Patients over age 50 typically present with one chronic disease per decade. Each chronic disease usually requires long-term drug therapy, meaning most older patients require several drugs to control their conditions and/or maintain their health. Simultaneously, the use of complementary and alternative medications (CAM) has increased in the United States over the last 20 years, reaching 36% in 2002; herbal medicine use accounts for approximately 22% of all CAM use. Older adults often add herbal medicines to medications prescribed by their physicians, yet do not always inform the physician. The drug metabolizing enzyme systems process all compounds foreign to the body including prescription drugs and herbal medications. Therefore use of both medicinals simultaneously has a potential for interactions of an adverse nature. This review, which will discuss kava, is one in a series covering the documented interactions between herbal medicines with proven efficacy and prescription drugs.
Bressler R. Herb-drug interactions: Interactions between Kava and prescription medications. Geriatrics 2005; 60(September):24-5.
Key words: herbal interactions * complementary and alternative medications * kava
**********
The use of herbal medications has been steadily increasing. From 1990 to 1997, use of self-prescribed herbal medications increased from 2.5% to 12%, and people consulting herbal medicine practitioners increased from 10.2% to 15.1%. (1-4)
Herbal medicines include dietary supplements that contain herbs, either singly or in mixtures. Also called botanicals, herbal medicines are plants or plant parts used for their scent, flavor, and/or therapeutic properties. Since herbal medicines are classified as dietary supplements, there are no Food and Drug Administration (FDA) regulations regarding accuracy of active ingredients content or efficacy and safety of active ingredients. (2)
The focus of health care in older patients is control of chronic diseases: Older adults typically manifest one chronic disease for each decade past 50. The most common chronic diseases are coronary artery disease, hypertension, diabetes mellitus, degenerative arthritides, depression, and cancers. Most chronic diseases are treated with multiple drug therapy. (5) The average older adult takes 5 prescriptions each day.
The addition of herbal medicines to a program of multiple drug therapy holds the potential for herb-drug interactions. (6,7) The lack of quantitative data on herbal medications, however, makes it difficult to predict the potential for interactions with prescription and over-the-counter drugs.
The seven herbal medicines most sold in the United States are (8)
1. Ginkgo biloba
2. St. John's Wort
3. Ginseng
4. Kava
5. Saw Palmetto
6. Garlic
7. Echinacea.
Efficacy information and drug interaction data is available for the first five. (8) Efficacy claims for garlic and echinacea are not supported in the literature. (1,2,6) This article, the fourth in a series (See April 2005 issue for article on ginkgo biloba, July 2005 issue for article on St. John's wort, and August 2005 issue for article on ginseng), will discuss specific proven efficacies and, where known, the mechanisms of action for kava. The final article in the series will discuss saw palmetto. Documented drug-herb interactions will be presented.
Kava (Piper methysticum)
Kava, an extract of the dried root of the pepper plant, is widely used as a sedative, anxiolytic, (8) and sleep aid. (9)
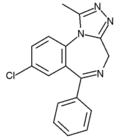
Pharmacologic actions. Kava's anxiolytic activity has been demonstrated in studies and its mechanism of action postulated. (9,10) Kava is thought to enhance gamma-amino-butyric acid binding at its CNS receptors, (9) and therefore its sedative-anxiolytic activity would be an indirect one. Its actions are similar to those of the benzodiazepines, which bind GABA receptors.
Naloxone inhibits morphine-induced analgesia but is ineffective in reversing kava's antinociceptive activities, showing that the analgesia produced by kava occurs via a nonopiate pathway. Kava may possess other CNS pharmacologic properties that affect sleep and anxiety. (9)
Dosage and administration. Dosage of kava lactones in clinical studies ranged from 100 mg/d to 200 mg/d. (8)
Contraindications. Patients with liver problems should take particular care in using kava. Kava users should notify their doctor immediately if they experience symptoms of liver disease (eg, yellowing of skin or eyes, dark urine). (8)
Adverse effects/toxicology. Alcohol consumption increases kava toxicity. (8) Patients may experience dry, flaking, discolored skin; scaly rash; red eyes; visual disturbance; blood cell abnormalities; liver damage (mild to severe); blood in urine; pulmonary hypotension; puffy face; and muscle weakness. (8) Kava produces mild euphoric changes characterized by happiness, fluent and lively speech, and increased sensitivity to sounds. High doses may also lead to muscle weakness. Visual or auditory changes may occur, as shown by reduced near point of accommodation and convergence, an increase in pupil diameter, and oculomotor balance disturbances. (8)
Ethanol increases the toxicity of kava. (8) This interaction may be of important clinical and social consequence if the two are taken concomitantly.
Reported drug interactions are detailed in the table.
Conclusion
Physicians are reminded to ask their patients about any herbal and dietary supplements that they might be taking. It might help to have patients fill out a chart to keep on file that lists this information, including the frequency and reasons for using supplements. Refer to the chart at www.geri.com. (Log onto www.geri.com, scroll down the left hand navigation bar to Patient Handout and print out the "Tracking your meds" handout to help patients understand the information they need to provide physicians regarding the dietary supplements they take.)
References
(1.) Ang-Lee MK, Moss MK, Yuan CS. Herbal medicines and perioperative care. JAMA 2001; 286(2):208-16.
(2.) Ernst E, Pittler MH. Herbal medicine. Med Clin North Am 2002; 86(1):149-61.
(3.) Astin, JA. Why patients use alternative medicine: Results of a national study. JAMA 1998: 279(19):1548-53.
(4.) Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States. Prevalence, costs, and patterns of use. N Engl J Med 1993; 328(4)246-52.
(5.) Bressler R, Bahl JJ. Principles of drug therapy for the elderly patient. Mayo Clin Proc 2003: 78(12):1564-77.
(6.) Ernst E. The risk-benefit profile of commonly used herbal therapies: Ginkgo, St. John's wort, ginseng, echinacea, saw palmetto, and kava. Ann Intern Med 2002; 136(1):42-53.
(7.) Miller LG. Herbal medicinals: Selected clinical considerations focusing on known or potential drug-herb interactions. Arch Intern Med 1998; 158(20):2200-11.
(8.) David S. Tatro, ed. Drug interaction facts: Herbal supplements and food. St. Louis, MO; Facts and Comparisons, A. Walters Kluwer Company; 2004. Also available online at: www.factsandcomparisons.com.
(9.) Wheatley D. Kava and valerian in the treatment of stress-induced insomnia. Phytother Res 2001; 15(6):549-51.
(10.) Pittler MH, Ernst E. Efficacy of kava extract for treating anxiety: Synthetic review and net-analysis. J Clin Psychopharmacol 2000; 20(1):84-9.
Dr. Bressler is professor of medicine and pharmacology, University of Arizona Health Sciences Center and the Sarver Heart Center, Tucson, and serves on the Geriatrics Editorial Advisory Board.
Disclosure Dr. Bressler's works are supported by the Sarver Heart Center and the Brach Foundation.
COPYRIGHT 2005 Advanstar Communications, Inc.
COPYRIGHT 2005 Gale Group