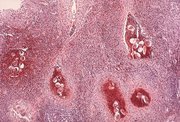
A 27-year-old woman was found to have a low-grade squamous intraepithelial lesion and koilocytic changes consistent with human papillomavirus infection on routine Papanicolaou test. She had lived in rural Senegal (West Africa) all her life, until she moved to the United States 3 years earlier. She recalled swimming in lakes while living in Senegal, but reported no history of abnormal bleeding of the cervix, in her urine, or per rectum. Biopsy of the cervix revealed moderate dysplasia involving the endocervical glands, squamous metaplasia, and severe acute and chronic cervicitis. Calcified eggs were present in the stroma (Figure 1, hematoxylin-eosin, original magnification ×20, after decalcification). These eggs were present throughout the cervical stroma and were not associated with any granulomatous reaction (Figure 2, hematoxylin-eosin, original magnification ×52, after decalcification). The eggs were nonoperculated and had a prominent terminal spine (Figure 3, hematoxylin-eosin, original magnification ×200, after decalcification). She was treated with praziquantel, 1800 mg twice daily for 1 day. No follow-up information was available at 7 months post-treatment.
The species most commonly implicated in female genital schistosomiasis is Schistosoma hematobium (other species that produce human disease are Schistosoma mansoni and Schistosoma japonicum). The cervix is the most commonly affected female genital site. Other less commonly affected sites include the ovary, clitoris, and fallopian tube, in that order.1 Functional disturbances that have been described in women with genital tract schistosomiasis include menstrual irregularities, pelvic pain, chronic cervicitis, spontaneous abortion, and infertility. The involved cervix may be irregularly shaped and eroded, and it may bleed easily. Granulomatous inflammatory reaction to the ova is a common histologie finding, and dense fibrosis is usually found at later stages of the disease. The moderate dysplasia seen in this case was probably due to the coexistence of human papillomavirus infection, since no cause-effect relationship has been described between cervical intraepithelial neoplasia and schistosomiasis of the cervix.
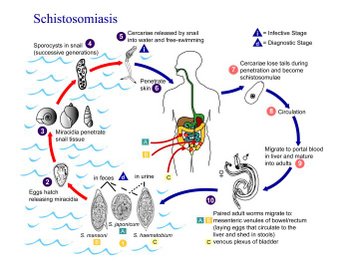
Prevalence of the disease depends on the presence of a susceptible intermediate snail host and fecal contamination of water supplies. Human infection occurs after the skin is penetrated by cercariae, the infective form of the parasite that is liberated into fresh water by the intermediate snail host (Figure 4, schematic representation of the life cycle of Schistosoma). After penetrating the skin, they shed their tails to become schistosomula, which travel through the venous circulation to the liver (via the lungs), where the adult worms mature. They then migrate along the portal vein to the mesenteric venules, where they produce large numbers of eggs. Subsequently, they invade various tissues from this location. The eggs return to the environment via feces or urine. The larvae develop inside the eggs but do not hatch until their arrival in fresh water, when they invade the snail host. The larvae inside the snail host produce several thousands of cercariae. Clinical manifestations of schistosomiasis result from an immunologie reaction on the part of the human host and represent type IV hypersensitivity.
Methods of detection of schistosome eggs in cervical tissue include cytologic examination of a cervical smear, histologie examination of a cervical biopsy, and direct examination of cervical tissue obtained by forceps biopsy. It has been suggested that direct examination of cervical tissue is the diagnostic test of choice.2
The drug of choice for treatment is praziquantel, but other drugs, such as oxamniquine and metrifonate, are also effective.
References
1. Gouzouv A, Baldassini B, Opa JF. Anatomicopathological aspects of genital bilharziasis in women. Med Trop. 1984;44:331-337.
2. Poggensee G, Sahebali S, Van Marck E, Swai B, Krantz I, Feldmeier H. Diagnosis of genital cervical schistosomiasis: comparison of cytological, histopathological and parasitological examination. Am J Trop Med Hyg. 2001;65:233-236.
Adebowale Adeniran, MD; Haytham Dimashkieh, MD; Yuri Nikiforov, MD, PhD
Accepted for publication July 30, 2003.
From the Department of Pathology and Laboratory Medicine, University of Cincinnati, Cincinnati, Ohio.
Reprints: Yuri Nikiforov, MD, PhD, Department of Pathology and Laboratory Medicine, University of Cincinnati, 231 Albert Sabin Way, Cincinnati, OH 45267-0529 (e-mail: yuri.nikitorov@uc.edu).
Copyright College of American Pathologists Dec 2003
Provided by ProQuest Information and Learning Company. All rights Reserved