Our aim in the study was to investigate the pathogenesis of eosinophilic inflammation in patients with acute eosinophilic pneumonia (AEP), and to determine the levels of (1[right arrow]3)-[beta]-D-glucan, which is one Of the major components of the cell wall of most fungi, in the BAL fluid (BALF) of those patients with AEP. Six patients with AEP and five patients with chronic eosinophilic pneumonia (CEP) that was in the acute stage and had been newly diagnosed, and nine healthy subjects from the Kurume University School of Medicine and the Social Institute Tagawa Hospital between 1995 and 2001 were entered into the study. In AEP patients, (1[right arrow]3)-[beta]-D-glucan was detected in BALF, and these findings were compared with BALF findings in patients with CEP as well as with those in healthy subjects. In the BALF of AEP patients, the mean concentration of (1[right arrow]3)-[beta]-D-glucan was significantly higher (p < 0.05) than that of CEP patients as well as healthy subjects. In patients with AEP, the mean concentration of (1[right arrow]3)-[beta]-D-glucan in BALF was significantly higher (p < 0.05) than that in the blood. In four of six patients with AEP, we measured serial changes in (1[right arrow]3)-[beta]-D-glucan levels, and the level of (1[right arrow]3)-[beta]-D-glucan in the BALF decreased with clinical improvement at follow-up. We concluded that inhaled (1[right arrow]3)-[beta]-D-glucan may be involved in the mechanisms of pulmonary inflammation in patients with AEP.
Key words: BAL; (1[right arrow]3)-[beta]-D-glucan; eosinophil; pneumonia
Abbreviations: AEP = acute eosinophilic pneumonia; BALF = BAL fluid; CEP = chronic eosinophilic pneumonia; PCR = polymerase chain reaction
**********
Acute eosinophilic pneumonia (AEP) is a recently defined clinical entity showing an acute febrile illness that can result in life-threatening respiratory failure. (1-3) Intervention with corticosteroids results in the rapid reversal of respiratory failure and complete recovery without relapse. (3) The widespread use of BAL as a diagnostic tool has resulted in the recognition of new forms of eosinophilic lung syndromes that lack prominent blood eosinophilia. Several etiologic agents associated with AEP have been described, including drugs, smoking, fungal and parasitic infections, and systemic vasculitis. (3-9) In most cases, the cause remains unknown, and idiopathic AEP is diagnosed. (3)
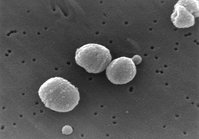
(1[right arrow]3)-[beta]-D-glucan is one of the major components of the cell wall of most fungi. The Fungitec G test (Seikagaku Kogyo Co; Tokyo, Japan), which measures the concentration of (1[right arrow]3)-[beta]-D-glucan, is a diagnostic method for deep mycosis. (10-12) We measured the concentration of (1[right arrow]3)[beta]-D-glucan in BAL fluid (BALF) from patients with AEP, those with chronic eosinophilic pneumonia (CEP) and healthy subjects (control group). The levels of (1[right arrow]3)-[beta]-D-glucan in BALF also were compared with the levels of other components in BALF and with plasma (1[right arrow]3)-[beta]-D-glucan levels.
MATERIALS AND METHODS
Subjects
Patients With AEP: Six patients with AEP (four men and two women; mean [[+ or -] SD]age, 31.7 [+ or -] 26.9 years; age range, 16 to 86 years) were studied. All patients were in the acute stage and had received their diagnoses in Kurume University School of Medicine and Social Institute Tagawa Hospital between 1995 and 2001. Five patients were current-smokers who had just started smoking cigarettes, and one patient was a nonsmoker. None had been receiving corticosteroids and antifungal agents before undergoing their first fiberoptic bronchoscopy. A diagnosis of AEP was established on the basis of criteria that have been previously described by Allen and Davis. (2) In short, the entry criteria were as follows: (1) acute onset; (2) febrile illness; (3) bilateral infiltrates seen on a chest radiograph; (4) dyspnea or hypoxemic respiratory failure; (5) eosinophilia of > 25% in BALF or the predominance of eosinophils in open-lung biopsy; (6) no history of hypersensitivity to drugs and no evidence of infection; and (7) a prompt and complete response to corticosteroids and no relapse after the discontinuation of therapy with corticosteroids.
The Pa[O.sub.2] in arterial blood gas ranged from 37.0 to 82.7 mm Hg (mean, 63.4 [+ or -] 15.8 mm Hg), when breathing room air. There were no pathogenic microorganisms detected either in the sputum or on a pharyngeal swab. The interval between the onset of illness and BAL ranged from 3 to 43 days (mean, 12.6 [+ or -] 15.1 days). All patients were regarded as having idiopathic AEP of unknown cause.
Patients With CEP: Five active, untreated, and newly diagnosed patients with CEP (two men and three women; mean age, 71.6 [+ or -] 9.6 years) were evaluated. All patients had the clinical characteristics of CEP described by Carrington et al, (13) including histologic findings on transbronchial lung biopsy. No patients had evidence of bacterial, mycobacterial, fungal, or parasitic infections. Three patients had a history of bronchial asthma but had never received therapy with corticosteroids orally or by inhalation before undergoing their first fiberoptic bronchoscopy. One patient had a history of diabetes mellitus for 2 years. Four patients were smokers, and one patient was a nonsmoker. Two patients had peripheral blood eosinophilia exceeding 500 cells/[micro]L.
Healthy Subjects (Control Group): The control group consisted of nine healthy subjects (six men and three women; mean age, 62.3 [+ or -] 11.0 years) with no evidence of diffuse respiratory disease. They underwent bronchoscopy as a diagnostic procedure to evaluate a history of minor hemosputum, a solitary peripheral lung nodule (< 2 cm in size), or other minimal radiologic findings found on their chest roentgenogram. None of the patients had received corticosteroids, antibiotics or antifungal agents in the previous month. Four subjects were smokers, and five subjects were nonsmokers.
Informed consent was obtained from each volunteer in the study according to institutional guidelines.
BAL
Fiberoptic bronchoscopy was performed as previously described. (14,15) The patients gargled with a mouthwash with 1 to 3% povidone-iodine (Meiji Co; Tokyo, Japan) just before the examination. The bronchoscope was inserted through the mouth in patients who were not intubated. In all patients with AEP and in healthy subjects, the tip of the bronchoscope was wedged into a distal portion of a bronchus in the right middle lobe, and BAL was performed by instilling three 50-mL aliquots of a sterile saline solution through the bronchoscope. To obtain BALF from patients with CEP, the tip of the bronchoscope was wedged into the bronchus showing pulmonary infiltrates on a chest CT scan. Samples of BALF were taken for fungal, mycobacterial, viral, Legionella, and other bacterial cultures. Some of the fluids underwent cytocentrifugation, and the pellets were examined for cellular differentials with the use of May-Giemsa stain, and for microorganisms using Gram stain, acid-fast bacilli, and Groccot stain. At follow-up, after the conditions of four of six patients with AEP had improved, BAL was performed for the second time.
Detection of (1[right arrow]3)-[beta]-D-Glucan in BALF and Plasma
The concentrations of (1[right arrow]3)-[beta]-D-glucan were measured by the Fungitec G test, as reported previously. (12) In brief, 2.0 mL BALF and blood were drawn into pyrogen-free disposable syringes, underwent anticoagulation with 5.0 U/mL heparin, underwent centrifugation immediately at 1,000g for 10 min, and was stored at -80[degrees]C. A 5.0-mL sample of BALF and plasma was pretreated with 20 mL test solution containing 0.15 mol/L KOH, 0.3 mol/L KCl, and 0.1% polybrene, and the mixture was incubated at 37[degrees]C for 10 min. The pretreated sample was added to 100 mL factor G dissolved in HCO(3-)-free N-2-hydroxyethyl-piperazine-N'-2-ethanesulfonic acid buffer (0.1 mol/L; pH 7.6), and then was incubated at 37[degrees]C for 30 min. The optical density of 405 nm was measured using the kinetic mode of a computerized well-reader (model SK601; Seikagaku Kogyo Co). The concentration of (1[right arrow]3)-[beta]-D-glucan below the detection limit of the test was 1.0 pg/mL.
Serologic Tests for Fungi
Serum specimens were obtained from the patients with AEP on hospital admission. The serum Candida antigen was determined by a commercial test (Cand-Tec test; Ramco Laboratories, Inc; Houston, TX). (16) The serum galactomannan antigen for Aspergillus spp was detected by a latex agglutination test (Mitubishi Kagaku Bio-Clinical Labs, Inc.; Tokyo, Japan). (17) The serum Cryptococcus antigen was detected by a commercial test (SERODIRECT "EIKEN" Cryptococcus; Eiken Chemical; Tokyo, Japan). (18) To test for the precipitating antibodies of Trichosporon spp, these sera were sent to the First Department of Internal Medicine, Kumamoto University School of Medicine. (19,20)
Detection of Pneumocystis carinii DNA Fragments in BALF by Capillary Polymerase Chain Reaction
BALF samples were obtained from patients with AEP to detect the specific DNA fragments of P carinii by polymerase chain reaction (PCR), as previously described. (21) All BALF samples were pelleted by centrifugation at 1,600g for 10 min, after which the supernatant was removed. The pellets were resuspended in TE buffer containing 10 mmol/L Tris-HCl (pH 8.0), 100 mmol/L KCL, 2.5 mmol/L MgCl2, 1% Tween 20, 1% NP 40, and 80 [micro]g protein kinase K per milliliter for 60 min at 56[degrees]C and then were incubated for 10 min at 100[degrees]C. One microliter of this sample was used as a DNA sample for PCR.
The two oligonucleotide primers PAZ102-E (5'-GATGGCT-GTTTCCAAGCCCA-3') and PAZ102-H (5'-GTGTACGTTG-CAAAGTACTC-3') were synthesized with a DNA synthesizer (MilliGen/Biosearch; Burlington, MA). The amplification product consisted of a 346-base pair DNA fragment.
DNA amplification for capillary PCR was performed in 50 mmol/L Tris (pH 8.5), 3 mmol/L Mg[Cl.sub.2], 20 mmol/L KCl, 500 [micro]g bovine serum albumin per milliliter, 0.5 [micro]mol each of the primer, 0.5 mmol each deoxynucleotide triphosphate, 1 [micro]L DNA sample, and 0.4 U taq polymerase (Promega Co; Madison, WI) per 10 [micro]L unless specified otherwise. Thirty-five cycles of DNA amplification were performed in a hot-air thermal cycler (Idaho Technology; Moscow, ID). The thermal profile is as follows: (1) denaturation at 94[degrees]C for 3 s; (2) annealing at 55[degrees]C for 3 s; and (3) extension at 72[degrees]C for 3 s.
The amplifications were subjected to electrophoresis in agarose gels, which were tested for the presence of bands by visualization with ultraviolet light after ethidium bromide staining.
Statistical Analysis
The data were expressed as mean [+ or -] SD. Differences in the concentration of (1[right arrow])-[beta]-D-glucan in BALF and plasma, and total and differential cell counts in BALF were tested by the unpaired Wilcoxon test. Significance was accepted when p < 0.05.
RESULTS
Clinical and BALF Characteristics of the Patients With AEP
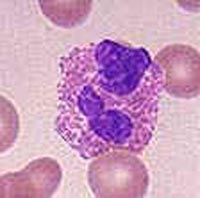
Table 1 shows the clinical and BALF characteristics of six patients with AEP. The median plasma (1[right arrow]3)-[beta]-D-glucan level in patients with AEP was 5.0 pg/mL (range, 1.0 to 16.5 pg/mL). The median BALF recovery of 150 mL BALF instilled was 59.8 [+ or -] 9.9%. The absolute number of cells recovered from BAL in these patients was markedly elevated (11.5 [+ or -] 6.0 x [10.sup.5] cells/mL; range, 5.0 to 21.5 x [10.sup.5] cells/mL), with a high percentage of eosinophils (54.4 [+ or -] 15.4%; range, 29.0 to 64.2%), and a low percentage of alveolar macrophages (21.1 [+ or -] 7.8%; range, 11.0 to 32.0%).
Analysis of Cells in BALF
The median number of cells in BALF in AEP patients was significantly elevated, with a high percentage of eosinophils and low percentage of alveolar macrophages compared to CEP patients and control subjects (Table 2).
(1[right arrow]3)-[beta]-D-Glucan Levels in BALF
The (1[right arrow]3)-[beta]-D-glucan levels in BALF are shown in Figure 1. The levels in all samples obtained from patients with AEP were > 100 pg/mL. In contrast, the levels in four of five patients with CEP and in all healthy subjects were < 20 pg/mL as a cutoff value. The median concentration of (1[right arrow]3)-[beta]-D-glucan in the BALF of AEP patients was significantly higher (851.7 [+ or -] 866.0 pg/mL; range, 216 to 2,571 pg/mL) than that of CEP patients (18.2 [+ or -] 31.1 pg/mL) and healthy subjects (2.5 [+ or -] 1.4 pg/mL; p < 0.01). The median concentration of (1[right arrow]3)-[beta]-D-glucan in BALF was significantly higher than that in blood (p < 0.01) in AEP patients.
[FIGURE 1 OMITTED]
In four of the six patients with AEP who underwent follow-up BAL, changes in (1[right arrow]3)-[beta]-D-glucan levels in BALF were examined, and the findings before treatment (mean, 1,020.5 [+ or -] 1,057.9 pg/mL; range, 216 to 2,571 pg/mL) and after treatment (mean, 4.6 [+ or -] 5.6 pg/mL; range, 1.0 to 13 pg/mL) with corticosteroids were compared. The (1[right arrow]3)-[beta]-D-glucan levels in BALF from the second examination were significantly reduced (p < 0.01), as the patient's symptoms improved (Fig 2).
[FIGURE 2 OMITTED]
Analysis of Microorganisms
In patients with AEP, there were no infectious organisms identified by routine stains of cultures. In serologic studies, all patients had negative results (Table 3).
There were no samples that demonstrated the presence of P carinii DNA in BALF samples by capillary PCR, and there were no findings of P carinii infections in the lung tissue obtained by transbronchial lung biopsy.
DISCUSSION
This is the first report to demonstrate an increase in (1[right arrow]3)-[beta]-D-glucan concentrations in BALF from untreated patients with AEP. In contrast, the concentrations of (1[right arrow]3)-[beta]-D-glucan were lower in the BALF from CEP patients and healthy subjects. The elevation of (1[right arrow]3)-[beta]D-glucan levels in BALF decreased with clinical improvement in AEP patients. These findings strongly suggest the important contribution of (1[right arrow]3)-[beta]-D-glucan to the pathogenesis of AEP. The concentrations of (1[right arrow]3)-[beta]-D-glucan in BALF were significantly higher than those in plasma, suggesting the role of inhaled agents.
These findings suggest differences in the pathogenesis of eosinophilic inflammation between AEP and CEP patients. We focused on (1[right arrow]3)-[beta]-D-glucan because it is one of the ingredients in cigarettes and has been described as being related to the possible role of cigarette smoking in the pathogenesis of AEP. (9)
It is known that (1[right arrow]3)-[beta]-D-glucan composes a portion of the cell wall of most fungi. The detection of (1[right arrow]3)-[beta]-D-glucan in sera was used as a serologic marker for the diagnosis of deep mycosis. (10-12) In Japan, several cases have been reported (7,8) in which fungus was a possible cause of AEP, resembling a summer-type hypersensitivity pneumonitis. In the present patients, we could not detect fungi by the conventional technique. P carinii has been placed in a fungus family. (22,23) We tried to detect the specific DNA fragments of P carinii in the BALF obtained from the patients with AEP, but none were detected. P carinii DNA and the findings of P carinii infections in lung tissue were not obtained by transbronchial lung biopsy.
It is also known that (1[right arrow]3)-[beta]-D-glucan is a biological response modifier functioning as an immunomodulating and antitumor factor. When injected intraperitoneally in vivo, (1-[right arrow]3)-[beta]-D-glucan induces some inflammatory-like responses. In contrast, when guinea pigs undergo long-term exposure to (1[right arrow]3)-[beta]-D-glucan in vivo, it causes an increase in the number of eosinophils in the airway. (24-26) In humans, Rylander and Lin (27) have reported that the inhaled environment of (1[right arrow]3)-[beta]-D-glucan worsens in patients with bronchial asthma due to allergic mechanisms. Taken together, it is highly possible that (1[right arrow]3)-[beta]-D-glucan causes inflammatory responses that are characteristic of AEP. The origins of (1[right arrow]3)-[beta]-D-glucan and the exact mechanisms for the development of AEP were not demonstrated in this study.
In summary, based on the findings that (1[right arrow]3)-[beta]-D-glucan was increased in the BALF from AEP patients then decreased with clinical improvement, we conclude that the inhaled environment of (1[right arrow]3)-[beta]-D-glucan may be involved in the development of AEP. Further studies are needed to disclose the exact role of (1[right arrow]3)-[beta]-D-glucan in AEP, and that information will be of great importance in treating patients with AEP.
ACKNOWLEDGMENT: The authors thank Professor Masayuki Ando at the First Department of Internal Medicine, Kumamoto University School of Medicine, for examination of the precipitating antibodies of Trichosporon spp.
REFERENCES
(1) Allen JN, Pacht JE, Grdek JE, et al. Acute eosinophilic pneumonia as a reversible cause of noninfectious respiratory failure. N Engl J Med 1989; 321:569-574
(2) Allen JN, Davis WB. Eosinophilic lung diseases. Am J Respir Crit Care Med 1994; 150:1423-1438
(3) Pope-Harman AL, Davis WB, Allen ED, et al. Acute eosinophilic pneumonia: a summary of 15 cases and review of the literature. Medicine 1996; 75:334-342
(4) Ricker DH, Taylor SR, Gartner Jr JC, et al. Fatal pulmonary aspergillosis presenting as acute eosinophilic pneumonia in a previously healthy child. Chest 1991; 100:875-877
(5) Roig J, Romeu J, Riera C, et al. Acute eosinophilic pneumonia due to toxocariasis with bronchoalveolar lavage findings. Chest 1992; 102:294-296
(6) Brander PE, Tukiainen P. Acute eosinophilic pneumonia in a heroin smoker. Eur Respir J 1993; 6:750-752
(7) Miyazaki E, Sugisaki K, Shigenaga T, et al. A case of acute eosinophilic pneumonia caused by inhalation of Trichosporon terrestre. Am J Respir Crit Care Med 1995; 151:541-543
(8) Imokawa S, Sato A, Hayakawa H, et al. Possible involvement of an environmental agent in the development of acute eosinophilic pneumonia. Ann Allergy Asthma Immunol 1996; 76:419-422
(9) Taki R, Sawada M, Isogai S, et al. A possible role of cigarette smoking in the pathogenesis of acute eosinophilic pneumonia [abstract]. Am J Respir Crit Care Med 1996; 153:A271
(10) Obayashi T, Yoshida M, Mori T, et al. Plasma (1[right arrow]3)-[beta]-D-glucan measurement in diagnosis of invasive deep mycosis and fungal febrile episodes. Lancet 1995; 345:17-20
(11) Mori T, Ikemoto H, Matsumura M, et al. Evaluation of plasma (1[right arrow]3)-[beta]-D-glucan measurement by the kinetic turbidimetric limulus test, for the clinical diagnosis of mycotic infection. Eur J Clin Chem Clin Biochem 1997; 35:553-560
(12) Hossain MA, Miyazaki T, Mitsutake K, et al. Comparison between Wako-WB003 and Fungitec G tests for detection of (1[right arrow]3)-[beta]-D-glucan in systemic mycosis. J Clin Lab Anal 1997; 11:73-77
(13) Carrington CB, Addington WW, Golf AM, et al. Chronic eosinophilic pneumonia. N Engl J Med 1969; 280:787-798
(14) Hunnunghake GW, Gadek JE, Kawakami O, et al. Inflammatory and immune processes in the human lung in health and disease: evaluation by bronchoalveolar lavage. Am J Pathol 1979; 97:149-206
(15) Reynolds HY. Bronchoalveolar lavage. Am Rev Respir Dis 1987; 135:250-263
(16) Herent P, Stynen D, Hernando F, et al. Retrospective evaluation of two latex agglutination tests for detection of circulating antigens during invasive candidasis. J Clin Microbiol 1992; 30:2158-2164
(17) Van Cutsem J, Meulemans L, Van Gerven F, et al. Detection of circulating galactomannan by pastorex Aspergillus in experimental invasive aspergillosis. Mycoses 1990; 33:61-69
(18) Kohno S, Yasuoka A, Koga H, et al. High detection rates of cryptococcal antigen in pulmonary cryptococcosis by Eiken latex agglutination test with pronase pretreatment. Mycopathologia 1993; 123:75-79
(19) Shimazu K, Ando M, Sakata T, et al. Hypersensitivity pneumonitis induced by Trichosporon cutaneum. Am Rev Repir Dis 1984; 130:407-411
(20) Yoshida K, Ando M, Sakata T, et al. Environmental mycological studies on the causative agent of summer-type hypersensitivity pneumonitis. J Allergy Clin Immunol 1988; 81:457-483
(21) Honda J, Hoshino T, Natori H, et al. Rapid and sensitive diagnosis of cytomegalovirns and Pneumocystis carinii pneumonia in patients with haematological neoplasia by using capillary polymerase chain reaction. Br J Haematol 1994; 86:138-142
(22) Edman JC, Kovacs JA, Masur H, et al. Ribosomal RNA sequence shows Pneumocystis carinii to be a member of the fungi. Nature 1988; 334:519-522
(23) Yasuoka A, Tachikawa N, Shimada K, et al. (1[right arrow]3)-[beta]-D-glucan as quantitative serological marker for Pneumocystis carinii pneumonia. Clin Diagn Lab Immunol 1996; 3:197-199
(24) Wan GH, Li CS, Guo SP, et al. An airborne model-derived product, [beta]-1, 3-D-glucan, potentates airway allergic responses. Eur J Immunol 1999; 29:2491-2497
(25) Rylander R, Holt PG. (1[right arrow]3)-[beta]-D-glucan and endotoxin modulate immune response to inhaled allergen. Mediators Inflamm 1998; 7:105-110
(26) Fogelmark B, Thorn J, Rylander R. Inhalation of (1[right arrow]3)-[beta]-D-glucan causes airway eosinophilia. Mediators Inflamm 2000; 10:13-19
(27) Rylander R, Lin RH. (1[right arrow]3)-[beta]-D-glucan-relationship to indoor air-related symptoms, allergy and asthma. Toxicology 2000; 152:47-52
* From the First Department of Internal Medicine, Kurume University School of Medicine, Fukuoka, Japan.
Manuscript received June 24, 2002; revision accepted September 17, 2002.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@chestnet.org).
Correspondence to: Hisamichi Aizawa, MD, First Department of Internal Medicine, Kurume University School of Medicine, 67 Asahi-machi, Kurume-City, Fukuoka 830-0011, Japan; e-mail: aizawa@med.kurume-u.ac.jp
COPYRIGHT 2003 American College of Chest Physicians
COPYRIGHT 2003 Gale Group