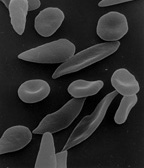
Sickle cell disease (SCD) is one of the most common genetic disorders in the United States. (1) Primary symptoms of this chronic disease include chronic hemolytic anemia and tissue damage secondary to vaso-occlusion by sickle-shaped red blood cells (Figure 1). Patients with SCD have an increased risk of developing cholelithiasis (ie, gallstones). (2) Cholelithiasis should be considered as a potential diagnosis when a child with SCD experiences recurrent abdominal pain. (3) Evaluation criteria used to confirm the diagnosis of cholelithiasis include radiological evaluation using biliary scintigram and ultrasound and laboratory results that indicate elevations in serum
[FIGURE 1 OMITTED]
* bilirubin,
* alkaline phosphatase,
* hepatic enzyme levels, and
* white blood cell count. (4)
An estimated 50% of patients in sickle cell crisis (ie, pain crisis) experience acute abdominal pain, which often is difficult to differentiate from acute cholecystitis. (5) One group of researchers noted that acute abdominal pain symptoms in children with SCD often were diagnosed as vaso-occlusive crisis rather than biliary colic associated with cholelithiasis. (6)
Cholecystectomy (ie, removal of the gallbladder) is the standard surgical intervention for the diagnosis of cholelithiasis in patients without a chronic illness. In contrast, cholecystectomy has been considered a controversial surgical intervention for children with SCD because these children usually display asymptomatic cholelithiasis. Currently, most physicians advocate elective cholecystectomy for children with SCD who display asymptomatic cholelithiasis to prevent symptoms of acute cholecystitis and the risk of requiring emergency cholecystectomy that may place them at risk of complications. (7) Typically, the indication for undergoing a cholecystectomy is the presence of symptomatic gallstones in patients, regardless of age. Prophylactic cholecystectomy also is appropriate for asymptomatic individuals who have a chronic illness (eg, SCD, diabetes) and those who have an increased risk of developing symptomatic gallstones. (8)
Cholelithiasis typically is observed less frequently in healthy children who do not have a chronic illness. Gallstones are observed with greater frequency among children with SCD. Age and chronic hemolysis are identified as the major factors that increase the risk of formation of black pigment type gallstones in children with SCD. (9) Additionally, development of pigment gallstones in children with SCD appears to be age dependent and occurs in approximately 15% of children younger than 10 years of age (10) and 50% of children by 20 years of age. (11) The incidence of gallstones varies with age across the life span for patients with SCD. For instance, the incidence is
* 12% in the two- to four-year-old age group, (12)
* 9% in the five- to seven-year-old age group, (13)
* 43% in the 15- to 18-year-old age group, (14)
* 83% in people older than 30 years of age, (15) and
* 60% to 85% in people age 33 or older. (16)
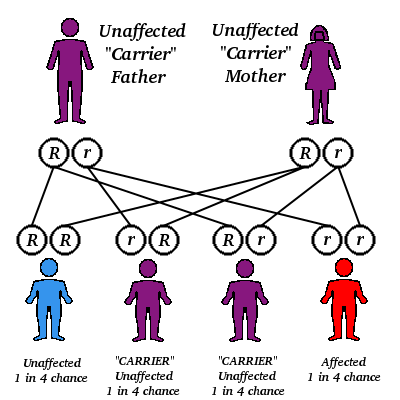
GALLBLADDER ANATOMY
The gallbladder's shape has been compared to a pear (Figure 2). It is approximately 7 cm long and holds 30 mL to 50 mL of bile. (17) Branches of the cystic artery originating from the right hepatic artery provide the gallbladder's blood supply. The common and right hepatic arteries provide the common bile duct with its blood supply. During cholecystectomy, the triangle of Calot serves as a surgical landmark to identify important structures. (18) These structures include the cystic duct, the common hepatic duct, and the inferior border of the liver. The common hepatic duct, gallbladder, and common bile duct function as a storage site for bile and a conduit for bile flow from the liver to the duodenum.
[FIGURE 2 OMITTED]
PIGMENT GALLSTONES
Children with chronic hemolytic disorders generally have an increased risk of developing pigment gallstones. (19) Pigment gallstones have been observed in 15% of children with SCD who are younger than 10 years of age. (20) and 50% of children with SCD by 20 years of age. The frequency of pigment gallstones is higher in this population because of a sustained increase in heme catabolism among children with SCD. (21)
Approximately 10% to 20% of gallstones are referred to as pigment stones. These are composed of poorly soluble calcium salts, especially calcium bilirubin, and are dark in color. Pigment stones are categorized as black, brown, or mixed pigment gallstones. Black pigment gallstones are small, hard, and spiculated (ie, sharp body with needle-like points) and are made of calcium bilirubinate, inorganic salts (eg, calcium phosphate), and calcium carbonate. (22) Black pigment stones typically develop in patients who have a history of excessive secretion of unconjugated bilirubin into bile. (23) Black pigment stones are observed in approximately 14% of children with SCD who are younger than 10 years of age. The percentage increases to 36% among school-age children and adolescents (ie, 10 to 20 years of age) and to 50% by age 22. (24)
Brown pigment stones are soft, crumbly aggregates that often form in the bile ducts of patients with a history of chronically infected bile above biliary strictures or cholesterol cysts. They are made of calcium bilirubinate and calcium palmitate. (25) Mixed gallstones are made of both cholesterol and calcium bilirubinate, and bacterial colonization or inflammation of the gallbladder may develop later. (26)
TREATMENT OF CHOLELITHIASIS
The current recommended treatment for children with SCD who are diagnosed with cholelithiasis is elective laparoscopic cholecystectomy. (27) An essential component of the preoperative preparation for elective cholecystectomy among children with SCD is erythrocyte transfusion therapy. The purpose of this therapy is to reduce the percentage of hemoglobin S and increase the hemoglobin concentration to greater than 10 g per dL. This reduces the risk of complications associated with vaso-occlusion. (28)
Risks associated with erythrocyte transfusion therapy among patients with SCD may include an increased risk of exposure to infectious agents and allosensitization to erythrocyte antigens. Undertaking these risks may be reasonable because of the decreased risk of postoperative morbidity with elective laparoscopic cholecystectomy compared to the traditional cholecystectomy procedure.
The primary goal of elective cholecystectomy is to prevent complications associated with emergency surgical intervention. Potential complications after emergency cholecystectomy in this patient population are associated with general anesthesia and the inability to implement recommended preoperative interventions, such as erythrocyte transfusion therapy. (29) In addition, children with SCD who undergo emergency cholecystectomy are at high risk of developing
* intraoperative complications, such as vaso-occlusion secondary to transient hypoxia, hypothermia, dehydration, or acidosis;
* postoperative complications, such as pneumonia, acute chest syndrome, or painful vaso-occlusive events; and
* other complications, such as ascending cholangitis (ie, inflammatory disease of the bile ducts), choledocholithiasis (ie, gallstones in the common bile duct), or acute cholecystitis (ie, gallstones or sludge obstructing the cystic duct). (30)
DEVELOPMENTAL THEORY FOR SCHOOL-AGE PATIENTS
Knowledge of the specific developmental characteristics of school-age children is important for nurses and other pediatric surgical team members. Child psychologist Jean Piaget, PhD, characterized children ages seven to 11 as being in the concrete operations stage of cognitive development. (31) Characteristics of this stage include interest in acquiring more detailed knowledge, improved concept of time, and increased self-control. Psychoanalyst Erik Erikson characterized children ages six to 12 as being in the industry versus inferiority stage of psychosocial development. (32) Characteristics of this stage include interest in
* participating in various school-related activities, such as development of peer relationships;
* attaining skills in competition and cooperation; and
* developing a sense of competence.
School-age children may experience anxiety before an unfamiliar or familiar medical procedure because of their increased cognitive ability. They may have many questions related to medical procedures that require health care providers to give age-appropriate explanations using correct scientific and medical terminology before all procedures. Explanation of these procedures can be enhanced by the use of simple anatomy and physiology diagrams and concrete terms explaining why and how equipment functions. According to developmental theory, school-age children are focused on gaining a sense of control and competence during various activities; therefore, health care providers should strive to keep children informed of what to expect before all medical procedures. Allowing time before procedures for patient questions and additional explanations is recommended. Health care providers also should educate school-age children about self-control strategies, such as helpful postoperative strategies (eg, deep breathing exercises, relaxation techniques, counting during dressing changes), before scheduled surgical procedures to prevent postoperative complications and minimize feelings of anxiety.
PREOPERATIVE PHASE
In the preoperative holding area, the circulating nurse and anesthesia care provider complete all required preoperative assessments for a pediatric patient before transferring the patient to the OR. Both participate in preoperative teaching for the parents to inform them about what their child will experience. The circulating nurse confirms the child's identity and the scheduled laparoscopic cholecystectomy procedure with the child's parents. The circulating nurse also verifies that all surgical informed consents are present and complete. In addition, the nurse documents the patient's allergies, NPO status, presences of prostheses, loose teeth, rashes, bruises, and any other pertinent information that facilitates safe patient care.
The perioperative nurse ensures that the following documents are present in the patient's chart:
* medical history,
* physical examination,
* preoperative records, and
* appropriate laboratory test results.
He or she then performs an assessment and documents the patient's physical condition, including vital signs, height, weight, and skin integrity. The nurse also can review age-appropriate (ie, concrete operational thinking) concepts with school-age patients, such as information related to what the patient can expect
* during the surgical process (eg, approximate time in surgery, recovery, return to the nit),
* regarding the location of the surgical incision, and
* regarding the appearance of postoperative surgical dressings.
The nurse should review the rationale and importance of implementing postoperative strategies, such as deep breathing exercises with the child.
The perioperative nurse offers the child the opportunity to select a scented oxygen mask (eg, cherry, grape, strawberry) for use during anesthesia induction in the OR. Encouraging the patient's participation in selecting a scented mask and providing concrete information related to the surgical process and postoperative strategies are examples of appropriate developmental strategies nurses can implement to aid in meeting the developmental needs of school-age patients (eg, gaining self-control, developing self-competence). The perioperative nurse then develops a care plan for the pediatric patient with SCD undergoing elective laparoscopic cholecystectomy (Table 1).
INTRAOPERATIVE PHASE
Perioperative team members transport the pediatric patient on a child-size stretcher to the OR suite and place the patient on a locked OR bed. The circulating nurse reassures the patient and provides simple explanations of the intraoperative equipment using concrete terms, such as explaining that the purpose of the OR bed strap is to ensure safety and prevent accidental falls rather than to tie the child down.
The circulating nurse incorporates distraction techniques appropriate for the school-age patient (eg, discusses hobbies, school activities, clubs, team sports) to minimize the emotional distress often experienced by children of this age group. The circulating nurse encourages the parents to accompany their child to the OR until after anesthesia induction to reduce the child's fears.
Anesthesia. The circulating nurse assists the anesthesia care provider during induction of general anesthesia and intubation of the child. The nurse either places the patient's IV line preoperatively in the pediatric unit or in the OR. The anesthesia care provider induces general anesthesia and places the endotracheal tube. After induction of anesthesia, the anesthesia care provider inserts an orogastric tube for decompression. After the child is intubated, a staff member escorts the parents to the parent surgical waiting room where they typically wait until their child's surgical procedure is complete.
Positioning and prepping. The circulating nurse initially positions the pediatric patient in the supine position on the OR bed and positions two video cameras at the head of the OR bed. The nurse evacuates the patient's urinary bladder via the Crede's maneuver (ie, massaging the bladder by pressing down on the anterior, superior surface of the abdomen).
The circulating nurse cleanses the patient's abdomen with an antiseptic solution. The pediatric surgeon, with the assistance of the scrub person, drapes the patient's surgical site. Depending on the patient's age, a four-cannula technique generally is used for the laparoscopic cholecystectomy procedure. During the initial steps of the procedure, the circulating nurse and anesthesia care provider rotate the patient and OR bed for improved visualization. The patient and bed are rotated into the reverse Trendelenburg's and left-dependent positions to aid in allowing the adjacent abdominal viscera to fall away from the surgical area. The surgeon performs lateral retraction of the junction of the infundibulum (ie, funnel-shaped passage or structure) of the gallbladder and cystic duct. (33) The primary benefit of using lateral retraction is the ability to reposition the cystic duct into a 90% orientation to the common bile duct versus an oblique or even parallel orientation. This minimizes the need for surgical manipulation by retraction. (34)
Risks. Surgery and general anesthesia are potential stressors for all children with SCD. Intraoperative complications may include
* transient hypoxia;
* hypothermia;
* dehydration;
* acidosis; (35)
* increased risk of reduced respiratory effort due to postoperative incisional pain, resulting in poor pulmonary toilet and hypoxia symptoms; (36) and
* bleeding diathesis.
Pediatric patients with SCD can experience bleeding diathesis and a sudden hemoglobin drop during the postoperative period even after an uneventful laparoscopic cholecystectomy procedure. (37) Erythrocyte transfusion therapy during the preoperative period, therefore, is recommended to increase the percentage of hemoglobin A to more than 65% of the total hemoglobin and a hematocrit of 35% to 45%. (38)
Physiological factors that influence the development of complications include
* patient immobility,
* hypothermia as a result of exposure to the cool surgical environment,
* hypoventilation, and
* pain.
Supportive perioperative interventions for the patient with SCD, therefore, include careful attention to ensuring adequate oxygenation, hydration, and acid-base balance. In addition, patients with SCD receive IV hydration therapy at a rate of one and one-half times the calculated maintenance amounts for 12 hours before elective surgery. Hydration therapy is continued into the postoperative period until the patient displays adequate oral intake, which usually occurs by the third postoperative day. (39) Supportive postoperative recommendations include careful attention to assessment of the patient's abdomen, and oxygen saturation and monitoring of the hematocrit and hemoglobin values at six hours after surgery and each morning for two consecutive days. (40)
Other recommended precautions are related to the risk of hypoxia and hypothermia. (41) The anesthesia care provider ensures that the patient receives 100% oxygenation before and after intubation and extubation and monitors the patient's body temperature to avoid hypothermia. The Circulating nurse maintains the room temperature at 80[degrees] F to 85[degrees] F (27[degrees] C to 29[degrees] C) during the procedure, ensures the patient is positioned properly, and is careful to determine that IV stability devices and dressings have not caused circulatory stasis.
LAPAROSCOPIC CHOLECYSTOMY PROCEDURE
The surgeon uses electrosurgery to make a 1-cm umbilical incision and dissect through the abdomen until the fascial tissue is entered. He or she then inserts the Veress insufflation needle into the abdomen and then places a 10-mm epigastric port. Using a 10-mm laparoscope, the surgeon visually inspects the patient's gallbladder. The anesthesia care provider rotates the bed into reverse Trendelenburg's and left-dependent position to help the adjacent viscera fall away from the surgical area. (42) The surgeon looks for adhesions and other abnormalities. He or she infiltrates the additional port sites with bupivicaine and uses electrosurgery to make incisions for three 5-mm ports
* at the anterior axillary line in the right costal margin,
* at the midclavicular line along the right costal margin, and
* under the epigastrium.
The surgeon places trocars and instruments into the 5-mm ports to grasp and elevate the gallbladder and then bluntly takes down any adhesions and grasps the infundibulum. The surgeon uses electrosurgery to remove the peritoneum from the gallbladder and then clear and reverse the triangle of Calot. The surgeon also inspects the cystic duct from its origin down to the gallbladder. He or she further divides the patient's peritoneum along the gallbladder to mobilize it before removing the cystic duct. The surgeon places two clips distal to the intended line of division and one on the cystic duct approximately 5 mm from its insertion into the common bile ducts. He or she transects the cystic duct and divides the cystic artery with electrosurgery before removing the gallbladder. The surgeon creates a small hole in the gallbladder to drain it with suction, which prevents bile leakage into the peritoneal cavity, before removing the gallbladder from the gallbladder bed. He or she pulls the gallbladder out through the umbilical port in an endoscopic specimen bag. The surgeon inspects the gallbladder and irrigates and aspirates the area until it is clear.
The surgeon removes all surgical instruments from the patient's abdomen and deflates the patient's abdomen by allowing the carbon dioxide to escape via the ports, after which he or she removes the ports. The surgeon closes the umbilical fascia with interrupted 2-0 braided absorbable polyglactin suture. The surgeon then infiltrates all surgical wounds with bupivicaine and closes the skin with subcuticular stitches of monofilament absorbable poliglecaprone. The surgeon uses tincture of benzoin and self-adhesive wound approximating strips to close the 5-mm port sites and applies antibiotic ointment and a sterile adhesive bandage strip on the patient's umbilicus.
POSTOPERATIVE CARE
The circulating nurse and anesthesia care provider transport the patient to the postanesthesia care unit (PACU) after the surgical procedure is completed. The circulating nurse gives report to the PACU nurse. After receiving report, the PACU nurse assesses the patient's vital signs, oxygen saturation level, level of consciousness, circulation, pain, IV site, fluid rate, and hydration status, as well as the status of the surgical site and dressing and all related monitoring equipment. The nurse also places warming blankets on the patient to enhance comfort and preserve the patient's body temperature.
Discharge. Pediatric patients with SCD usually are discharged four to six days after elective laparoscopic cholecystectomy. The pediatric surgical nurse provides in-depth discharge teaching to the parents about the child's recommended activity level and restrictions, pain management, and diet. He or she also discusses recommended follow-up management with the physician and the surgeon (Table 2).
POTENTIAL COMPLICATIONS
The major benefits of elective laparoscopic cholecystectomy include shorter hospitalization, decreased postoperative discomfort, a shorter interval before returning to normal activities, (43) and increased respiratory efforts. (44) Patients who have undergone this procedure, however, have a slightly increased risk of major bile duct injury (ie, 0.3% versus 0.2% for those who undergo traditional open cholecystectomy). (45) The primary complication identified is the risk of bile duct injury among adults (46), and bleeding diathesis among children with SCD. (47) It is recommended, therefore, that all children with SCD be monitored closely postoperatively, including having their hemoglobin and hematocrit assessed for 48 hours to 72 hours. Laparoscopic cholecystectomy also carries a small risk of complications for all patients related to required surgical treatments, such as anesthesia, blood transfusion, hemorrhage, and insufflation of the peritoneal cavity with carbon dioxide. (48)
CASE STUDY
Sarah, a 10-year-old African-American female with a history of SCD, was admitted to the pediatric unit at St Louis Children's Hospital with a suspected diagnosis of acute cholecystitis. After undergoing numerous diagnostic examinations, the physician confirmed diagnoses of acute cholecystitis, prolonged prothrombrin time, and multiple pigmented stones in the gallbladder. Hematology-oncology team members evaluated Sarah and initiated medical interventions, including pain management and vitamin K administration. Sarah recovered from the acute painful episode and was scheduled for elective laparoscopic cholecystectomy.
Sarah's pediatric nurse started an IV in Sarah's left anticubital fossa and began administering IV fluids (ie, 5% dextrose in 0.45% normal saline with 20 mEq potassium chloride) at 80 mL per hour in preparation for the scheduled surgical procedure. The nurse also administered prophylactic antibiotic therapy (ie, 1 g IV cefoxitin sodium) every eight hours for three doses in preparation for the surgical procedure.
The elective laparoscopic cholecystectomy procedure proceeded uneventfully, and although the surgeon identified some adhesions from the omentum to the gallbladder, she detected no other abnormalities except for mild hepatomegaly. The surgeon bluntly dissected all detected adhesions from the omentum on the duodenum into the gallbladder and dissected the gallbladder free. She was unable to locate Sarah's dominant artery; however, small branches of this artery were identified. While mobilizing and transecting the cystic duct, the surgeon determined that one of the distally placed clips appeared not to have approximated appropriately; therefore, the surgeon placed an endoloop proximal to the clips on the cystic duct stump. She removed the gallbladder without difficulty and closed the incisions.
Sarah was transferred via pediatric stretcher to the PACU, and after she recovered for 60 minutes, PACU nurses transferred Sarah to the pediatric surgical unit. Sarah's pediatric surgical unit nurse completed an admission assessment and then monitored Sarah's vital signs every four hours until discharge. During the surgical procedure and the postoperative phase, the nurse managed Sarah's pain with a continuous IV infusion via a computerized patient-controlled anesthesia (PCA) pump of 1 mg per mL of morphine sulfate (MS) at a rate if 0.5 mg per hour. In the event that Sarah experienced MS-associated side effects, such as pruritus, the nurse had orders to administer 25 mg diphenhydramine hydrochloride IV or by mouth (PO) every six hours as needed. If the pruritus was unresponsive to diphenhydramine, Sarah's nurse could administer 2 mg of IV nalbuphine every one to two hours as needed. Additionally, the nurse had orders to treat other side effects associated with MS therapy, such as nausea and vomiting, with 4 mg IV ondansetron every six hours or 6 mg IV metaclopramide hydrochloride every six hours as needed. Fortunately, Sarah did not experience side effects typically associated with MS.
On the first postoperative day, Sarah was not allowed any oral intake for 24 hours. On her second postoperative day, the nurse slowly advanced Sarah's diet beginning with clear liquids, increasing to a normal diet as tolerated. The nurse assisted Sarah out of bed on the second postoperative day and encouraged her to increase her activity as tolerated, offering assistance as needed. The nurse discontinued Sarah's PCA, IV fluids, and IV medications during the second day and managed Sarah's pain with PO oxycodone 5 mg or acetaminophen with codeine every four to six hours as needed. The nurse instructed Sarah and her parents about discharge instructions. He also instructed Sarah's parents to make Sarah's follow-up appointment in approximately four to six weeks. Overall, this patient experienced an uneventful recovery period after the surgical procedure.
SUMMARY
Elective laparoscopic cholecystectomy in children has been described as a safe and effective alternative to the traditional cholecystectomy surgical procedure because of a shortened hospital stay and improved postoperative recovery. (49) One of the significant benefits of laparoscopic cholecystectomy for children with SCD is reduced postoperative pain, which improves pulmonary toilet and decreases risk of pneumonia and vaso-occlusive events. (50) Other identified postoperative benefits include reduced risk of postoperative ileus, smaller incision, and decreased keloid formation, resulting in an improved body image for young patients with SCD. (51)
Current guidelines for children with SCD experiencing symptoms of cholelithiasis recommend elective laparoscopic cholecystectomy to prevent complications such as acute cholecystitis and the risk of emergency surgery for an unprepared patient. (52) The cholecystectomy procedure, whether traditional or laparoscopic, does not cure SCD. The elective laparoscopic cholecystectomy procedure, however, offers a planned surgical intervention, reducing the risk of complications associated with emergency cholecystectomy. For school-age patients with SCD, these benefits minimize feelings of fear and anxiety associated with Surgery and hospitalization and foster a sense of self-control.
NOTES
(1.) V L Hendricks-Ferguson, M A Nelson, "Laparoscopic splenectomy for splenic sequestration crisis," AORN Journal 71 (April 2000) 820-834.
(2.) R E Ware et al, "Diagnosis and management of common bile duct stones in patients with sickle hemoglobinopathies," Journal of Pediatric Surgery 27 (May 1992) 572-575.
(3.) D De Caluwe, U Akl, M Corbally, "Cholecystectomy versus cholecystolithotomy for cholelithiasis in childhood: Long-term outcome," Journal of Pediatric Surgery 36 (October 2001) 1518-1521.
(4.) R Rudolph, J S Williams, "Cholecystectomy in patients with sickle cell disease: Experience at a regional hospital in southeast Georgia," Journal of the National Medical Association 84 (August 1992) 692-696.
(5.) Ibid.
(6.) E P Tagge et al, "Impact of laparoscopic cholecystectomy on the management of cholelithiasis in children with sickle cell disease," Journal of Pediatric Surgery 29 (February 1994) 209-213; A J Jawad et al, "Laparoscopic cholecystectomy for cholelithiasis during infancy and childhood: Cost analysis and review of current indications," World Journal of Surgery 22 (January 1998) 69-74.
(7.) Rudolph, Williams, "Cholecystectomy in patients with sickle cell disease: Experience at a regional hospital in southeast Georgia," 692-696.
(8.) E A Pomfret, J J Pomposelli, R L Jenkins, "Surgical approaches to diseases of the biliary system," in Schiff's Diseases of the Liver, eighth ed, E R Schiff, M F Sorrell, W C Maddrey, eds (Philadelphia: Lippincott-Raven Publishers, 1999) 693-717.
(9.) E A Shaffer, "Gallbladder disease," in Pediatric Gastrointestinal Disease: Pathophysiology, Diagnosis, Management, third ed, W A Walker et al, eds (Hamilton, Ontario: B C Decker, 2000) 1291-1311.
(10.) C F Gholson et al, "Sequential endoscopic/laparoscopic management of sickle hemoglobinopathy-associated cholelithiasis and suspected choledocholithiasis," Southern Medical Journal 88 (November 1995) 1131-1135; Jawad et al, "Laparoscopic cholecystectomy for cholelithiasis during infancy and childhood: Cost analysis and review of current indications," 69-74.
(11.) G W Holcomb, J B Pietsch, "Gallbladder disease and hepatic infections," in Pediatric Surgery, vol two, fifth ed, J A O'Neill et al, eds (St Louis: Mosby, 1998) 1495-1511.
(12.) Rudolph, Williams, "Cholecystectomy in patients with sickle cell disease: Experience at a regional hospital in southeast Georgia," 692-696.
(13.) N D Duncan, A H McDonald, D I G Mitchell, "Cholecystectomy in Jamaican children with homozygous sickle-cell disease," Tropical Doctor 30 (October 2000) 214-216.
(14.) Rudolph, Williams, "Cholecystectomy in patients with sickle cell disease: Experience at a regional hospital in southeast Georgia," 692-696.
(15.) Duncan, McDonald, Mitchell, "Cholecystectomy in Jamaican children with homozygous sickle-cell disease," 214-216.
(16.) Shaffer, "Gallbladder disease," 1291-1311.
(17.) D L Nahrwold, "The biliary system," in Textbook of Surgery: The Biological Basis of Modern Surgical Practice, 15th ed, D C Sabiston, H K Lyerly, eds (Philadelphia: W B Saunders Co, 1997) 1117-1125.
(18.) Ibid
(19.) Shaffer, "Gallbladder disease," 1291-1311.
(20.) Gholson et al, "Sequential endoscopic/laparoscopic management of sickle hemoglobinopathy-associated cholelithiasis and suspected choledocholithiasis," 1131-1135.
(21.) Holcomb, Pietsch, "Gallbladder disease and hepatic infections," 1495-1511; T M Walker, I R Hambleton, G R Serjeant, "Gallstones in sickle cell disease: Observations from the Jamaican cohort study," The Journal of Pediatrics 136 (January 2000) 80-85.
(22.) Shaffer, "Gallbladder disease," 1291-1311.
(23.) D M Heuman, W Y Wassef, Z R Vlahcevic, "Gallstones," in Schiff's Diseases of the Liver, eighth ed, E R Schiff, M F Sorrell, W C Maddrey, eds (Philadelphia: Lippincott-Raven Publishers, 1999) 631-647.
(24.) Ibid.
(25.) Ibid
(26.) Shaffer, "Gallbladder disease," 1201-1311.
(27.) Heuman, Wassef, Vlahcevic, "Gallstones," 631-647; Jawad et al, "Laparoscopic cholecystectomy for cholelithiasis during infancy and childhood: Cost analysis and review of current indications," 69-74.
(28.) Ibid.
(29.) A H Al-Salem et al, "Laparoscopic versus open cholecystectomy in children," Pediatric Surgery International 12 (October1997) 587-590; A H Al-Salem, S Qaisruddin, "The significance of biliary sludge in children with sickle cell disease," Pediatric Surgery International 13 (January 1998) 14-16; Duncan, McDonald, Mitchell, "Cholecystectomy in Jamaican children with homozygous sickle-cell disease," 214-216; R M Hatley et al, "Laparoscopic cholecystectomy in children with sickle cell disease," The American Surgeon 61 (February 1995) 169-171; Holcomb, Pietsch, "Gallbladder disease and hepatic infections," 1495-1511; Tagge et al, "Impact of laparoscopic cholecystectomy on the management of cholelithiasis in children with sickle cell disease," 209-213.
(30.) R Ware et al, "Laparoscopic cholecystectomy in young patients with sickle hemoglobinopathies," The Journal of Pediatrics 120 (January 1992) 58-61.
(31.) J Piaget, The Theory of Stages of Cognitive Development (New York: McGraw-Hill, 1969).
(32.) E Erikson, Childhood and Society, second ed (New York: Norton Press, 1963).
(33.) Nahrwold, "The biliary system," 1117.
(34.) Holcomb, Pietsch, "Gallbladder disease and hepatic infections," 1495-1511.
(35.) Ware et al, "Laparoscopic cholecystectomy in young patients with sickle hemoglobinopathies," 58-61.
(36.) Ibid.
(37.) Hatley et al, "Laparoscopic cholecystectomy in children with sickle cell disease," 169-171.
(38.) Ware et al, "Elective cholecystectomy in children with sickle hemoglobinopathies: Successful outcome using a preoperative transfusion regimen," 17-22.
(39.) Ibid.
(40.) Hatley et al, "Laparoscopic cholecystectomy in children with sickle cell disease," 169-171.
(41.) Ware et al, "Laparoscopic cholecystectomy in young patients with sickle hemoglobinopathies," 58-61.
(42.) Holcomb, Pietsch, "Gallbladder disease and hepatic infections," 1495-1511.
(43.) G W Holcomb, D O Olsen, K W Sharp, "Laparoscopic cholecystectomy in the pediatric patient," Journal of Pediatric Surgery 26 (October 1991) 1186-1190; E Leandros et al, "Laparoscopic or open cholecystectomy in patients with sickle cell disease: Which approach is superior?" The European Journal of Surgery 166 (November 2000) 859-861.
(44.) Hatley et al, "Laparoscopic cholecystectomy in children with sickle cell disease," 169-171.
(45.) Pomfret, Pomposelli, Jenkins, "Surgical approaches to diseases of the biliary system," 693-717.
(46.) Ibid.
(47.) Hatley et al, "Laparoscopic cholecystectomy in children with sickle cell disease," 169-171.
(48.) Walker, Hambleton, Serjeant, "Gallstones in sickle cell disease: Observations from the Jamaican cohort study," (January 2000) 80-85.
(49.) Hatley et al, "Laparoscopic cholecystectomy in children with sickle cell disease," 169-171.
(50.) Ibid
(51.) Ware et al, "Laparoscopic cholecystectomy in young patients with sickle hemoglobinopathies," 58-61.
(52.) Ibid.
Home Study Program
TREATMENT OF CHOLELITHIASIS IN CHILDREN WITH SICKLE CELL DISEASE
The article "Treatment of cholelithiasis in children with sickle cell disease," is the basis for this AORN Journal independent study. The behavioral objectives and examination for this program were prepared by Rebecca Holm, RN, MSN, CNOR, clinical editor, with consultation from Susan Bakewell, RN, MS, education program professional, Center for Perioperative Education.
A minimum score of 70% on the multiple-choice examination is necessary to earn 2.3 contact hours for this independent study. Participants receive feedback on incorrect answers. Each applicant who successfully completes this study will receive a certificate of completion. The deadline for submitting this study is June 30, 2006.
Send the completed application form, multiple-choice examination, learner evaluation, and appropriate fee to
AORN Customer Service
c/o Home Study Program
2170 S Parker Rd, Suite 300 Denver, CO 80231-5711
or fax the information with a credit card number to (303) 750-3212.
BEHAVIORAL OBJECTIVES
After reading and studying the article on treatment of cholelithiasis in children with sickle cell disease (SCD), the nurse will be able to
(1) explain how a child with SCD may suffer from cholelithiasis,
(2) describe the gallbladder according to SCD,
(3) identify treatment options for cholelithiasis,
(4) define developmental theory in regard to prominent child psychologists,
(5) explain the nursing care provided during the preoperative phase of a cholecystectomy procedure performed on a child with SCD,
(6) discuss the intraoperative phase of the procedure, and
(7) elaborate on the postoperative experience of a child with SCD undergoing cholecystectomy.
This program meets criteria for CNOR and CRNFA recertification, as well as other continuing education requirements.
Examination
TREATMENT OF CHOLELITHIASIS IN CHILDREN WITH SICKLE CELL DISEASE
1. Primary symptoms of sickle cell disease (SCD) include
a. jaundice and hepatomegaly.
b. chronic hemolytic anemia and tissue damage.
c. hypoproteinemia and pelegra.
d. dysphagia and hemoptysis.
2. -- pigment gallstones are small, hard, and spiculated (ie, sharp body with a needle-like points) and made of calcium bilirubinate, inorganic salts (eg, calcium phosphate), and calcium carbonate.
a. Black
b. Brown
c. Mixed
d. Yellow
3. The purpose of erythrocyte transfusion therapy is to
a. terminate bleeding by mechanical or chemical means or by vasoconstriction, platelet aggregation, and thrombin and fibrin synthesis.
b. form and develop various types of blood cells using fresh blood plasma or serum.
c. reduce the percentage of hemoglobin S and increase the hemoglobin concentration to greater than 10 gm per dL.
d. remove impurities or wastes from the blood with diffusion and ultrafiltration and then return the blood to the patient's circulation.
4. Children with SCD who undergo cholecystectomy have a higher risk of developing all of the following except
a. ascending cholangitis.
b. choledocholithiasis.
c. acute cholecystitis.
d. cholangioma.
5. Psychologist Erik Erikson characterized children ages six to 12 as being in the -- -- stage of psychosocial development.
a. autonomy versus shame and doubt
b. initiative versus guilt
c. industry versus inferiority
d. identity versus role confusion
6. Encouraging the patient's participation in selecting a scented mask is an example of an appropriate developmental strategy that nurses can implement to aid in meeting the developmental needs of a school-age child.
a. true
b. false
7. All of the following interactions are appropriate for the nursing diagnosis "Fear of the unknown related to undergoing cholecystectomy" except
a. explains the purpose of intraoperative equipment in age-appropriate terms.
b. explains how cholecystectomy is a definitive treatment for cholelithiasis.
c. incorporates distraction techniques appropriate for the school-age patient by discussing interests.
d. encourages the patient to select a scented oxygen mask for use during anesthesia induction in the OR.
8. Surgery and general anesthesia are potential stressors for children with SCD. Intraoperative complications include all of the following except
a. organ system reserve depletion.
b. hypothermia and transient hypoxia.
c. dehydration.
d. bleeding diathesis.
9. Submersion of the incision is allowed immediately after surgery because the incision is closed with collodion.
a. true
b. false
10. Benefits of elective laparoscopic cholecystectomy in children with SCD include all of the following except
a. reduced postoperative pain, which improves pulmonary toilet and decreases risk of pneumonia and vase-occlusive events.
b. shortened hospital stay and improved postoperative recovery.
c. reduced risk of postoperative ileus, smaller incision, and decreased keloid formation, resulting in an improved body image for young patients with SCD.
d. easier observation of the abdominal cavity than is possible with an open procedure.
AORN is accredited as a provider d continuing nursing education by the American Nurses Credentialing Center's Commission on Accreditation. AORN recognizes these activities as continuing education for RNs. This recognition does not imply that AORN or the American Nurses Credentialing Center approves or endorses products mentioned in the activity. AORN is provider-approved by the California Board of Registered Nursing, Provider Number CEP 13019.
Verna Hendricks-Ferguson, RN, DNSc, CS, is an associate professor at Jewish Hospital, College of Nursing and Allied Health, Edwardsville, Ill.
Martha A. Nelson, RN, BS, CPNP, is the pediatric nurse practitioner and sickle cell patient coordinator at St Louis Children's Hospital.
COPYRIGHT 2003 Association of Operating Room Nurses, Inc.
COPYRIGHT 2003 Gale Group