Study objectives: To characterize the long-term pulmonary function and health status in a prospectively identified cohort of patients who survived the severe acute respiratory syndrome (SARS).
Design: Prospective follow-up cohort study.
Setting: University-affiliated hospital.
Patients: Ninety-four patients who recovered from SARS were assessed at a uniform time point of 1 year after hospital discharge.
Measurements: The study included the measurement of static and dynamic lung volumes, the determination of the diffusing capacity of the lung for carbon monoxide (DLCO), and a health status evaluation using the St. George Respiratory Questionnaire (SCRQ).
Results: Eleven patients (12%) had mild impairment of FVC, 20 (21%) had mild impairment of FE[V.sub.1], 5 (5%) had mild impairment of the FE[V.sub.1]/FVC ratio, and 17 (18%) had mild impairment of the DLCO. There was one patient (1%) who had moderate impairment of FVC, one patient (1%) who had moderate impairment of the FE[V.sub.1]/FVC ratio, and three patients (3%) who had moderate impairment of the DLCO. No pulmonary function abnormalities were detected in 59 patients (63%). Mean scores were significantly higher (ie, worse) than the population norms in the activity (p < 0.001), impacts (p < 0.001), and total (p < 0.001) domains of the SGRQ.
Conclusions: One year after recovery from SARS, persistent pulmonary function impairment was found in about one third of patients. The health status of SARS survivors was also significantly worse compared with the healthy population. The main determinants of morbidity in recovered SARS patients need to be further defined.
Key words: follow-up studies; outcome assessment; pneumonia; respiratory, impairment
Abbreviations: ATS = American Thoracic Society; CoV = coronavirus; DLCO = diffusing capacity of the lung for carbon monoxide; FI[O.sub.2] = fraction of inspired oxygen; LDH = lactate dehydrogenase; SARS = severe acute respiratory syndrome; SGRQ = St. George respiratory questionnaire; TLC = total lung capacity
**********
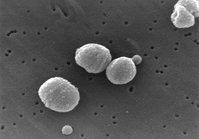
The severe acute respiratory syndrome (SARS) is a recently described condition caused by infection with a coronavirus (CoV) (1) and is characterized by both an atypical pneumonia and efficient nosocomial transmission.
First recognized in March 2003, SARS spread across the globe, caused many major outbreaks, and had an overall mortality rate of 11% (2) but was successfully contained in < 4 months. Although it has been > 1 year since the illness was successfully contained, published data on the condition of those who survived the illness are limited. Several studies (3-9) have reported persistent symptoms, as well as radiologic and functional abnormalities during follow-up several weeks or months after hospital discharge, but the prevalence and severity of the longterm sequelae of SARS remain largely unknown. Because lung function is known to improve for up to 1 year after discharge from the hospital in survivors of other causes of acute lung injury, (10,11) it is imperative that long-term studies of SARS survivors be conducted in order to determine the persistence of abnormalities in pulmonary function, and whether these abnormalities contribute to permanent impairment and disability. As the majority of patients with SARS survive the illness (2) and medical personnel, physicians, nurses, and hospital workers are among those commonly infected in most countries, (2) an additional requisite for the identification and quantification of morbidity among survivors may be for the consideration of awarding compensation.
The purpose of this study was to characterize the long-term pulmonary function and health status in a prospectively identified cohort of patients who survived SARS in Singapore.
MATERIALS AND METHODS
Patient Selection
There were 206 cases of SARS in Singapore reported to the World Health Organization as of June 26, 2003. (12) According to the World Health Organization case definition, probable SARS was diagnosed in all of these patients, (13) and they were admitted to a single hospital (Tan Tock Seng Hospital). Survivors at 1 year after hospital discharge were eligible for enrollment in the study if they were [greater than or equal to] 21 years of age. Patients were excluded from the study if they had been immobile before being admitted to hospital for SARS, had a history of pulmonary resection, or had a documented neurologic or psychiatric disease. We obtained written informed consent from patients prior to pulmonary function testing. This study was approved by the institutional ethics committee.
One hundred seventy-four consecutive SARS survivors were evaluated for this study (Fig 1). Twenty-seven patients were excluded from the study for the reasons outlined in Figure 1. Seventeen patients were uncontactable, and 7 were overseas during the study period. Of the remaining 123 patients, 29 declined to participate in this study. The diagnosis of SARS was confirmed by a positive serology result for SARS-CoV in all except 1 of the 94 patients enrolled in this study.
[FIGURE 1 OMITTED]
Pulmonary Function Testing
Pulmonary function tests at 1 year after hospital discharge included spirometry, and measurements of total lung capacity and diffusing capacity of the lung for carbon monoxide (DLCO). The protocol and equipment used for pulmonary function testing in this study were similar to those used in an earlier study (9) that we conducted among recovered SARS patients. Spirometry was performed in accordance with recommended standards. (14) All of the lung function tests were performed with the subjects seated and on the same day, but after patients had answered the health status questionnaire. FVC and FE[V.sub.1] were measured with a clinical spirometer (Vmax 229; SensorMedics; Yorba Linda, CA). Total lung capacity and its subdivisions were measured by the nitrogen washout method with the spirometer, the testing adhered to standard criteria. (15) The DLCO was determined by the single-breath carbon monoxide technique (16) using an infrared analyzer (Vmax 229). DLCO was adjusted for a hemoglobin concentration of 14.6 g/dL for men and 13.4 g/dL for women. (16) The spirometry, lung volumes, and DLCO measurements were expressed as the percentages of predicted normal values using reference values taken from the prediction equations of Chia et al (17) and Poh and Chia. (18) The rating of impairment was made according to the American Thoracic Society (ATS) statement (19) for the evaluation of impairment/disability secondary to respiratory disorders.
Health Status Measurement
All of the eligible patients completed the Singapore-English version of the St. George respiratory questionnaire (SGRQ). The SGRQ is a standardized, self-administered, pulmonary-specific health status questionnaire containing 50 items and 76 weighted responses that is divided into three subscales, as follows: (1) symptoms (8 items); (2) activity (16 items); and (3) impacts (26 items). SGRQ scores were calculated using score calculation algorithms and missing data imputation recommended by its developer. For each subscale and for the overall questionnaire, scores range from 0 (no impairment) to 100 (maximum impairment). Mean scores obtained from a sample of persons (n = 74) between 17 and 80 years of age (mean age, 46 years) who had no history of respiratory disease (mean FE[V.sub.1], 95%) served as reference values (P.W. Jones, MD; Scoring Manual of the SGRQ May 2003).
Statistical Analysis
Comparisons between groups were done with the Student t test for normally distributed continuous variables and with Mann-Whitney U tests for nonnormally distributed continuous variables. The linear regression model was used to study the association between known prognostic indicators of SARS and the 1-year pulmonary function outcomes, as well as the association between mechanical ventilation parameters during the acute illness and 1-year pulmonary function outcomes. Results were reported as the mean [+ or -] SD. The conventional level of statistical significance of 0.05 was used for all of the analyses.
RESULTS
The baseline characteristics of the enrolled patients during their hospital admission for SARS are shown in Table 1. Forty-seven of the 94 patients (50%) were health-care workers. The mean ([+ or -] SD) of the percentage of lung involvement based on the worst chest radiograph appearance during the acute illness using a scoring system similar to that of Wong et al (20) was 40.6 [+ or -] 29.9%. Eleven patients (12%) required admission to the ICU, and the mean Pa[O.sub.2]/ fraction of inspired oxygen (FI[O.sub.2]) ratio among these patients in the ICU was 95.5 [+ or -] 65.6. Seven of these patients required mechanical ventilation. All seven of the patients had a Pa[O.sub.2]/FI[O.sub.2] ratio of [less than or equal to] 200 while receiving mechanical ventilation with a positive end-expiratory pressure of [greater than or equal to] 5 cm [H.sub.2]O and evidence of airspace changes in all four of the quadrants on chest radiography. Overall, seven patients (7%) had a history of cigarette smoking. Nineteen patients (20%) had significant preexisting medical conditions. The four most common preexisting illnesses were hypertension (six patients), bronchial asthma (five patients), treated pulmonary tuberculosis (three patients), and diabetes mellitus (two patients).
Comparing the SARS survivors who were enrolled in this study with those who were not included, there was no significant difference with regard to age, gender, steroid exposure, or severity of the acute illness as indicated by the length of hospitalization, the requirement for intensive care or mechanical ventilation, and the highest recorded serum lactate dehydrogenase (LDH) level (Table 2). Of the seven enrolled patients who had required mechanical ventilation, the mean duration of mechanical ventilation was 1.5 days compared with 11 days for the five patients who required mechanical ventilation among the 80 survivors who were not included in this study. The difference in the mean duration of mechanical ventilation between these two subsets of patients was not statistically significant (p = 0.443).
At 1 year after hospital discharge, with regard to respiratory symptoms that were present at least a few days a month over the preceding year, 28 patients (30%) had cough, 19 (9.0%) had increased sputum production, 28 (30%) had shortness of breath, and 7 (7%) had occasional wheezing. The mean body mass index of the group at this time was 23.4 [+ or -] 4.5.
The pulmonary function test results of the 94 patients are shown in Table 3. The group means of forced expiratory volumes, static lung volumes, and diffusion capacity were all within normal limits (ie, > 80% predicted). However, several cases of abnormalities in FVC, FE[V.sub.1], FE[V.sub.1]/FVC ratio, and DLCO were detected. According to the ATS recommendations (19) for evaluating respiratory impairment, 11 patients (12%) had mild impairment of FVC, 20 (21%) had mild impairment of FE[V.sub.1], 5 (5%) had mild impairment of FE[V.sub.1]/FVC ratio, and 17 (18%) had mild impairment of DLCO. There was one patient (1%) with moderate impairment of FVC, one patient (1%) with moderate impairment of FE[V.sub.1]/ FVC ratio, and three patients (3%) with moderate impairment of DLCO. Because there were cases of patients with impairment in more than one of the four variables, the number of patients with mild and moderate impairment according to the ATS recommendations was 30 (32%) and 5 (5%), respectively. Table 4 shows the pulmonary function data of these 35 patients who had respiratory impairment. The majority of the impairment in FE[V.sub.1] and FVC suggests a restrictive abnormality, but in only eight patients was the total lung capacity (TLC) < 80% predicted. Two patients had obstructive abnormality with an FE[V.sub.1]/FVC ratio < 70% predicted, and one of them (patient No. 17 in Table 4) had a history of poorly controlled bronchial asthma. The other patient (patient No. 12 in Table 4) had a significant history of cigarette smoking. None of the other patients who had respiratory impairment were current or ex-smokers. The preexisting medical conditions that may affect pulmonary function in the patients with pulmonary function abnormalities are as shown in Table 4.
Table 5 shows the serial pulmonary function data of 17 patients in the present study who were detected to have abnormalities from among a group of patients who had been evaluated at 3 months after hospital discharge in an earlier study. (9) The mean DLCO improved significantly by 8.3% (p = 0.047) at 1 year, but no significant changes were detected in the other pulmonary function variables of these 17 patients.
Comparing the pulmonary function of patients who required ICU care and mechanical ventilation during hospitalization for SARS with those who did not, there was no significant difference in FVC, FE[V.sub.1], FE[V.sub.1]/FVC ratio, or DLCO between the two groups. Using multivariate analysis to analyze the association between known prognostic indicators of SARS, (2) namely, age, gender, comorbidity, serum LDH level, ribavarin level, and steroid use, and the 1-year pulmonary function outcomes, we found that only age was significantly associated with the FVC percent predicted (every year increase, -0.34; 95% confidence interval, -0.6 to -0.08; p = 0.01) and with the FE[V.sub.1] percent predicted (every year increase, -0.26; 95% confidence interval, -0.5 to -0.01; p = 0.04), but none of the prognostic factors were significantly associated with the DLCO percent predicted. Among patients who required intensive care and mechanical ventilation during the acute illness, there was no significant association among the duration of mechanical ventilation, the Pa[O.sub.2]/ FI[O.sub.2] ratio on admission to the ICU, steroid usage, and the pulmonary function parameters at 1 year after hospital discharge. All 94 of the patients completed the SGRQ. Domain scores other than the symptoms domain of the SGRQ were significantly higher (ie, worse) than the population norms (Table 6).
DISCUSSION
Impaired pulmonary function is present in about one third of patients 1 year after their recovery from SARS. The most common pulmonary function impairment was of the FE[V.sub.1] and DLCO. As measured by the SGRQ, SARS survivors had significant worsening in health status compared with the healthy population.
To date, reported studies on the functional outcomes of patients during the recovery stage of SARS are limited, (3-6,9) and none has evaluated the outcomes at a uniform 1-year time point. In assessing long-term outcomes after acute lung injury, it is important to attempt the consecutive enrollment of survivors with defined time points for study, because there is a possibility of bias toward the selection of sicker patients with abnormal pulmonary function test results if studies enrolled any patient who returned for a follow-up evaluation. In an earlier prospective study (9) of pulmonary function tests in 46 recovered SARS patients at a uniform time point of 3 months after hospital discharge, we found 7 patients (15%) with mild impairment of FVC, 12 patients (26%) with mild impairment of FE[V.sub.1], 17 patients (37%) with mild impairment of DLCO, and 1 patient (2%) with moderate impairment of DLCO. Overall, pulmonary function defects were detected in half of the recovered SARS patients at 3 months after hospital discharge. The finding in the present study of persistent pulmonary function abnormalities in a significant proportion of SARS patients 1 year after hospital discharge is notable, not only for the long-term follow-up and management of these patients but also as a highlight of the permanent respiratory impairment that can result from the acute infection. Viral pneumonia usually resolves without any clinical or radiologic sequelae, whereas SARS-related radiologic sequelae appear to be quite common among survivors, as observed by several studies. (8,21)
The finding of higher prevalence of dynamic lung volume abnormalities than DLCO impairment in the present study, together with the significant improvement in DLCO but not dynamic lung volumes in serial lung function testing of a subset of our patients, suggest that DLCO abnormalities can improve with time. In contrast, ventilatory abnormalities are more likely to persist in the long term. This appears to be in contrast to information from several reviews (22,23) on survivors of the ARDS documenting the persistence of a mild reduction in DLCO as the most common abnormality found in pulmonary function testing, and that DLCO remained low in long-term follow-ups. Interestingly, all of the articles on ARDS survivors reporting normal lung volumes or very low rates of either obstruction or restriction were published earlier when cohorts were likely more heterogeneous, and lung injuries in the surviving population were most likely less severe. (24-26) In more recent studies, the proportion of patients with ventilatory impairment has ranged constantly higher, from 18 to 33% for airway obstruction and from 15 to 45% for lung restriction (27-30) In particular, Neff et al (31) have reported that residual restrictive and obstructive types of functional impairment remained common (25% of patients with each type) in survivors of severe ARDS, and only 12.5% of patients had impairment in DLCO.
The exact pathologic cause(s) of the pulmonary dysfunction in recovered SARS patients is not known. Adverse long-term pulmonary sequelae of the ARDS include lung fibrosis, but untreated bronchiolitis obliterans-organizing pneumonia and bronchiolitis obliterans may 'also contribute to the physical morbidity in ARDS survivors. (32) In addition, neuromuscular weakness may also contribute to the decline in pulmonary function. (33) A recent study (8) correlating high-resolution CT scan findings and pulmonary function in survivors of SARS during the early recovery phase (ie, 25 to 38 days after hospital discharge) found that FE[V.sub.1], FVC, TLC, residual volume, and DLCO correlated well with the severity of ground-glass opacification and fibrosis. The presence of fibrosis was associated with significantly lower pulmonary function variables. It would be interesting to compare structural and functional changes in survivors of SARS during late recovery to see whether a similar correlation persists and whether these changes are different from those observed in ARDS survivors whose condition is not related to SARS.
In contrast to the results of the earlier study (5) among patients averaging 28 days in the posthospital discharge period, significantly worse scores were not found in the symptoms domain of the SGRQ among our SAILS survivors at 1 year. This is likely attributable to an improvement in symptoms with time of recovery. In studies among survivors of ARDS, it is known that nearly all of the patients are symptomatic at hospital discharge, but there is significant improvement over the first year after ARDS in most patients. (11) In addition, survivors of ARDS are also much less symptomatic than other patients with chronic lung disease. (11) Nonetheless, the mean activity score of our patients measuring disturbances to their daily physical activity and their mean impacts score covering a wide range of disturbances of psychosocial function remain significantly worse compared with those in healthy subjects. Physical morbidity in SAILS survivors may also stem from extrapulmonary causes. In an earlier study (9) evaluating pulmonary function and exercise capacity among patients from the same cohort, we found no evidence of exercise limitation solely because of ventilatory constraints, and there were very few patients with significant oxygen desaturation during exercise. Hence, the disability represented by an increased (ie, worse) score on the SGRQ activity domain in the present study is not likely to be specific to intrinsic pulmonary dysfunction, especially given that pulmonary dysfunction in our patients is modest, but may instead reflect any cause of impaired physical functioning, such as muscle loss/weakness or neuromuscular disease. Corticosteroid myopathy may be a contributory factor, although only a small percentage of our patients had received treatment with steroids during their acute illness.
There are several limitations of this study that we would like to acknowledge. First, the heterogeneity of acute lung disease encompassed by the case definition of SARS may account for the observed variation in pulmonary and extrapulmonary sequelae among our patients. Second, the proportion of patients who declined evaluation may have led to a bias toward the selection of sicker patients with abnormal pulmonary function. This is likely, because most of the patients who declined participation in the study offered a lack of symptoms and inconvenience as the main reasons for doing so. Third, evaluations of arterial blood gas levels and exercise testing were not performed in this study. However, we did not anticipate that there was significant hypoxemia in these patients, because none of them was found to have hypoxemia or was assessed as requiring oxygen supplementation during routine follow-up. Cardiopulmonary responses to exercise in SARS survivors had been evaluated in an earlier study (9) at 3 months after hospital discharge, but we do not have any longer term data on this. Fourth, only a respiratory-specific measure of health status was used in this study. A generic health status measure, such as the Medical Outcomes Study 36-item short-form health survey, would have provided a more global assessment of the patients, especially with regard to their role limitations as a result of emotional problems, mental health, bodily pain, and general health perceptions. The interaction of the data obtained from generic and disease-specific measures of health status may also have helped to determine the contributions of pulmonary and nonpulmonary factors to the longterm health status of SARS survivors.
In summary, 1 year after recovery from SARS, persistent pulmonary function impairment was found in about one third of patients. The health status of SARS survivors was also significantly worse compared with that of the healthy population.
ACKNOWLEDGMENT: We acknowledge the work of research coordinators M. Lee and W-F. Chong in the preparation of the manuscript, as well as that of the staff of the Respiratory Function Laboratory, Tan Toek Seng Hospital.
REFERENCES
(1) Ksiazek TG, Erdman D, Goldsmith CS, et al. A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med 2003; 348:1953-1966
(2) Rainer TH. Severe acute respiratory syndrome: clinical features, diagnosis, and management. Curr Opin Pulm Med 2004; 10:159-165
(3) Han Y, Geng H, Feng W, et al. A follow-up study of 69 discharged SARS patients. J Tradit Chin Med 2003; 23:214-217
(4) Peng M, Cai BQ, Liu T, et al. Assessment of pulmonary function in SARS patients during the convalescent period. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 2003; 25:529-532
(5) Liu T, Peng M, Cai BQ, et al. Assessment of health-related quality of life in cured SARS patient. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 2003; 25:16-19
(6) Xie LX, Liu YN, Hao FY, et al. Prognostic analysis of lung function and chest X-ray changes of 258 patients with severe acute respiratory syndrome in rehabilitation after discharge. Zhonghua Jie He He Hu Xi Za Zhi 2004; 27:147-150
(7) Tian Q, Liu YN, Xie LX, et al. Comparative study of clinical characteristics and prognosis of clinically diagnosed SARS patients with positive and negative serum SARS coronavirus-specific antibodies test. Zhonghua Yi Xue Za Zhi 2004; 84:642-645
(8) Hsu HH, Tzao C, Wu CP, et al. Correlation of high-resolution CT, symptoms, and pulmonary function in patients during recovery from severe acute respiratory syndrome. Chest 2004; 126:149-158
(9) Ong KC, Ng AWK, Lee LSU, et al. Pulmonary function and exercise capacity in survivors of severe acute respiratory syndrome. Eur Respir J 2004; 24:436-442
(10) Herridge MS, Cheung AM, Tansey CM, et al. One-year outcomes in survivors of acute respiratory distress syndrome. N Engl J Med 2003; 348:683-693
(11) Lee CM, Hudson LD. Long-term outcomes after ARDS. Semin Respir Grit Care Med 2001; 22:327-336
(12) Hsu LY, Lee CC, Green JA, et al. Severe acute respiratory syndrome (SARS) in Singapore: clinical features of index patient and initial contacts. Emerg Infect Dis 2003; 9:713-717
(13) World Health Organization. Case definitions for surveillance of severe acute respiratory syndrome (SARS). 2003; 4. Available at: http://www.who.int/esr/sars/casedefinition/en/. Accessed August 7, 2004
(14) American Thoracic Society. Standardization of spirometry. Am J Respir Grit Care Med 1995; 152:1107-1136
(15) Quanjer PH, Tammeling GJ, Cotes JE, et al. Lung volumes and forced ventilatory flows: Report Working Party Standardization of Lung Function Tests, European Community for Steel and Coal; Official Statement of the European Respiratory Society. Eur Respir J Suppl 1993; 16:5-40
(16) American Thoracic Society. Single-breath carbon monoxide diffusing capacity (transfer factor): recommendations for a standard technique; 1995 update. Am J Respir Grit Care Med 1995; 152:2185-2198
(17) Chia SE, Wang YT, Chan OY, et al. Pulmonary function in healthy Chinese, Malay and Indian adults in Singapore. Ann Acad Med Singapore 1993; 22:878-884
(18) Poh SC, Chia M. Respiratory function tests in normal adult Chinese in Singapore. Singapore Med J 1969; 10:265-271
(19) American Thoracic Society. Evaluation of impairment/disability secondary to respiratory disorders. Am Rev Respir Dis 1986; 133:1205-1209
(20) Wong KT, Antonio GE, Hui DS, et al. Severe acute respiratory syndrome: radiographic appearances and pattern of progression in 138 patients. Radiology 2003; 228:401-406
(21) Antonio GE, Wong KT, Hui DS, et al. Thin-section CT in patients with severe acute respiratory syndrome following hospital discharge: preliminary experience. Radiology 2003; 228:810-815
(22) Luhr O, Aardal S, Nathorst-Westfelt U, et al. Pulmonary function in adult survivors of severe acute lung injury treated with inhaled nitric oxide. Acta Anaesthesiol Scand 1998; 42:391-398
(23) Herridge MS. Long-term outcomes after critical illness. Curr Opin Crit Care 2002; 8:331-336
(24) Buchser E, Leuenberger P, Chiolero R, et al. Reduced pulmonary capillary blood volume as a long-term sequel of ARDS. Chest 1985; 87:608-611
(25) Ruhle KH, Schuster A, Vogel W, et al. Follow-up examinations of lung function in patients with shock lung [in German]. Prax Klin Pneumol 1983; 123:492-495
(26) Klein JJ, van Haeringen JR, Sluiter HJ, et al. Pulmonary function after recovery from the adult respiratory distress syndrome. Chest 1976; 69:350-355
(27) McHugh LG, Milberg JA, Whitcomb ME, et al. Recovery of function in survivors of the acute respiratory distress syndrome. Am J Respir Crit Care Med 1994; 150:90-94
(28) Bachofen M. Prognosis following extubation in severe ARDS [in German]. Schweiz Med Wochenschr 1991; 121:1552-1556
(29) Peters JI, Bell RC, Prihoda TJ, et al. Clinical determinants of abnormalities in pulmonary thnetions in survivors of the adult respiratory distress syndrome. Am Rev Respir Dis 1989; 139:1163-1168
(30) Ghio AJ, Elliot CG, Crapo RO, et al. Impairment after adult respiratory distress syndrome: an evaluation based on American Thoracic Society recommendations. Am Rev Respir Dis 1989; 139:1158-1162
(31) Neff TA, Stoeker R, Frey HR, et al. Long-term assessment of lung function in survivors of severe ARDS. Chest 2003; 123:845-853
(32) Herridge MS, Cheung AM, Tansey CM, et al. Long term outcomes in survivors of ARDS [abstract]. Am J Respir Crit Care Med 2002; 165:A254
(33) Aggarwal AN, Gupta D, Behera D, et al. Analysis of static pulmonary mechanics helps to identify functional defects in survivors of acute respiratory distress syndrome. Crit Care Med 2000; 28:3480-3483
* From the Departments of Respiratory Medicine (Drs. Ong and Ng), Infectious Diseases (Dr. Lee), Diagnostic Radiology (Dr. Kaw), Psychological Medicine (Dr. Kwek), General Medicine (Dr. Leow), and Clinical Epidemiology (Mr. Earnest), Tan Tock Seng Hospital, Singapore.
This study was supported by a grant from the A*STAR Biomedical Research Council.
Manuscript received September 19, 2004; revision accepted January 18, 2005.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjourual. org/misc/reprints.shtml).
Correspondence to: Kian-Chung Ong KCOng Chest and Medical Clinic, Mount Elizabeth Medical Centre, 3 Mount Elizabeth #12-03, Singapore 228510; e-mail: ongkianchung@yahoo.com.sg
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group