Study objectives: Flexible bronchoscopy (FB) is an invasive procedure associated with patient discomfort and frequent nose pain. A simple sedation procedure that does not require the intervention of an anesthetist is of interest. The aim of this prospective, randomized, double-blind study was to assess efficiency of nitrous oxide inhalation on the reduction of FB-induced discomfort in adult patients.
Design and settings: Two hundred six patients were randomized to receive either a prefixed equimolar nitrous oxide/oxygen mixture ([N.sub.2]O) or a prefixed equimolar nitrogen and oxygen mixture (control). The primary outcome was stress as assessed by pulse rate and systemic BP during the procedure. Secondary outcomes were self-assessed pain using a visual analog scale (VAS) and patient satisfaction based on a questionnaire. Adverse events were recorded.
Results: A significant increase in BP was observed only in the control group (p = 0.003), while pulse rate values did not differ between the two groups. As assessed by the VAS, pain was lower in the [N.sub.2]O group as compared to placebo (p = 0.02). Nose pain and cough were also significantly reduced by [N.sub.2]O. Adverse events, mostly anxiety, were reported in 10 patients.
Conclusion: These results indicate that equimolar [N.sub.2]O inhalation is efficient in reducing patient discomfort and may be an alternative to general anesthesia.
Key words: bronchoscopy; conscious sedation; outpatients; randomized trial
Abbreviations: ANOVA = analysis of variance; FB = flexible bronchoscopy; [N.sub.2]O = nitrous oxide/oxygen mixture; NS = not significant; Sp[O.sub.2] = transcutaneous oxygen saturation; TO = 5 min before the procedure; T1 = passing through the nose; T2 = passing through the trachea; T3 = during bronchial sampling; T4 = 5 min after the end of the procedure; VAS = visual analog scale
Flexible bronchoscopy (FB) is a diagnostic and therapeutic tool of great value in clinical practice. However, it is an invasive procedure that is associated with frequent minor adverse effects such as nose and throat pain and with very few serious side effects. (1,2) A survey (3) in the United Kingdom reported the use of topical anesthesia alone by 10% of physicians and of a benzodiazepine sedation alone by 63%. An opioid alone or in combination with benzodiazepine were preferred by 28% of physicians. Sedation has been shown to allay anxiety and to reduce stress, to improve patient comfort and co-operation, to provide amnesia, and to facilitate the bronchoscopic procedure. (4) Various sedation protocols have been proposed. (4) Deep sedation may improve patient tolerance to the procedure but is associated with morbidity and mortality. (5-7) A study (8) in children suggests that nitrous oxide may be efficient in reducing patient discomfort during FB. Very few and minor side effects have been reported with the use of this gas, which is widely used for its analgesic properties associated with light sedation. (9,10) We therefore carried out a prospective, randomized, double-blind study to assess efficiency of a prefixed, equimolar nitrous oxide/oxygen mixture ([N.sub.2]O) on the reduction of patient discomfort induced by FB in adults.
MATERIALS AND METHODS
The protocol was approved by the local Ethics Committee (Comite de Protection des Personnes dans la Recherche Biomedicale), and signed informed consent was obtained from all participating patients before the procedure. Adult patients were recruited in the Lung Disease Department of a tertiary care hospital.
Patients were considered eligible for the study if they required FB for diagnostic purposes including BAL or bronchial biopsies. Patients were excluded if any of the following criteria were fulfilled: (1) absence of indication for BAL or bronchial biopsy leading to a FB duration too short to assess all parameters of patient stress; (2) respiratory failure as assessed by a FE[V.sub.1] < 1 L, FE[V.sub.1]/FVC ratio < 40%, and Pa[O.sub.2] < 60 mm Hg breathing room air; (3) low performance status; (4) inability to answer the questionnaire; (5) pregnant or breeding women; and (6) contraindication to nitrous oxide usage: cranial hypertension, unconsciousness, pneumothorax, and vitamin [B.sub.12] deficiency. (11,12)
Study Design and Measurements
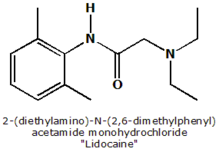
This prospective, phase III, randomized, double-blind, parallel-controlled, monocenter trial was conducted in the CHI of Creteil. Patients were included and randomized in two groups: the first group received prefixed, equimolar [N.sub.2]O (nitrous oxide group), and the second group received a prefixed equimolar nitrogen and oxygen mixture (control group). Gas mixtures were stocked in similar gas containers under a pressure of 170 bar, equivalent to 4 [m.sup.3] under a pressure of 1 bar at 15[degrees]C. A member of the department not involved in the endoscopy process was in charge of opening the randomization envelope. The same person was also in charge of selecting, setting up, and managing the gas container according to the randomization number. The container was connected to a facemask designed with a one-way valve for FB introduction. Gas flow was from 9 to 12 L/min. Administration of the gas started 3 min before the procedure and ended with the removal of the endoscope. All procedures were performed 10 min after local anesthesia similar in both groups and using 2% xylocaine nebulization in the oropharynx and nasal fossae and instillation on vocal cords and in the tracheobronchial tree not exceeding a total dose of 400 mg. Nasal introduction of the endoscope was the first approach. Three physicians participate in the study. The inclusion period extended from September 2000 to May 2002, a 21-month period.
The primary outcome was stress assessment using pulse rate and systemic BP (Critikon Dinamap; General Electric Medical Systems; Milwaukee, WI) at various time points: T0 = 5 min before the procedure, T1 = passing through the nose, T2 = passing through the trachea, T3 = during bronchial sampling, and T4 = 5 min after the end of the procedure. Secondary outcomes were as follows: (1) self-assessment of pain using a visual analog scale (VAS), where 0 = no discomfort and 100 = procedure not tolerable; (2) satisfaction as assessed by a questionnaire (Web site material). Both items were completed 30 min after the procedure.
Tolerance was also assessed on objective criteria such as transcutaneous oxygen saturation (Sp[O.sub.2]) [Nelleor Model NBP-40, Les Ulis, France], bronchospasm, bradycardia (heart rate < 60 beats/min), nausea, vomiting, and any other unusual clinical manifestation. Adverse events leading to the premature ending of the procedure were also noted (anxiety, confusion, consciousness alteration).
Statistical Analysis
The number of patients to include in this study had been estimated using a two-sided a of 5% and a [beta] risk of 10%. The hypothesis tested was that nitrous oxide treatment induces a reduction by 50% of the heart rate increase during FB. Under these assumptions, 120 patients per treatment group were necessary. As the rhythm of inclusions was slow, the trial was stopped earlier. Two hundred six patients were enrolled, resulting in a statistical power of 85%.
Results were analyzed with the intent-to-treat approach and expressed as mean [+ or -] SE for all quantitative parameters with the exception of the VAS. The distribution of this parameter did not follow a normal distribution; therefore, results were expressed as median and quartiles. Variations in pulse rate, BP, and Sp[O.sub.2] were analyzed using a analysis of variance (ANOVA) for repeated measurements.
For qualitative parameter comparisons, a [chi square] test was used. For quantitative parameters, a t test was used with the exception of VAS results, which were compared using a nonparametric Mann-Whitney U test. Data were analyzed using statistical software (Statistica; StatSoft; Tulsa, OK).
RESULTS
Two hundred six patients were included and equally distributed between both groups: 103 in the control group ([N.sub.2]) and 103 in the nitrous oxide ([N.sub.2]O) group. Patient characteristics and procedure conditions are shown in Table 1. There were no significant differences between the groups for patient characteristics, endoscopy conditions, sampling procedures, introduction route, procedure length (10.4 [+ or -] 4.4 min for all patients [[+ or -] SD]), and duration of gas inhalation (13.6 [+ or -] 4.2 min for all patients).
Primary Outcome
Hemodynamic Parameters: Effect of Time: As shown in Figure 1, pulse rate showed a significant change during the procedure (p < 0.00001). Significant changes were a decrease between T0 and T1, followed by a pulse rate increase for T2 that was sustained at T3 and returned to a value not different from baseline at T4. BP was significantly changed during the procedure (p < 0.05; Fig 2). BP increased from T0 to T2 and then decreased back to the baseline value at T4.
[FIGURES 1-2 OMITTED]
Hemodynamic Parameters: Effect of Treatment: Baseline values were similar in the two groups (Fig 1, 2). Nitrous oxide inhalation was associated with a significant reduction in BP increase between TO and T1 (significant interaction, p < 0.04). As shown in Figure 2, there was no significant change in BP in the nitrous oxide group, as opposed to a significant increase in patients receiving placebo (p = 0.003). No significant interaction was noted for changes in heart rate (Fig 1).
Secondary Outcomes
Self-Assessment: Among the 206 patients selected for the study, 1 patient was excluded for early withdrawal. The patient took off the mask at the beginning of the procedure (control group).
As assessed by the VAS, pain was lower in the [N.sub.2]O group (p = 0.02). The response for the questionnaire query "Would you accept another bronchial endoscopy under similar conditions?" did not show any differences between the two groups. Estimated duration of the procedure was similar in both groups and matched the real duration. Nose pain as well as cough were significantly reduced in the [N.sub.2]O group as compared to the control group (p = 0.04 for each item). Local anesthesia was equally tolerated in both groups. According to the questionnaire, the most uncomfortable period of the procedure was the moment of introduction of the bronchoscope. This discomfort time was reported less frequently in the nitrous oxide group but did not reach the level of significance. Results are reported in Table 2.
Tolerance: No significant change in Sp[O.sub.2] was noted during the procedure, and there was no effect of treatment (Fig 3). Desaturation episodes defined as a transient decrease of Sp[O.sub.2] > 4% were observed in 34 patients: 19 patients and 15 patients in the nitrous oxide and the control groups, respectively (Table 3). Transient bradycardia episodes defined as a pulse rate < 60 beats/min were noted in 8 patients in the placebo group and 15 patients in the nitrous oxide group (not significant [NS]) [Table 3].
[FIGURE 3 OMITTED]
Adverse Events: Adverse events (12) leading to the premature ending of the procedure were reported in 10 patients (Table 4). The most frequent side effect was anxiety in six eases (three patients in each group). Consciousness alterations were reported more frequently in nitrous oxide group. Two events were considered as severe: an anxiety episode in the placebo group, and a delirium episode in the nitrous oxide group.
DISCUSSION
In European countries, many ambulatory fiberoptic endoscopies are still performed after topical anesthesia only. This simplified approach without any premeditation is safe and results in decreased expenditures. (16) However the procedure of FB is associated with constant discomfort and sometimes with pain, particularly during nasal introduction of the fibroscope. Therefore, sedation is an essential part of the procedure to prevent pain and to alleviate discomfort, leading to better cooperation and optimal efficacy of the endoscopy. In a retrospective study, (13) IV sedation was reported in 50% of the procedures; however, this technique requires the use of hospital and anesthetic resources and is associated with a low but real morbidity and mortality. Moreover, IV sedation limits dynamic analysis of the airways such as vocal cords dynamics, presence of local or diffuse malacia, or effects of voluntary cough. Therefore, a risk/benefit approach comparing the same procedure performed under general or local anesthesia is indicated. Some authors (14,15) have proposed the systematic use of preoperative sedation by a benzodiazepine agonist such as diazepine or midazolain, but the effectiveness of these techniques remain controversial. (9,10,13,17-19) IV narcotics such as morphine and or fentanyl are not in routine use in some countries because, as in this ease, the presence of an anesthetist is required by regulations. Two questionnaire surveys (3,20) conducted in the United Kingdom emphasized large variations in the sedation procedures. Conscious sedation using inhalation of prefixed [N.sub.2]O/[O.sub.2] 50%/50% mixture is one of the simplest form of sedation available. Utilization of the equimolar mixture possesses many significant advantages over other pharmacosedation and can give an alternative method of sedation. The onset of action of inhalation sedation is rapid (3 to 4 min), and recovery time is usually complete 5 min following administration.
The analgesic and sedative pharmacologic properties of equimolar [N.sub.2]O have permitted its use in various settings because, as the mixture is without anesthetic effect, it does not require the presence of an anesthetist. (9,10) Inhalation of this gas for a sedative purpose is associated with very few side effects, resulting in a large set of indications, such as care for trauma, skin burns, or procedures such as lumbar puncture and sutures. These features of nitrous oxide are of interest to alleviate the anxiety and nasal pain that is associated with the nasal introduction of the fiberoptic bronchoscope. This pain relief approach is in agreement with current recommendations. (21,22) The present work as well as a previous publication (23) emphasizes this critical period of the procedure. However, pain management should not be limited to the use of analgesics. It has been shown that a clear evaluation of the patient before the procedure may significantly reduce the reported pain. (24) Moreover, the association of [N.sub.2]O with light preoperative sedation may be beneficial as a synergistic effect of both approaches. Hemodynamic changes are the most commonly assessed physiologic responses to stress. (25) BP and cardiac frequency (26-29) were the chosen parameters for stress evaluation in our study. Both parameters (BP and pulse rate) were increased during FB but returned to baseline values as soon as the procedure was finished. Administration of [N.sub.2]O resulted in a significant reduction of the BP swing observed at the beginning of the procedure. Regarding the VAS, the group receiving nitrous oxide expressed significantly higher satisfaction than the placebo group. Analysis of the satisfaction questionnaire also showed a significant reduction in nasal pain related to the introduction of the fibroscope and in cough reported during the procedure.
As previously reported in the literature, (11) [N.sub.2]O was associated with few and minimal adverse events in this trial, and the administration of the gas was well tolerated. Side effects were noted for two patients. One patients reported a severe but transient anxiety attack, and another patients had a short confusion episode. No significant differences were noted in Sp[O.sub.2] and bradycardia episodes in the nitrous oxide group comparing to the control group. As long-term and frequent administration of nitrous oxide may influence the health of the personnel working in operating rooms, safety procedures for gas scavenging should be used. (30) It appears to be useful to emphasize this recommendation for endoscopists and their staff who are working in the breathing zone of the patient, as they may be exposed to high levels of nitrous oxide concentrations.
In conclusion, the present study suggests that prefixed equimolar [N.sub.2]O results in enhanced comfort for the patient and may be an efficient sedation solution that is intermediate between topical anesthesia and general anesthesia for performing FB under good conditions without any serious side effects. This approach, already validated for FB in children, (31) should be extended in adult clinical practice. Criteria allowing a better selection of patients who should nevertheless undergo general anesthesia remain to be established.
REFERENCES
(1) British Thoracic Society guidelines on diagnostic flexible bronchoscopy. Thorax 2001; 56(suppl):i1-i21
(2) American Thoracic Society, Medical Section of the American Lung Association. Guidelines for fiberoptic bronchoscopy in adults. Am Rev Respir Dis 1987; 136:1066
(3) Smyth CM, Stead RJ. Survey of flexible fibrcoptic bronchoscopy in the United Kingdom. Eur Respir J 2002; 19:458-463
(4) Matot I, Kramer MR. Sedation in outpatient bronchoscopy. Respir Med 2000; 94:1145-1153
(5) Clarkson K, Power CK, O'Connell F, et al. A comparative evaluation of propofol and midazolam as sedative agents in fiberoptic bronchoscopy. Chest 1993; 104:1029-1031
(6) Crawford M, Pollock J, Anderson K, et al. Comparison of midazolam with propofol for sedation in outpatient bronchoscopy. Br J Anaesth 199.3; 70:419-422
(7) Randell T. Sedation for bronchofiberoscopy: comparison between propofol infusion and intravenous boluses of fentanyl and diazepam. Acta Anaesthesiol Stand 1992; 36:221-225
(8) Garcia J, Roure P, Hayem C, et al. Endoseopic bronchique sous anesthesie locale et douleur chez l'enfant: interet du melange protoxyde d'azote-oxygene. Rev Mal Respir 1998; 15:179-183
(9) Johnson JC, Atherton GL. Effectiveness of nitrous oxide in a rural EMS system. J Emerg Med 1991; 9:45-53
(10) Kerr F, Brown MG, Irving JB, et al. A double-blind trial of patient-controlled nitrous-oxide/oxygen analgesia in myocardial infarction. Lancet 1975; 1:1397-1400
(11) Gall O, Annequin D, Benoit G, et al. Adverse events of premixed nitrous oxide and oxygen for procedural sedation in children. Lancet 2001; 358:1514-1515
(12) Guttormsen AB, Refsum H, Ueland PM. The interaction between nitrous oxide and cobalamin: biochemical effects and clinical consequences. Acta Anaesthesiol Stand 1994; 38:753-756
(13) Colt HG, Morris JF. Fiberoptic bronchoscopy without pre-medication: a retrospective study. Chest 1990; 98:1327-1330
(14) Prakash UB, Offord KP, Stubbs SE. Bronchoscopy in North America: the ACCP survey. Chest 1991; 100:1668-1675
(15) Graham DR, Hay JG, Clague J, et al. Comparison of three different methods used to achieve local anesthesia for fiberoptic bronchoscopy. Chest 1992; 102:704-707
(16) Putinati S, Ballerin L, Corbetta L, et al. Patient satisfaction with conscious sedation for bronchoscopy. Chest 1999; 115: 14:37-1440
(17) Hatton MQ, Allen MB, Vathenen AS, et al. Does sedation help in fibreoptic brouchoscopy? BMJ 1994; 309:1206-1207
(18) Maltais F, Laberge F, Laviolette M. A randomized, double-blind, placebo-controlled study of lorazepam as premeditation for bronchoscopy. Chest 1996; 109:1195-1198
(19) Rees PJ, Hay JG, Webb JR. Premedication for fibreoptic bronchoscopy. Thorax 1983; 38:624-627
(20) Honeybourne D, Neumann CS. An audit of bronchoscopy practice in the United Kingdom: a survey of adherence to national guidelines. Thorax 1997; 52:709-713
(21) Diette GB, White P Jr, Terry P, et al. Quality assessment through patient self-report of symptoms prefiberoptic and postfiberoptic bronchoscopy. Chest 1998; 114:1446-1453
(22) Poi PJ, Chuah SY, Srinivas P, et al. Common fears of patients undergoing bronchoscopy. Eur Respir J 1998; 11:1147-1149
(23) Lechtzin N, Rubin HR, White P Jr, et al. Patient satisfaction with bronchoscopy. Am J Respir Crit Care Med 2002; 166:1326-1331
(24) Lechtzin N, Rubin HR, Jenckes M, et al. Predictors of pain control in patients undergoing flexible bronchoscopy. Am J Respir Crit Care Med 2000; 162:440-445
(25) Noble RE. Diagnosis of stress. Metabolism 2002; 51:37-39
(26) Meyer FU. Haemodynamic changes under emotional stress following a minor surgical procedure under local anaesthesia. Int J Oral Maxillofae Surg 1987; 16:688-694
(27) Paramaesvaran M, Kingon AM. Alterations in blood pressure and pulse rate in exodontia patients. Aust Dent J 1994; 39:282-286
(28) Sadahiro S, Noto T, Tajima T, et al. Fluctuation of blood pressure and pulse rate during colostomy irrigation. Dis Colon Rectum 1995; 38:615-618
(29) Yeragani VK. Heart rate and blood pressure variability: implications for psychiatric research. Neuropsychobiology 1995; 32:182-191
(30) Kanmura Y, Sakai J, Yoshinaka H, et al. Causes of nitrous oxide contamination in operating rooms. Anesthesiology 1999; 90:693-696
(31) Fauroux B, Onody P, Gall O, et al. The efficacy of premixed nitrous oxide and oxygen for fiberoptic bronchoscopy in pediatric patients: a randomized, double-blind, controlled study. Chest 2004; 125:315-321
This work was supported by a grant of Air Liquide Sante International.
Manuscript received January 27, 2005; revision accepted March 4, 2005.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal.org/misc/reprints.shtml).
Correspondence to: Kinan Atassi, MD, Centre Hospitalier Intercommunal, Service de Pneumologie, 40 avenue de Verdun, 940000 Creteil, France; e-mail: kinan.atassi@chicreteil.fr
* From the Service de Pneumologic et de Pathologie Professionnelle (Drs. Atassi, Mangiapan, Fuhrman, Lasry, and Housset), CHI de Creteil, Creteil; and Air Liquide Sante International (Dr. Onody), Paris, France.
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group