The purpose of this study was to determine the impact of health education intervention on the perception and prevalence of urinary schistosomiasis among school children in endemic rural communities in Cameroon. The rapid assessment technique method was used to determine the prevalence of Schistosoma heamatobium infection in Gounougou (experiment 1), Ouro-Doukoudje (experiment 2), and Lagdo (control). There was a positive correlation between the questionnaire approach, the biochemical testing, and ova detection rate (r dispersed between 0.98 and 1.00). In the first phase of the study, after collection of the baseline data, school children of the experimental villages received health education. Unlike in Gounougou where children were given a predesigned control procedure, those in Ouro-Doukoudje were asked to design their own control procedure under the supervision of the investigators. A second investigation conducted eight months after the end of the first intervention showed a significant drop of prevalence in Gounougou (53.2% vs 29.6%, p 0.25). It also showed a significant increase of the awareness in Gounougou (14.5% vs 94.7%, p 10); with the greater increase in Ouro-Doukoudje (94.0%) as compared to Gounougou (80.2%, p
INDEX TERMS: Health education, urinary schistosomiasis.
Clin Lab Sci 2003;16(3):137
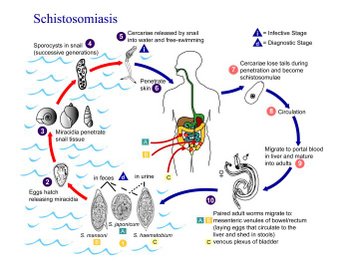
Schistosomiasis is one of the most widespread of all human parasitic diseases, affecting over 200 million people in more than 74 countries.1 It is the most prevalent of water-borne diseases and a great health risk in rural areas of developing countries.2
Although schistosomiasis is not the most serious of diseases in the tropics, compared to malaria, diarrhea, acute respiratory infections, or malnutrition, it is widespread, particularly in young populations, and its chronicity has made it difficult to determine the impact on overall morbidity and mortality in endemic areas.3
Schistosomiasis, like the majority of the parasitic diseases, is influenced: 1) by human behaviour, mainly water use practices and indiscriminate urination and defecation, and 2) by failure to take advantage of available screening services or to comply with medical treatment.
In schistosomiasis, like in many other parasitic diseases, the aim of health education is: 1) to help people understand that their own behaviour is a key factor in the transmission of the disease, and 2) to find a common ground between traditional beliefs and practices, and modern scientific knowledge and methods.
In this study, social science principles were used to determine the impact of health education on the perception and prevalence of urinary schistosomiasis among school children in three rural communities in Cameroon.
MATERIALS AND METHODS
Study area and subjects
The study was conducted from September 2000 to June 2001 in the North Province of Cameroon in an area known as Lagdo dam region, where 20 years ago, an artificial lake was created by the construction of a dam on the river Benoue, in Lagdo village. The three villages targeted in this study (Lagdo, Gounougou, and Ouro-Doukoudje) are all situated around the lake, about 60 km from each other. The three villages are typical rural African communities. There is no pipe-borne water, electricity, or drainage system. The residents rely wholly on water from the artificial lake for their economic and domestic needs.
Phases of the study
Phase 1
Collection of samples
Urine samples were collected into clean universal containers. Samples were collected from school pupils between 5 and 19 years of age. Pupils were requested to exercise by running to increase the chances of recovery of ova from urine. Samples were collected between 12:00 (noon) and 2:00 P.M. when maximum egg excretion occurs.4
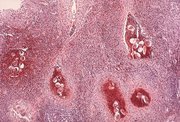
Detection of hematuria and ova
Hematuria was detected soon after collection in the field using dipsticks (Ames, Bayer Diagnostic, Brussels, Belgium). The results were read immediately and recorded. Thereafter, five mL of sample was transferred into a clean universal container holding 1% aqueous solution of carbol fuchsin for staining and preservation of ova. Filtration of samples was done using Whatman No 1 filter paper as described by Ejezie.5 Examination for the ova of Schistosoma haematobium was done using a light microscope with the 10X objective.
Health education intervention strategy
Health education intervention was utilized in Gounougou (experiment 1) and Ouro-Doukoudje (experiment 2), and was aimed at promoting and reinforcing health behaviour. The basic messages communicated were: what schistosomiasis is, how the disease is acquired, what the signs and symptoms of the disease are, and what can be done about it.
Health education method
In Gounougou, school children were given predesigned criteria and procedures for implementation for the control of schistosomiasis. In Ouro-Doukoudje children were asked to design a method for control of schistosomiasis in their village. Under the supervision of the investigators, one of the proposed methods was selected for implementation. In Lagdo (control) only the base data were collected.
Phase 2
This phase was conducted eight months after the end of the first intervention and consisted of the collection of samples and detection of hematuria and ova.
Data analysis
Chi-square, student-t-test, and Pearson's product moment correlation were used to test for the significance of the results.
RESULTS
Table 1 shows the prevalence of Schistosoma haematobium infection and hematuria among school children in Gounougou, Ouro-Doukoudje, and Lagdo, according to age, before and after health education intervention. It was observed that in Gounougou (experiment 1) and Ouro-Doukoudje (experiment 2), where health education strategies were implemented, there was a significant drop in the prevalence (53.2% vs 29.6%, p
Table 2 shows the validation of children's questionnaires with biochemical and parasitological techniques in Gounougou, Ouro-Doukoudje, and Lagdo. There appeared to be a strong positive correlation between the questionnaire approach and the biochemical and parasitological techniques (r dispersed between 0.99 and 1.0).
Table 3 depicts the perception of urinary schistosomiasis before and after health education in Gounougou, Ouro-Doukoudje, and Lagdo. There was a significant increase in awareness in Gounougou (14.5% vs 94.7%, p
DISCUSSION
The purpose of this study was to determine the impact of health education on the perception and prevalence of urinary schistosomiasis. Previous studies had emphasized the limits of epidemiological and control studies based only on children in school.6,7 In most rural communities of Sub-Saharan Africa, only about 68% of children go to school and females are generally marginalized.8,9
The study was targeted at school children as they are most of the heavily infected individuals in the community, and are at risk of developing severe disease.10,13 School children are likely to contribute most to transmission and they are readily accessible through the framework of school.14 Furthermore, it is believed that school children are more receptive to health education and can easily spread the message within the community.15
Comparing among school children the prevalence of urinary schistosomiasis obtained during the first and second phases of the study, it was observed in Gounougou (experiment 1) and Ouro-Doukoudje (experiment 2), where the strategies of the health education were implemented, there was a significant drop in the prevalence of urinary schistosomiasis. On the other hand there was no significant change in the prevalence of urinary schistosomiasis in Lagdo, the control village in which no health education strategy was implemented. The significant change in prevalence observed in Gounougou and Ouro-Doukoudje can not be attributed to social or seasonal variation; the three villages share the same social, geographical, and climatic features.16 Only health education applied in the experimental villages could have accounted for the observed prevalence decrease.
The comparison of the prevalence of urinary schistosomiasis according to age in the three villages under study indicates that more children between 10 and 14 years of age were receptive to health education in the experimental villages. It is believed that the majority of these children who were either at the end of the primary education or in the secondary school had a better understanding than the younger ones (5 to 9 years). On the contrary, children of the 15 to 19 age group, even though more educated, did not perceive urinary schistosomiasis as a serious problem, probably for one of the following reasons: 1) It is now accepted that effective resistance to infection/ re-infection develops after 5 to 15 years of exposure.17 It follows that the worm burden may be milder in older children, so they found no reason for visiting the health centre of their locality, even after health education. 2) the majority of children aged between 15 to 19 years of age might have been hosting the parasite for many years, and thus did not look upon blood in urine as a cause of worry. They regrettably rejected health education and consequently refused to visit the health centre.
The validation of children's questionnaires with biochemical and parasitological techniques (Table 2) showed a strong positive correlation between the questionnaire approach and other techniques (r = 0.99). These findings support the use of reagent strips and questionnaires to screen in areas with high risk of urinary schistosomiasis as earlier proposed by Lengeler.18 Thus, instead of spending many resources in carrying out definitive diagnosis before mass treatment of school children in schistosomiasis endemic areas, a simple questionnaire administered to these children, along with biochemical testing, could be used as a diagnostic method.
The strong negative correlation between the perception and the prevalence of urinary schistosomiasis in Gounougou (experiment 1) and Ouro-Doukoudje (experiment 2) indicates that the prevalence (in percentage of infected subjects) was inversely proportional to the awareness. In other words, ignorance of the cause of urinary schistosomiasis is strongly related to its prevalence. This is explained by the fact that, children who are conversant with the knowledge of the disease are more aware of the consequences of many attitudes and practices than those who have not been exposed to such an opportunity. It follows that through health education, a child is exposed to health ideals which enhance the promotion of his physical, social, and psychological health throughout life. It is therefore important to select appropriate strategies, if health education is to be successful, for addressing the factors contributing to behaviour that influences health.2
The present study has shown that the strategy applied in Ouro-Doukoudje (experiment 2) and proposed by school children (under our supervision) yielded a greater increase of awareness than the strategy applied in Gounougou, which was predesigned by the investigators. This observation is consistent with WHO recommendations that if health education is to be effective, it must encourage participation of the target population as full partners in planning.2
It is therefore recommended that health education through the framework of school be adopted as a national policy for urinary schistosomiasis control programs. The strategy of this policy should be planned with school children as full partners, provided they receive appropriate orientation.
This paper was accepted for oral presentation at IAMLTASCLS World Congress 2002 in Orlando, Florida USA.
REFERENCES
1. World Health Organization. The control of schistosomiasis. Tech Rep Ser WId Hth Org 1985;3:6,7.
2. World Health Organization. Health education in the control of schistosomiasis. Tech Rep Ser Wld Hth Org 1990;WC 810.
3. Mott KE, (1983). A reusable polyamide filter for diagnoses of Schistosoma haematobium infection by urine filtration. Bull de la Soc de Pathol Exotique 1983;76:101-4.
4. Chen MG, Mott KE. Progress in assessment due to schistosomiasis. Trop Dis Bull 1989;86:1-56.
5. Ejezie GC Ade-Serrano MO. Schistosoma haematobium in Ajara community of Badagry Nigeria. A study on prevalence, intensity and morbidity from infection among primary school children. Trop Geog Med1981;37:175-0.
6. Useh MF Ejezie GC. Prevalence and morbidity of Schistosoma haematobium infection in Adim community of Nigeria. Nigerian J Med Lab Sci 1996;5:17-28.
7. Useh MF, Ejezie GC. School-based schistosomiasis control programs: a comparative study on the prevalence and intensity of urinary schistosomiasis among Nigerian school-age children in and out of school. Trans Roy SocTrop Med Hyg 1999;93:1-5.
8. UNESCO (United Nations Educational Scientific and Cultural Organisation) (1993). World Education Report 1993.UNESCO.
9. Csapo M. Religious, social and economic factors hindering the education of girls in northern Nigeria. Comparative education 1981;3:121-9.
10. Anderson RM, May RM. Herd immunity to helminth infection and implications to parasitic control, Nature London 1985;315:493-6.
11. Anderson RM, May RM. Herd immunity to helminth: mathematical models. Population dynamics and control. Adv Parasitol 1985;24:1-101.
12. Anderson RM, Medley GE Community control of helminth infections of man by mass and selective chemotherapy. Parasitol 1985;90:629-60.
13. Butterworth AE, Sturrock RF, Ouma JH, and others. Comparison of different chemotherapy strategies against Schistosoma mansoni in Machakos Districk, Kenya: effects on human infection and morbidity. Parasitol 1991;103.339-45.
14. Ouma JH. (1987). Transmission of Schistosoma mansoni in an endemic area of Kenya with special reference of the role of human defecations behaviour and sanitary practices. PhD thesis, University of Liverpool, UK.
15. Somerset HCA. Child-to-Child. A questionnaire review and studies of projects in three countries. Institute of Education, University of London. 1988.
16. MEAVSB (Mission d'Etude et d'Amenagement de la vallee Superieure de la Benoue). Suggestions pour le mise en valeur des mares de Gounougou et Djanga. Haskoning, MEAVSB, 1989. Univ. Leyde.
17. Hogan P. Immunity and morbidity in infection due to Schistosoma haematobium. Am J Trop Med Hyg 1996;55(5),116-20.
18. Lengeler C, Desavingny D, Mshinda H, and others. Community-based questionnaires and health statistics as tools for the cost-effective identification of communities at risk of urinary schistosomiasis. Int J Epidemiol 1991;20:796-807.
Address for correspondence: Dr Kamga Fouamno Henri Lucien, Faculty of Health Sciences, University of Buea-Republic of Cameroon, (+237) 7769464. henrikamga@alooh.com.
Copyright American Society for Clinical Laboratory Science Summer 2003
Provided by ProQuest Information and Learning Company. All rights Reserved