethylamphetamine, and 3,4-methylenedioxyamphetamine with HPLC and fluorescence detection in whole blood, serum, vitreous humor, and urine. Clin Chem 2000:46:1968-77.
47. UhI M. Tandem mass spectrometry: a helpful tool in hair analysis for the forensic expert. Forensic Sci Int 2000;107:l69-79.
48. De Letter EA, De Paepe P, Clauwaert KM, and others. Is vitreous humour useful for the interpretation of 3,4-methylenedioxymethamphetamine (MDMA) blood levels? Experimental approach with rabbits. Int J Legal Med 2000;! 14:29-35.
Victor A Skrinska PhD DABCC is Professor and Chair, university of Alabama at Birmingham, Department of Diagnostic and Therapeutic Sciences, Birmingham AL.
Susan B Gock MSMT(ASCP) is Forensic Laboratory Technical Director, Milwaukee County Medical Examiner's Office, Milwaukee WI.
Address for correspondence: Victor A Skrinska PhD DABCC, Professor and Chair, University of Alabama at Birmingham, Department of Diagnostic and Therapeutic Sciences, 1530 3rd Ave S, Birmingham AL 35294-1212. (205) 934-9124. skrinska@uab.edu
Victor A Skrinska PhD DABCC is the Focus: Psychostimulants guest editor.
Focus Continuing Education Credit: see pages 124 to 126 For learning objectives, test questions, and application form.
Copyright American Society for Clinical Laboratory Science Spring 2005
Provided by ProQuest Information and Learning Company. All rights Reserved