Sickle cell disease (SCD) is an inherited blood disorder that causes the bone marrow to produce red blood cells with defective hemoglobin, hemoglobin S (sickled hemoglobin). Leg ulcers are the most common cutaneous manifestation of SCD.1 These ulcers are characterized by an indolent, intractable course, typically healing up to 16 times slower than venous ulcers.2 A patient who experiences his or her first sickle cell ulcer is likely to ulcerate again: Approximately 97% of healed sickle cell ulcers will recur in less than 1 year.3 Due to the recalcitrant nature of these ulcers, patients may experience significant disfigurement, social isolation, and loss of income.
The incidence of leg ulcers in patients with SCD ranges from 25.7% to 75%.3,4 Risk factors for the development of ulcers include being older than 20 years, being male, having a lower level of fetal hemoglobin and a hemoglobin level less than 6 g/dL, having antithrombin III deficiency, possessing certain human leukocyte antigens (HLA), having thrombocytosis, and living in certain geographic areas.1'5'6 History of a sickle cell leg ulcer carries a 23-fold increased risk of developing future ulcerations; having 1 active ulcer carries a 146-fold increased risk.1 Prognosis improves in these patients, however, with the presence of sickle/beta-thalassemia and sickle C hemoglobin.5
Pathogenesis
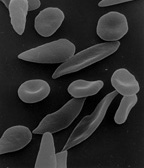
Although the pathogenesis of leg ulcers in SCD has not been completely elucidated, several theories have been offered to explain this phenomenon. In sickle cell disease, the amino acid valine is substituted for glutamic acid in the beta-hemoglobin chain of hemoglobin, leading to the polymerization of hemoglobin when hemoglobin is deoxygenated. This results in the sickling, or misshaping, of red blood cells (Figure 1).1,7,8 Sickled red blood cells are rigid and inflexible, which allows them to become lodged within smaller blood vessels and causes vascular obstruction.1,9-12 Once obstruction occurs, ischemia ensues and tissue necrosis results.
In addition, injury to red blood cells leads to the upregulation of integrins, which act as adhesion molecules on endothelial cells. This upregulation promotes platelet aggregation, adherence of sickled cells to the endothelium, slow blood flow, and additional occlusion of the vessels.13 Furthermore, granulocytes interact with the sickled cells, leading to the release of injurious cytokines, which cause added tissue injury.
Other factors have been implicated in ulcer formation in SCD. For example, trauma is believed to cause sickle cell ulcers by stimulating the sickling of red blood cells and perpetuating the previously described cascade.1,12 In addition, venous incompetence may contribute to the development of sickle cell ulcers. Venous incompetence results in venous hypertension and the elevation of venous pressures,14,15 which predisposes patients to the development of leg ulcers. Anemia may also contribute to hypoxia, causing ischemia and tissue necrosis.1,12 If thrombocytosis exists in patients with SCD-and it often does due to bone marrow stimulation-blood viscosity increases, promoting thrombosis and vascular occlusion and resulting in subsequent tissue necrosis.1 Antithrombin III deficiency, which promotes vascular thrombosis, has also been implicated in the pathogenesis of leg ulcers in SCD.1'16
Certain geographic locations, such as Jamaica, have reported a high incidence of sickle cell leg ulcers (75%); countries such as Saudi Arabia have reported almost zero incidence.1,17 This suggests that either a genetic or environmental predisposition exists for this condition. In addition, possession of certain types of HLA, such as HLA-B35 and Cw4, have been found to be related to the development of leg ulcers in SCD.1,17
Diagnosis
Sickle cell ulcers normally occur in areas with less subcutaneous fat, thin skin, and decreased blood flow. Common sites include the anterior tibial area, dorsum of the foot, Achilles tendon area, and ankles, with the medial malleolus being more affected than the lateral malleolus (Figures 2 and 3).1,4,10 Sickle cell ulcers classically appear as round, punchcd-out ulcers with raised margins, deep bases, and necrotic slough (Figure 4). Surrounding brown hyper-pigmentation and scaling-reminiscent of venous ulcers-may also be present.1 Multiple ulcers or scarring from healed ulcers may be found in the vicinity. Patients usually complain of extreme tenderness or pain at the site of the ulcer. This is because sickled cells lead to tissue death, which is painful. In essence, sickle cell ulcers represent a type of ischemie ulcer.
A biopsy of the ulcer is nonspecific; however, sickled red blood cells may be visualized within the dermal blood vessels. Laboratory analysis for patients with suspected sickle cell ulcers includes peripheral smear to visualize the pathognomonic sickled red blood cells, a complete blood count to determine the level of anemia, and hemoglobin electrophoresis to measure the levels of hemoglobin A, S, and F (Table I).18'19 Several types of hemoglobin exist, with hemoglobin A being the normal variant. Hemoglobin F is the fetal hemoglobin, which is fairly resistant to sickling.
Three hemoglobinopathies arise due to mutations in the beta-globin chain of hemoglobin molecule. Hemoglobin S results from an amino acid substitution of valine for glutamic acid in the beta-globin chain. Hemoglobin C and E result from the same amino acid substitution (lysine for glutamic acid). However, they occur at different locations in the beta-globin chain, all of which vary, based on the severity of the anemia they produce.
The white blood cell count may also be elevated in patients with infected sickle cell ulcers.19 Liver and renal function may be compromised, manifesting as elevated blood urea nitrogen (BUN) and creatinine levels. Urinalysis may detect early renal disease, which is characterized by proteinuria and microhematuria. Elevated levels of fibrin D-dimers have also been associated with sickle cell crises.20 Decreased folate, iron, and vitamin B12 levels may be seen in these patients.18 A high homocysteine level may occur, and it may represent a risk factor for cerebrovascular accidents.
Treatment
Therapy for sickle cell leg ulcers encompasses 3 broad areas: prevention, treatment of existing ulcers, and treatment of infection.1 Because trauma is an inciting factor in these ulcers, simple measures-such as wearing properly fitting shoes, using insect repellent, and promptly treating any minor trauma-are essential components of prevention. Given the risk of concurrent venous or lymphatic disease, the use of support stockings, leg elevation, and sodium restriction may aid in decreasing edema and preventing ulcer formation. Other important prevention strategies include proper hygiene and liberal use of emollients to reduce drying and cracking of the skin.
Treatment options for sickle cell leg ulcers can be divided into 4 categories: topical treatments, dressings, surgical interventions, and systemic medications (Table 2). 1-5,9,12,16,21-32 In randomized controlled trials, topical triple antibiotic ointments have been shown to heal sickle cell ulcers and treat concurrent infections.1'21 A double-blind, placebo-controlled trial showed rapid healing of sickle cell ulcers with the use of a synthetic matrix comprised of arginine-glycine-aspartic acid tripeptide bound to hyaluronate.1 This formulation was theorized to work by stimulating the production of granulation tissue and subsequent keratinocyte migration.
A number of anecdotal reports have successfully treated sickle cell ulcers with the use of topical oxygen with a tent.1 In addition, Ballas22 reported that 2 patients healed faster and with less pain when treated with either oxycodone dissolved in water and mixed with debriding ointment or meperidine dissolved in water and mixed with lidocaine (Xylocaine) ointment.
A variety of dressings have been used to heal sickle cell ulcers. The use of an Unna's boot, a zinc-oxide impregnated dressing, controlled edema in patients with sickle cell ulcers and led to subsequently faster healing.5'12 Dressings may be used in conjunction with elastic compression bandages for controlling edema and have the advantage of requiring weekly or twice weekly dressing changes, minimizing cutaneous trauma, DuoDERM, (ConvaTec, A Bristol-Myers Squibb Company; Skillman, NJ), a hydrocolloid dressing that protects newly forming epithelium while preventing infection, has also been used alone and in conjunction with an Unna's boot or compression stockings to aid in the healing of leg ulcers in SCD.1'9 However, DuoDERM was not found to be superior in a randomized controlled trial that compared Solcoseryl (Merck Ltd, Darmstadt Germany), DuoDERM, and conventional treatment with wet dressings.28 Solcoseryl is a deproteinized extract of calf blood that has been reported to stimulate tissue oxygen utilization, thereby promoting wound healing. In the study,28 Solcoseryl was found to increase healing rates of sickle cell ulcers. Reindorf et al4 reported successful use of Collastat (Kendall, Mansfield, MA), a collagen matrix dressing, in the treatment of sickle cell leg ulcers in 2 patients. The dressing was reapplied every 4 weeks, with all ulcers healing within 3 months. Fried et al23 used Omiderm (Omiderm Ltd,Yavne, Israel), a transparent dressing with elastic properties, to rapidly heal leg ulcers in their patients.
Surgical interventions for sickle cell ulcers include debridement and the use of myocutaneous flaps and split-thickness skin grafts. Debridement with dressings or debriding ointments enables the removal of necrotic slough.1 Autologous split-thickness skin grafts or pinch grafts are advocated for the use of recalcitrant ulcers (Figures 5 and 6).1'5'12 Most grafts fail, however, because of the inherent circulatory difficulties and vascular insufficiency in the areas of these ulcers. To increase the chance of skin survival after transplantation, the use of myocutaneous flaps is encouraged because they carry their own blood supply to the area of ulceration.3'33'34 Some authors have used anticoagulation in conjunction with myocutaneous flap placement to promote flap survival.33'34
Gordon and Bui2 reported a patient with long-standing sickle cell ulcers who healed within 6 weeks with the use of Apligraf (Organogenesis, Inc, Canton, MA), a bilayered skin equivalent manufactured from neonatal foreskin keratinocytes and fibroblasts. The patient experienced no recurrence after 33 weeks. Others have reported less success using cultured autologous epidermal grafts.35
Due to the intractable nature of sickle cell ulcers, data from randomized controlled trials are scant, except those concerned with the use of oral zinc sulfate.24 Zinc deficiency is common in patients with SCD,1 and the addition of oral zinc sulfate has improved the anemia of SCD. Serjeant et al24 found significant improvement in ulcers related to SCD when patients were treated with 220 mg oral zinc sulfate 3 times a day. Numerous reports have supported the use of a number of different blood products and systemic agents, such as pentoxifylline, antithrombin III concentrate, hydroxyurea (with or without erythropoietin), L-carnitine, arginine butyrate, and periodic transfusions.1'5'6'9'12,16,25-27
Although no controlled trial has examined the efficacy of transfusion therapy, many recalcitrant leg ulcers are now managed this way.1 Transfusions have long been used to treat the anemia and crises associated with SCD. The goal of this therapy for sickle cell ulcers is to transfuse enough packed red blood cells to increase the oxygen-carrying capacity of blood by raising the hemoglobin to 10 g/dL and reducing the hemoglobin S to less than 30%.1,13,36This therapy is continued until the ulcer heals or is stopped after 6 months if no healing occurs. However, 20% to 30% of patients become alloimmunized after many transfusions.13 In addition, iron overload may occur with repeat transfusions.
The use of pentoxifylline has been shown to heal venous leg ulcers in several randomized controlled trials; however, data for its use to treat sickle cell ulcers is scant. Pentoxifylline has been effective in vasoocclusive crises associated with sickle cell anemia by decreasing the frequency of the crises, decreasing occurrence of acute chest syndrome, decreasing the need for transfusions, and increasing the level of fetal hemoglobin.29 Frost and Treadwell25 reported 1 case of sickle cell ulcers treated successfully with pentoxifylline. Pentoxifylline is believed to work by decreasing the sickling of red blood cells, increasing erythrocyte deformability, increasing leukocyte flexibility, inhibiting platelet aggregation, reducing blood viscosity, and decreasing plasma fibrinogen levels.1'25
Antithrombin III concentrate and heparin were used to successfully heal a leg ulcer in a patient who was found to have concurrent SCD and antithrombin III deficiency.16 The ulcer healed in 6 weeks with no recurrence al 6 months.
The use of hydroxyurea, with or without the concurrent use of erythropoietin, has been utilized in patients with sickle cell anemia to increase the fetal hemoglobin level; to decrease platelet, neutrophil, and monocyte levels; and to enrich red blood cells.30-13 Hydroxyurea has been demonstrated to aid in the healing of recalcitrant leg ulcers in patients with SCD.1'9'12 However, increased incidence of ulceration has been associated with the use of hydroxyurea.30'31 Erythropoietin has been used in the treatment of sickle cell ulcers because it stimulates proliferation of red blood cell precursors and potentially acts as a growth factor for nonhematologic tissue.32
L-carnitine, a cofactor for oxidation of fatty acids in the mitochondria, increases adenosine triphosphate and energy production and has demonstrated efficacy in the treatment of ischeacutemic heart disease, peripheral arterial disease, and vasculopathic leg ulcers.26 It has been shown in case reports to aid in healing of sickle cell ulcers; however, data from a randomized controlled trial showed no improvement in ulcer healing with its use.26 Arginine butyrate, a fatty acid that aids in the synthesis of fetal hemoglobin, was used to completely heal one patient's ulcers in 6 weeks.27 No recurrence was noted after 6 months.
Pain management is critically important in the treatment of patients with SCD.18 Agents most commonly used include nonopioid analgesics, such as acetaminophen, nonsteroidal anti-inflammatory agents and cyclooxygenase-2 (COX-2) inhibitors; opioid analgesics, such as codeine, morphine, fentanyl, and methadone; and adjuvants, such as antihistamines, antidepressants, and anticonvulsants.
References
1. Eckman JR. Leg ulcers in sickle cell disease. Hematol Oncol Clin North Am 1996;10:1333-44.
2. Gordon S, BuI A. Human skin equivalent in the treatment of chronic leg ulcers in sickle cell disease patients. J Am Podiatr Med Asset 2003;93:240-1.
3. Khouri RK, Upton J. Bilateral lower limb salvage with free flaps in a patient with sickle cell ulcers. Ann Plast Surg 1991;27:574-6.
4. Reindorf CA, Walker-Jones D, Adekile AD1 Lawal O, Oluwole SF. Rapid healing of sickle cell legs ulcers treated with collagen dressing. J Natl Med Assoc 1989;81:866-8.
5. Koshy M, Entsuah R, Koranda A, et al. Leg ulcers in patients with sickle cell disease. Blood 1989:74:1403-8.
6. Ballas SK. Sickle cell anemia: progress in pathogenesis and treatment. Drugs 2002:62:1143-72.
7. Steinberg MH, Rodgers GP. Pathophysiology of sickle cell disease: role of cellular and genetic modifiers. Semin Hematol 2001;38:299-306.
8. Steinberg MH, Brugnara C. Pathophysiological-based approaches to treatment of sickle cell disease. Annu Rev Med 2003:54:89-112.
9. Cackovic M, Chung C, Bolton LL, Kerstein MD. Leg ulceration in sickle cell patient. J Am Coll Surg 1998:187:307-9.
10. Morgan AG. Sickle cell leg ulcers, lnt J Dermatol 1985:24:643-4.
11. Gabuzda TG. Sickle cell leg ulcers: current pathophysiologic concepts, lnt J Dermatol 1975:14:322-5.
12. al-Momen AK. Recombinant human erythropoietin-induced rapid healing of a chronic leg ulcer in a patient with sickle cell disease. Acta Haematol 1991 ;86:46-8.
13. Steinberg MH. Management of sickle cell disease. N Engl J Med 1999;340:1021-30.
14. Clare A, FitzHenley M, Harris J, Hambleton I, Serjeant GR. Chronic leg ulceration in homozygous sickle cell disease: the role of venous incompetence. Br J Dermatol 2002;119:567-71.
15. Shekarappa RJ, Ruiz-Montero J. Chronic non-healing ulcers. Am Fam Physician 1999;59:31b3-4.
16. Cacciola E, Musso R, Giustolisi R, Cacciola E, Alessi M. Blood hypercoagulability as a risk factor for leg ulcers in sickle cell disease. Blood 1990; 75:2467-8.
17. Ofosu MD, Castro O, Alarif L. Sickle cell leg ulcers are associated with HLA-B35 and Cw4. Arch Dermatol 1987:123:482-4.
18. Ballas SK. Sickle cell disease: current clinical management. Semin Hematol 2001;38:307-14.
19. Wethers DL Sickle cell disease in childhood. Part I. Laboratory diagnosis, pathophysiology and health maintenance. Am Fam Physician 2000;62:1013-20,1027-8.
20. Devine DV, Kinney TR, Thomas PF, Rosse WF, Greenberg CS. Fragment D-dimer levels: an objective marker of vaso-occlusive crisis and other complications of sickle cell disease. Blood 1986;68:317-19.
21. Baum KF, MacFarlane DE, Maude GH, Serjeant GR. Topical antibiotics in chronic sickle cell leg ulcers. Trans R Soc Trop Med Hyg 1987:81:847-9.
22. Ballas SK. Treatment of painful sickle cell leg ulcers with topical opioids. Blood 2002;99:1096.
23. Fried M, Golan J, Moshe F. Treatment of leg ulcers in sickle cell disease. Blood 1990;75:2467.
24. Serjeant GR, Galloway RE, Gueri MC. Oral zinc sulphate in sickle-cell ulcers. Lancet 1970;2:891-2.
25. Frost ML, Treadwell P. Treatment of sickle cell leg ulcers with pentoxifylline. lnt J Dermatol 1990;29:375-6.
26. Serjeant BE, Harris J, Thomas P, Serjeant GR. Propionyl-L-carnitine in chronic leg ulcers of homozygous sickle cell disease: a pilot study. J Am Acad Dermatol 1997;37(3 Pt 1):491-3.
27. Sher GD, Olivieri NF. Rapid healing of chronic leg ulcers during arginine butyrate therapy in patients with sickle cell disease and thalassemia. Blood 1994;84 2378-80.
28. La Grenade L, Thomas PW, Serjeant GR. A randomized controlled trial of Solcoseryl and DuoDerm in chronic sickle-cell ulcers. West Indian Med J 1993;42:121-3.
29. Ward A, Clissold SP. Pentoxifylline. A review of its pharmacodynamic and pharmacokinetic properties, and its therapeutic efficacy. Drugs 1987;34:50-97.
30. Loukopoulos D, Voskaridou E, Kalotychou V, Schina M, Loutradi A, Theodoropoulos I. Reduction of the clinical severity of sickle cell/beta-thalassemia with hydroxyurea: the experience of a single center in Greece. Blood Cells Mol Dis 2000:26:453-66.
31. Kersgard C, Osswald MB. Hydroxyurea and sickle cell leg ulcers. Am J Hematol 2001:68:215-6.
32. Chung C, Cackovic M, Kerstein MD. Leg ulcers in patients with sickle cell disease. Adv Wound Care 1996;9:46-50.
33. Spence RJ. The use of a free flap in homozygous sickle cell disease. Plast Reconstr Surg 1985:76:616-9.
34. Richards RS, Bowen CV, Glynn MF. Microsurgical free flap transfer in sickle cell disease. Ann Plast Surg 1992;29:278-81.
35. Hefton JM, Caldwell D, Biozes DG, Balin AK, Carter DM. Grafting of skin ulcers with cultured autologous epidermal cells. J Am Acad Dermatol 1986;14:399-405.
36. Claster S, Vichinsky EP. Managing sickle cell disease. Br Med J 2003:327:1151-5.
Jennifer T. Trent, MD, and Robert S. Kirsner, MD, PhD
Jennifer T. Trent, MD, is a Resident in the Department of Dermatology and Cutaneous Surgery, University of Miami School of Medicine, Miami, FL. Robert S. Kirsner, MD, PhD, is Associate Professor, Department of Dermatology and Cutaneous Surgery and Department of Epidemiology and Public Health, University of Miami School of Medicine, Miami, FL, and Chief of Dermatology, Veterans Administration Medical Center, Miami, FL.
Copyright Springhouse Corporation Oct 2004
Provided by ProQuest Information and Learning Company. All rights Reserved