Objectives: To study the effectiveness of noninvasive positive pressure ventilation (NIPPV) in the treatment of acute respiratory failure (ARF) in severe acute respiratory syndrome (SARS), and the associated infection risk.
Methods: All patients with the diagnosis of probable SARS admitted to a regional hospital in Hong Kong from March 9 to April 28, 2003, and who had SARS-related respiratory distress complications were recruited for NIPPV usage. The health status of all health-care workers working in the NIPPV wards was closely monitored, and consent was obtained to check serum for coronavirus serology. Patient outcomes and the risk of SARS transmission to health-care workers were assessed.
Results: NIPPV was applied to 20 patients (11 male patients) with ARF secondary to SARS. Mean age was 51.4 years, and mean acute physiology and chronic health evaluation II score was 5.35. Coronavirus serology was positive in 95% (19 of 20 patients). NIPPV was started 9.6 days (mean) from symptom onset, and mean duration of NIPPV usage was 84.3 h. Endotracheal intubation was avoided in 14 patients (70%), in whom the length of ICU stay was shorter (3.1 days vs 21.3 days, p < 0.001) and the chest radiography score within 24 h of NIPPV was lower (15.1 vs 22.5, p = 0.005) compared to intubated patients. Intubation avoidance was predicted by a marked reduction in respiratory rate (9.2 breaths/min) and supplemental oxygen requirement (3.1 L/min) within 24 h of NIPPV. Complications were few and reversible. There were no infections among the 105 health-care workers caring tbr the patients receiving NIPPV.
Conclusions: NIPPV was effective in the treatment of ARF in the patients with SARS studied, and its use was safe for health-care worker. (CHEST 2004; 126:845-850)
Key words: acute respiratory failure; endotracheal intubation; infection control; noninvasive positive pressure ventilation; severe acute respiratory syndrome
Abbreviations: APACHE = acute physiology and chronic health evaluation; ARF = acute respiratory failure; CXR = chest radiograph; ePAP = expiratory positive airway pressure; iPAP = inspiratory positive airway pressure; NIPPV = noninvasive positive pressure ventilation; SARS = severe acute respiratory syndrome
**********
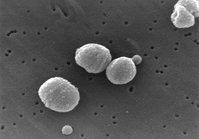
Severe acute respiratory, syndrome (SARS) was first defined by the World Health Organization in mid-March 2003. (1) It is a highly infectious disease due to a novel coronavirus, the SARS-associated coronavirus. (2-4) Its clinical course can be stormy, with 14 to 25% of cases progressing to acute respiratory failure (ARF) and requiring endotracheal intubation and mechanical ventilation. (5,6) Pathologic findings of early SARS are compatible with focal changes of ARDS. (7) Noninvasive positive pressure ventilation (NIPPV) is known to be effective in the treatment of early ARDS. (8) Owing to the fear of leakage from the mask interface with subsequent transmission of SARS to health care workers, the rate of NIPPV use for patients with SARS in Hong Kong was very low, even though there had been 1,755 infected patient-sof whom 15 to 25% would require assisted ventilation or intensive care. (5) The effectiveness of NIPPV in patients with SARS has so far not been studied or reported. To avoid the risk of nosocomial pneumonia in intubated patients, which is of particular relevance in our patients with SARS because the standardized treatment routinely used in our hospital contains high-dose corticosteroids, (9) we aimed to evaluate the effectiveness of NIPPV in the early respiratory failure of SARS. We also aimed to evaluate the infection risk among health-care workers with direct contact with patients receiving NIPPV.
MATERIALS AND METHODS
Patients
This was a retrospective study of patients who could fulfil the latest definitions of probable SARS according to both the World Health Organization and the Centers for Disease Control and Prevention, (10,11) and had used NIPPV for treatment of ARF secondary to SARS. All were admitted to Pamela Youde Nethersole Eastern Hospital, Hong Kong, from March 9 to April 28, 2003, and subsequently had complications of SARS-related respiratory failure, to the extent that > 6 L/min of supplemental oxygen was required to maintain oxygen saturation at 93 to 96%. All patients were treated with our standard protocol of broad spectrum antibiotics, ribavirin, and corticosteroid. (9) Our 21-day steroid treatment protocol was as follows: IV methylprednisolone, 1 mg/kg tid for 5 days; then 1 mg/kg bid for 5 days; then oral prednisolone, 0.5 mg/kg bid for 5 days; then 0.5 mg/kg/d for 3 days; and finally 0.25 mg/kg/d for 3 more days. In case of rapid clinical and radiologic deterioration, a course of pulsed methyl-prednisolone, 500 mg bid for 2 days, was administered as rescue therapy. (9)
Noninvasive Ventilation Settings
NIPPV was delivered from a bilevel positive airway pressure system (BiPAP; Respironics; Murrysville, PA) with maximal positive pressures of 20 cm [H.sub.2]O or 30 cm [H.sub.2]O. The spontaneous-timed mode was used for all patients, with a back-up rate of 12 breaths/min. Inspiratory positive airway pressure (iPAP) was adjusted to achieve respiratory rates of < 25 breaths/min and exhaled tidal volumes of at least 6 mL/kg. Expiratory positive airway pressure (ePAP) was adjusted to achieve target oxygenation with minimum carbon dioxide rebreathing. In order to decrease production of droplets, the following three strategies were implemented: (1) a facial mask was preferred to a nasal mask to decrease the leakage of air from the month; (2) a Whisper-Swivel II (Respironics) was used as the exhalation device, because compared with the jet outflow of the Whisper-Swivel I, its round-the-tube outflow may reduce the chance of jets of expired air from the patients with SARS contaminating the environment; and (3) a viral-bacterial filter (Airlife; Allegiance Healthcare; McGaw Park, IL) was placed before the exhalation device from March 21, 2003, onwards to decrease the viral bacterial load to the environment. Oxygen was connected to the mask, and the fraction of inspired oxygen was estimated from the oxygen flow rate and minute volume. (12, 13)
All patients were maintained continuously on NIPPV for at least 6 h after initiation. Thereafter, the mask could be removed for short periods of up to 30 min each for meals and sputum clearance. Respiratory rate, oxygen saturation, oxygen supplement requirement, and arterial blood gas results were closely monitored. Intubation was indicated if patients showed respiratory distress and/or when the supplemental oxygen requirement was > 12 L/min to maintain oxygen saturation of 93%. When improvement in respiratory rate and decrease in oxygen requirement were evident, gradual weaning in the daytime followed by sleeping hours was performed.
Radiologic Studies
All chest radiographs (CXRs) were semiquantified and independently scored by two pulmonologists who were blinded to individual patient's clinical information. Each lung was separated into six sections (upper, middle, and lower zones; medial and lateral divisions), and each section was scored based on a 4 point scale: 0 clear, 1 = subtle haziness or mild infiltrates, 2 = ground-glass appearance or prominent infiltrates, and 3 = confluent or dense opacities. (9)
Infection Control
Because of a possible risk of aerosol generation resulting from leakage at the mask-face interface during bilevel pressure ventilation, stringent infection control measures were implemented. Patients were cared for in central air-conditioned isolation rooms in the ICU or in general ward isolation cubicles. Through installation of exhaust ventilation fans in each area to achieve negative pressure airflow, air changes were maintained at 8/h initially (before March 18, 2003) and later at > 12/h. Airflow was directed from the corridors outside the ward through the nursing station to patient areas and finally out to the atmosphere. Before mid-April 2003, personal protective equipment for all health-care workers included surgical or N-95 masks, protective eye wear, full-face shields, caps, gown with full sleeve coverage, surgical gloves, and shoe covers. After mid April 2003, personal protective equipment during direct contact with patients receiving NIPPV was upgraded to an Air-Mate HEPA Powered Air Purifying Respirator System (3M Corporation; St. Paul, MN), which was recommended by the Centers for Disease Control and Prevention as an interim domestic infection control for aerosol-generating procedures on patients with SAIRS. (14) The Air-Mate HEPA Powered Air Purifying Respirator System is a device with face piece and hood that filters the surrounding air through a built-in-high-efficiency particulate air filter before supplying to the user.
The health status of all health-care workers with direct contact with patients receiving NIPPV was closely monitored. All staff with fever or respiratory symptoms would be seen by pulmonologists, and chest radiography and blood tests would be performed to exclude SARS. Consent was also obtained to check serum for coronavirus serology in mid-April, May, or July 2003.
Outcome Assessment
NIPPV success was defined as follows: (1) the ability to be weaned from NIPPV for [greater than or equal to] 24 h, and (2) avoidance of endotracheal intubation secondary to SARS deterioration. Infection directly attributable to NIPPV was defined as development of SARS in health-care workers within 10 days of starting to work in a NIPPV ward.
Data Collection
For patients, the following general data were collected: age, gender, date of symptom onset, date of hospital admission, serology result for coronavirus, date of starting steroid and ribavirin, date of starting pulse steroid, total course of pulsed steroid given, and underlying illnesses. Data related to NIPPV included the following: NIPPV starting date; acute physiology and chronic health evaluation (APACHE) II score; iPAP and ePAP level used; tidal volume; respiratory, rate, oxygen saturation, supplemental oxygen requirement, and/or arterial blood gas measurement and blood test results on hospital admission, before NIPPV, within 24 h of NIPPV, and before removing NIPPV/ intubation; CXR stores; duration of NIPPV usage; ICU and hospital survival; ICU and hospital stay; and outcome in terms of intubation status, mortality, and NIPPV-related complications.
Statistical Analysis
All data were expressed as mean [+ or -] SD unless specified. Categorical variables were analyzed with [chi square] test. For continuous variables, all between subject comparisons were performed with Mann-Whitney U test, and all within-subject comparisons were performed with Wilcoxon test. Statistical significance was taken at p < 0.05.
RESULTS
>From March 9, 2003, 90 patients were admitted to the hospital with probable SARS, of whom 87 patients (96.7%) had positive serology findings for SARS-associated coronavirus. NIPPV was used in 23 episodes for 22 patients. Three episodes were excluded from analysis because NIPPV was used for treatment of acute pulmonary edema (two episodes) and for weaning after extubation (one episode). Of the remaining 20 episodes in the 20 recruited patients (11 men), the mean age was 51.4 [+ or -] 14.2 years. Seven patients had underlying comorbidities singly or in combination: diabetes mellitus (n = 5), hypertension (n = 3), and ischemic heart disease (n = 1). Nineteen patients (95%) had fourfold or greater rises in antibody titer to the SARS-associated coronavirus. Demographic, physiologic, and blood test results for these 20 patients on hospital admission are shown in Table 1. The timing of starting ribavirin and steroid, pulsed methylprednisolone, and NIPPV treatment were 7.2 [+ or -] 8.3 days, 8.7 [+ or -] 2.4 days, and 9.6 [+ or -] 4.0 days, respectively, from symptom onset. Average respiratory rate before NIPPV was 28.9 [+ or -] 6.2 breaths/min with supplemental oxygen of 8.0 [+ or -] 3.1 L/min to maintain an oxygen saturation of 93.1 [+ or -] 5.0%. Because of the sudden onset and rapid rate of respiratory deterioration in many patients, pre-NIPPV arterial blood gas results were available in only nine patients, with average Pa[O.sub.2]/fraction of inspired oxygen being 18.3 [+ or -] 6.9 kPa (137.5 [+ or -] 51.6 mm Hg) and PaC[O.sub.2] of 4.5 [+ or -] 0.62 kPa (33.9 [+ or -] 4.6 nun Hg). Intubation was avoided in 14 patients. NIPPV was not successful in six patients, mad they required endotracheal intubation.
CXR scores before NIPPV were 16.4 [+ or -] 6.7 and 21.5 [+ or -] 4.3, respectively (p = 0.153), in the success and failure groups. The mean CXR score within 1 day after NIPPV was significantly higher for the failure group (22.5 [+ or -] 3.3 vs 15.1 [+ or -] 6.0, p = 0.005). All patients received at least one course of pulsed methylprednisolone (2 g), with two courses being administered to three patients in whom NIPPV failed. Success was predicted by a marked and statistically significant reduction in respiratory rate and supplemental oxygen requirement within 24 h and at the end of NIPPV (Fig 1).
[FIGURE 1 OMITTED]
Overall mean duration of NIPPV usage was 84.3 [+ or -] 47.0 h, and mean durations of ICU and hospital stay were 8.6 [+ or -] 14.0 days and 33.7 [+ or -] 13.5 days, respectively. Analyses of clinical outcome and laboratory results between the success and failure groups are shown in Table 2. ICU stay for the success group was significantly shorter than the failure group (3.1 [+ or -] 2.1 days vs 21.3 [+ or -] 21.2 days, p < 0.001). Two elderly patients (aged 66 years and 72 years) with comorbidities (diabetes mellitus and hypertension) could be totally weaned from NIPPV, but later had fatal acute myocardial infarction and acute ischemic stroke, respectively. A third fatality occurred in another elderly (aged 74 years) with ventilator-associated pneumonia.
NIPPV was complicated in four patients by pneumothorax (n = 1), pneumomediastinum (n = 1), nosceomial pneumonia (n = 1), and pneumomediastinum plus nosocomial pneumonia (n = 1). All recovered without major consequences. The overall incidence of nosocomial pneumonia was 2 of 20 patients (10%) during NIPPV usage, while the nosocomial pneumonia rate for the intubated group was 2 of 6 patients (33.3%) during mechanical ventilation.
Infection Risk
One hundred five health-care workers, including doctors, nurses, and health-care assistants, had taken care of patients receiving NIPPV. None had acquired SARS from the patients. One hundred two health-care workers (97.1%) consented to have serum checked for coronavirus serology, and none showed evidence of coronavirus infection.
DISCUSSION
Progression of SARS to ARF is common. Most patients with SARS and ARF were treated with endotracheal intubation and mechanical ventilation. (5,6) In the present series, NIPPV was effective in preventing endotracheal intubation in 70% (14 of 20 patients). The efficacy of NIPPV may be attributed to early recruitment of the collapsed alveoli and resting of respiratory, muscles while waiting for the action of pulsed corticostcroids to take effect. Since our patients who responded to NIPPV did so within 24 h, patients who would eventually need endotracheal intubation may thus be potentially identified early in the course of treatment. This finding is similar to the results of the use of NIPPV in other forms of ARF. (15)
All three deaths in our series occurred in the elderly, with two patients having underlying comorbidities. This is similar to the higher mortality rates of SARS in such patients in Hong Kong (daily press briefing, May 8, 2003; Department of Health and Hospital Authority, Hong Kong). The overall intubation and mortality rates in our 90 patients with SARS were 10% and 4.4%, respectively. Our comparatively lower mortality rate (16) may partly be explained by the use of NIPPV, which may reduce the need for emergency intubation and intensive care admission when applied early to patients with SARS and severe acute hypoxemic respiratory failure.
Since a severe outbreak of SARS in another Hong Kong hospital was attributed to the use of nebulized treatment in a patients with SARS, (5) whether or not NIPPV use in patients with SARS poses a similar infection risk remains a controversial issue. Based on our prior experience with NIPPV in ARF, (17) and the safety and efficacy in its early use in a negative pressure environment, (9) we continued to utilize this treatment modality with strict enforcement of personal protection measures and close monitoring of health status of all involved staff. The subsequent successful sourcing and additional use of an expiratory viral and bacterial filter might also have contributed to prevention of staff infection. We hope that our experience could alleviate the anxiety of all health-care workers caring for patients with SARS, such that patients would not be deprived of NIPPV as an important modality of assisted ventilation.
Comparing with previous experiences with NIPPV, (15,17,18) major complication rates (barotrauma and nosocomial pneumonia) were relatively high in our patients with SARS. While nosocomial pneumonia can be explained by the use of high-dose corticosteroids, barotrauma may or may not be related to NIPPV since spontaneous pneumothorax or pneumomediastinum without ventilation were seen in six of our patients, as well as in 12% in another series from Hong Kong. (19)
Our study is limited by the lack of a control group, and its retrospective nature. These problems were difficult to avoid in a rapid outbreak of an unknown disease. At the time of our planned randomized control study on NIPPV and endotracheal intubation in late April, SARS was already dying down in Hong Kong, and our last patient with SARS was clinically confirmed on April 28, 2003. To validate the effectiveness of NIPPV in SARS-related ABF, larger-scale prospective randomized control studies can be considered in the next outbreak. Our study also suffers from the low availability of pre-NIPPV blood gas results, which in conjunction with lack of multi-organ failure led to low APACHE II scores. However, the progression of respiratory failure was so fast that treatment decisions took precedence over blood work in this very infectious condition. From the level of oxygen requirement and corresponding oxygen saturation, all patients without blood gas data could fulfil the criteria for type 1 respiratory failure. Our study is also limited by the incomplete coronavirus serology for the 105 health-care workers, as three of the health-care workers refused to give consent for blood taking.
CONCLUSION
NIPPV was an effective and safe treatment modality for the patients with SARS mad ARF in this study. Use of NIPPV in a negative pressure environment was also safe for health-care workers equipped with the appropriate personal protective equipment.
* From the Division of Respiratory and Critical Care Medicine, Department of Medicine (Drs. Cheung, Yam, So, Lau, Poon, and Kong), and Department of Microbiology (Dr. Yung), Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, PRC.
REFERENCES
(1) World Health Organization. World Health Organization issues emergency travel advisory. Available tit: http://www. who.int/csr/sars/archive/2003_03_15/en/. Accessed August 16, 2004
(2) Peiris JSM, Lai ST, Pooh LLM, et al. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet 2003; 361:1319-1325
(3) Ksiazek TG, Erdman D, Goldsmith CS, et al. A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med 2003; 348:1953-1966
(4) Dmsten C, Gunther S, Preiser W, et al. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med 2003; 348:1967-1976
(5) Lee N, Hui D, Wu A, et al. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med 2003; 348:1986-1994
(6) Booth CM, Matukas LM, Tomlinson GA, et al. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA 2093; 289:2801-2809
(7) Nicholls JM, Poon LLM, Lee KC, et al. Lung pathology of fatal severe acute respiratory syndrome. Lancet 2003; 361: 1773-1778
(8) Rocker GM, Mackenzie MG, Williams B, et al. Noninvasive positive pressure ventilation: successful outcome in patients with acute lung injury/ARDS. Chest 1999; 115:173-177
(9) So LKY, Lau ACW, Yam LYC, et al. Development of a standard treatment protocol for severe acute respiratory, syndrome. Lancet 2003; 361:1615-1617
(10) World Health Organization. Case definitions for surveillance of severe acute respiratory syndrome (SARS), revised 1 May 2008. Available at http://www.who.int/csr/sars/casedefinition/ en/print.html. Accessed August 16, 2004
(11) Centers for Disease Control and Prevention. Updated interim U. S. case definition of severe acute respiratory syndrome (SARS), revised May 20, 2003. Available at: http://www. cdc.gov/incidod/sars/casedefinition.html. Accessed July 14, 2003
(12) Yam LYC. Clinical applications of oxygen therapy in hospitals and techniques of oxygen administration: a review. J HK Med Assoc 1993; 45:318-325
(13) Murray JF, Nadel JA, eds. Textbook of respiratory medicine. Philadelphia, PA: WB Saunders Company, Harcourt Brace Jovanovich, 1988; 1982-1986
(14) Centers for Disease Control and Prevention. Interim domestic infection control precautions for aerosol-generating procedures on patients with severe acute respiratory syndrome (SARS), revised May 20, 2003. Available at: http://www.cdc. gov/ncidod/sars/aerosolinfectioncontrol.htm. Accessed October 31, 2003
(15) Meduri GU, Turner RE, Abou-Shala N, et al. Noninvasive positive pressure ventilation via face mask: first line intervention in patients with acute hypercapnic and hypoxemic respiratory failure. Chest 1996; 109:179-193
(16) World Health Organization. Cumulative number of reported probable cases of SARS. Available at: http://www.who.int/csr/ sars/country/2003_06_06/en/. Accessed August 16, 2004
(17) Cheung MT, Yam LYC, Lau CW, et al. Use of non-invasive positive-pressure ventilation for acute respiratory failure: prospective study. Hong Kong Med J 2000; 6:361-367
(18) Brochard L, Mancebo J, Wysocki M, et al. Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med 1995; 333:817-822
(19) Peiris JSM, Chu CM, Cheng VCC, et al. Clinical progression and viral load in a community outbreak of coronavirus-associated SARS pneumonia: a prospective study. Lancet 2003; 361:1767-1772
Manuscript received August 7, 2003; revision accepted February 25, 2004.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@chestnet.org).
Correspondence to: Thomas M. T. Cheung, FHKAM, MRCP, FCCP, Department of Medicine, Pamela Youde Nethersole Eastern Hospital, 3, Lok Man Rd, Hong Kong SAR, PRC; e-mail: tommtcheung@yahoo.com.hk
COPYRIGHT 2004 American College of Chest Physicians
COPYRIGHT 2004 Gale Group