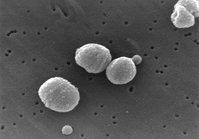
The severe acute respiratory syndrome (SARS) is caused by a novel coronavirus (SARS-CoV) with great genetic diversity among strains. (1,2) Coronaviruses are single-stranded RNA viruses that can cause common cold in humans and diseases in animals. The SARS-CoV is moderately infective, with an attack rate that ranges from 2.4 to 31 cases per 1,000 exposure hours (3) and may be transmitted by aerosolization. The SARS epidemic affected thousands of people in five continents (26 countries) over a period of 9 months following its first appearance in November of 2002 in the south of China. The case fatality rate associated with SARS is about 15%. However, a higher mortality occurs in the elderly and in patients with comorbid conditions. (4)
The clinical presentation of patients with SARS ranges from asymptomatic infection to severe multi-lobar pneumonia and death. Of the symptomatic patients, approximately 20 to 25% become critically ill and need to be admitted to the ICU, most commonly with acute respiratory failure that fulfills the criteria for acute lung injury (ALI) and ARDS. (5,6) The initial chest radiographic finding in patients with SARS, unifocal peripheral airspace disease, is nonspecific and has significant overlap with the radiographic findings of other atypical pneumonias. (7,8) Progression to bilateral disease is associated with poor outcomes. (7,8) Patients with ALI/ARDS (bilateral diffuse infiltrates and severe hypoxemia) have diffuse alveolar damage (9) that may look similar to diffuse alveolar damage present in most patients with ARDS. (10)
In this issue of CHEST (see page 1393), Ong et al (11) report the pulmonary function and health status at 1 year of a cohort of patients from Singapore who recovered from SARS. There were 206 patients with probable SARS in Singapore, 15% of whom died (32 patients). Of the patients who survived, 46% declined participation, could not be contacted, were underage, or could not perform the battery of tests. The 94 subjects included in this study (half of them were health-care workers) had pulmonary function tests done and the authors administered the St. George's Respiratory Questionnaire. Unfortunately, exercise testing was not performed. Ong et al (11) found that at 1 year, 20 to 30% of the patients had cough, sputum production, or shortness of breath, but the mean values for lung volumes were in the normal range. According to the American Thoracic Society criteria, mild and moderate impairment were present in 32% and 5%, respectively. Only 12% of the study population required admission to the ICUs for severe acute respiratory failure, and only 7% were intubated. Interestingly, the outcomes of the patients with severe respiratory failure were similar to the patients who were not admitted to the ICU. Overall, however, patients who survived SARS had worse health-related quality of life than normal subjects.
This new study by Ong et al (11) extends the observation regarding lung function done at 3 months (12) and at 6 months from hospital discharge, (13) and complements a recent study (14) from Beijing that followed up patients 1 year after SARS. All of these studies (12-14) report common abnormalities in pulmonary function tests, but most if not all of the abnormalities were mild. It is important to emphasize that in a previous communication by Ong et al, (12) in patients evaluated at 3 months after SARS, up to 78% patients had mild-to-moderate impairment of exercise capacity, although none of the patients showed ventilatory impairment during exercise. The limitations during exercise in this group may be related to poor conditioning or residual muscular problems. An important limitation of the current study is the lack of exercise test results, as we do not know the real impact of the alterations present in the breathing tests and in the health-related quality of life questionnaire.
It is important to notice the similarities and differences between the current report by Ong et al (11) and the reported physiologic and health-related quality of life abnormalities in survivors of ARDS and pneumonia. (15-18) In both SARS and ARDS, (15,18) recovery of lung function in survivors is impressive considering the extent of the original injury. However, patients who survive ARDS have significant decrease in health-related quality of life when compared with matched control subjects with sepsis and trauma but without ARDS. (16) It seems that patients with SARS have a more benign course compared with patients with ARDS and pneumonia in terms of health-related quality of life.
What are the lessons learned over the last 28 months? The first one is how vulnerable the human race is when we are faced with new diseases and lack immunity to new pathogens. However, the medical community has been able to work together and share new findings and new knowledge, to control the epidemic of SARS of from 2002 to 2003. Coordination of medical personnel with administrative and political authorities, rapid actions, sound public health policy, and use of infection control procedures are essentials in tackling major epidemics. (19)
What is going to be the new epidemic/pandemic affecting us in the next few months or years? Could it be SARS again? Or avian influenza (H5N1 strain of influenza A), (20,21) a virus with a major potential of causing pandemic? Whatever it is, the medical community needs to remain vigilant and generate knowledge that will limit the impact of the disease, as has been the case with SARS.
REFERENCES
(1) Guan Y, Peiris JS, Zheng B, et al. Molecular epidemiology of the novel coronavirus that causes severe acute respiratory syndrome. Lancet 2004; 363:99-104
(2) Peiris JSM, Lai St, Poon L, et al. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet 2003; 361:1319-1325
(3) Varia M, Wilson S, Sarwal S, et al. Investigation of a nosocomial outbreak of sever acute respiratory syndrome (SARS) in Toronto, Canada. Can Med Assoc J 2003; 169:285-292
(4) Anderson RM, Fraser C, Ghani AC, et al. Epidemiology, transmission dynamics and control of SARS: the 2002-2003 epidemic. Philos Trans R Soc Lond B Biol Sci 2004; 359: 1091-1105
(5) Fowler RA, Lapinsky SE, Hallet D, et al. Critically ill patients with severe acute respiratory syndrome. JAMA 2003; 290: 367-373
(6) Lew TWK, Kwek TK, Tai D, et al. Acute respiratory distress syndrome in critically ill patients with severe acute respiratory syndrome. JAMA 2003; 290:374-380
(7) Lai EK, Deif H, LaMere EA, et al. Severe acute respiratory syndrome: quantitative assessment from chest radiographs with clinical and prognostic correlation. AJR Am J Roentgenol 2005; 184:255-263
(8) Chau TN, Lee P, Choi K, et al. Value of initial chest radiographs for predicting clinical outcomes in patients with severe acute respiratory syndrome. Am J Med 2004; 117:249-254
(9) Cheung OY, Chan JWM, Ng CK, et al. The spectrum of pathological changes in severe acute respiratory syndrome (SARS). Histopathology 2004; 45:119-124
(10) Esteban A, Fernandez-Segoviano P, Frutos-Vivar F, et al. Comparison of clinical criteria for the acute respiratory distress syndrome with autopsy findings. Ann Intern Med 2004; 141:440-445
(11) Ong KC, Ng AW, Lee LSU, et al. 1-year pulmonary function and health status in survivors of severe acute respiratory syndrome. Chest 2005; 128:1393-1400
(12) Ong KC, Ng AW, Lee LSU, et al. Pulmonary function and exercise capacity in survivors of severe acute respiratory syndrome. Eur Respir J 2004; 24:436-442
(13) Ng CK, Chan JWM, Kwan TL, et al. Six month radiological and physiological outcomes in severe acute respiratory syndrome (SARS) survivors. Thorax 2004; 59:889-891
(14) Xie L, Liu Y, Fan B, et al. Dynamic changes of serum SARS-coronavirus IgG, pulmonary function and radiography in patients recovering from SARS after hospital discharge [abstract]. Respir Res 2005; 6:5
(15) Orme J, Romney JS, Hopkins RO, et al. Pulmonary function and health-related quality of life in survivors of acute respiratory distress syndrome. Am J Respir Crit Care Med 2003; 167:690-694
(16) Davidson TA, Caldwell ES, Curtis JR, et al. Reduced quality of life in survivors of acute respiratory distress syndrome compared with critically ill control patients. JAMA 1999; 281:354-360
(17) Laitinen LA, Miettinen AK, Kuosma E, et al. Lung function impairment following mycoplasmal and other acute pneumonias. Eur Respir J 1992; 5:670-674
(18) Herridge MS, Cheung AM, Tansey CM, et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med 2003; 348:683-693
(19) Christian MD, Poutanen SM, Loutfy MR, et al. Severe acute respiratory syndrome. Clin Infect Dis 2004; 38:1420-1427
(20) Monto AS. The threat of an avian influenza pandemic. N Engl J Med 2005; 352:323-325
(21) Ungchusak K, Auewarakul P, Dowell SF, et al. Probable person-to-person transmission of avian influenza A (H5N1). N Engl J Med 2005; 352:333-340
Alejandro C. Arroliga, MD
Enrique Diaz-Guzman, MD
Herbert P. Wiedemann, MD
Cleveland Clinic Foundation
Cleveland OH
Dr. Arroliga is Professor of Medicine, Cleveland Clinic Lerner College of Medicine, and Head, Section of Critical Care Medicine.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml).
Correspondence to: Alejandro C. Arroliga, MD, Cleveland Clinic Lerner College of Medicine, Section of Critical Care Medicine, 9500 Euclid-Ave, G6-156, Cleveland, OH 44195; e-mail: arrolia@ccf.org
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group