Context.-Magnetic resonance imaging of bone marrow in homozygous sickle cell disease (hemoglobin [Hb] SS) shows nonhomogeneous, mottled signals that increase with age and number of crises. The pattern of these signals is reminiscent of the underlying vascular architecture, but histopathology of this tissue has not been adequately studied.
Objective.-To elucidate the histopathology of blood vessels in the bone marrow in sickle cell disease.
Design.-Retrospective histochemical morphometric study of bone marrow arteries by point counting in HbSS (13 cases) and sickle cell Hb C (HbSC) (8 cases) compared to nonanemic normal controls (HbAA) (10 cases). All patients were nondiabetic, normotensive, younger than 37 years, and matched for age group.
Results.-The mean point count for perivascular fibrous tissue was significantly greater in the HbSS group (P
Conclusion.-In sickle cell disease, arterial vessels in the bone marrow show significantly increased fibrous connective tissue and changes in muscle that vary with age and vessel size.
(Arch Pathol Lab Med. 2004;128:634-639)
Of the many facets of sickle cell disease, the osteoarticular manifestations occur most frequently, are the earliest to appear, and are the most difficult to diagnose.1,2 The sinusoidal blood flow and the high oxygen uptake within the bone marrow predisposes this tissue to stasis of blood, which promotes regional hypoxia, acidosis, sickling, and, consequently, thrombosis and infarction.1,4 In addition, the hyperplastic hematopoietic marrow in sickle cell disease persists within areas that normally convert to nonhematopoietic fatty marrow and, therefore, may be poorly adapted for hematopoiesis.5,6
After the first report of radiological findings in sickle cell disease by Cooley in 1927, diagnostic modalities relied initially on conventional radiography and later on isotope scans.7-9 Both of these modalities have significant limitations.1011 Conventional radiographs (plain films and computed tomography) record differences in densities of adjacent tissues and are not sensitive to the early stages of vaso-occlusion. Several days must lapse before ischemie injury causes sufficient anatomic changes to be detectable by conventional radiography. Likewise, scintigraphic studies, which primarily assess function by uptake of radiotracers, cannot differentiate various conditions in which activity is decreased, such as acute infarction, osteomyelitis, and some aggressive primary and metastatic tumors. Additionally, areas of decreased uptake may represent either an old infarct or residual normal fatty marrow. Finally, the clinical utility of both of these modalities carries the risk of radiation exposure, which is cumulative with repeated examinations.
Application of magnetic resonance imaging (MRI) to bone marrow diseases suggests that this noninvasive modality is useful in sickle cell disease, especially in differentiating acute from chronic ischemie changes.12-716 Patchy or mottled low- and high-signal areas in the marrow of patients with sickle cell disease increase with the age of the patient and with the number of crises.14 The distribution of the low-signal areas is reminiscent of the normal vascular distribution within the marrow. Correlation of the histopathology with MRI findings in 1 autopsy case suggested perivascular fibrosis was present.14 Elucidation of vascular changes in sickle cell disease may help improve the utility of this less invasive imaging modality.
This study was initiated to compare the histopathologic findings in nondiabetic, normotensive patients with sickle cell disease with those in nondiabetic, nonanemic, normotensive, age group-matched normal controls.
MATERIALS AND METHODS
This investigation was a retrospective, histochemical, morphometric study of blood vessels in hematopoietic bone marrow in cases of sickle cell hemoglobinopathy and in age group-matched normal control subjects. The archive at the Centralized Pathology Unit for Sickle Cell Disease in Mobile, Ala, was reviewed for cases with adequate clinical data and tissue samples. Clinical data were reviewed for age, sex, past medical and surgical history, and evidence of trauma or infections in the location of bone marrow sampling. Tissue samples were considered adequate when there were at least 5 low-power (times;10) fields of marrow for study. cases were excluded when there was clinical or morphologic evidence of hypertension, diabetes, vascular disease, connective tissue disorders, osteomyelitis, or trauma at the sampling site, and when the patient was older than 36 years. The upper age limit of 36 years for the study population was arbitrarily chosen to avoid the vascular changes expected with age. Hemoglobin (Hb) types were confirmed by electrophoresis or polymerase chain reaction.17 Patients with sickle hemoglobinopathy were subgrouped by Hb types (HbSS or HbSC) and by age (pediatrie group, 1-18 years; adult group, 19-36 years). Ten control subjects were selected as nondiabetic, normotensive, nonanemic cases with HbAA and no clinical or morphologic evidence of anemia, hypertension, diabetes, vascular disease, connective tissue disorders, osteomyelitis, or trauma at the sampling site. Control subjects were subgrouped by age (as study group).
Bone marrow samples were obtained either by biopsy or at autopsy from iliac crests, tibias, or vertebral bodies; fixed in buffered formalin; and processed routinely for histologie sections. Histochemical stains included hematoxylin-eosin and Masson trichrome. Appropriate histologie controls were used to evaluate the quality of the stains, and slides were excluded when the stain or tissue section was inadequate. Multiple levels of each sample were studied morphometrically in a masked fashion by 2 observers who were unaware of the origin of each tissue. In all cases, histologie sections were reviewed to select appropriate fields for morphometric analyses. sections were excluded when representation of the architecture was inadequate or when there was evidence of necrosis, infarct, inflammatory changes, or fracture. Morphometric parameters included the number of arterial blood vessels per high-power field and blood vessel diameter (measured at narrowest point). Arterial blood vessels were categorized by luminal diameter as small (100 µm).
Simple point counting was used to quantitate relative proportions of vessel wall composed of muscle and fibrous connective tissue, w all blood vessels were photographed using the same microscope, ocular objectives, film-processing method, and photographic paper, and all were projected in a standardized manner onto a point-counting grid. sections with tangential cuts through the vascular walls were excluded. Point counts from photographs taken at 3 magnifications (×100, ×160, and ×400) were mathematically adjusted to a common magnification base (×400). Data were analyzed using the following variables: mean point counts (MFCs) for muscle, MFCs for fibrous tissue, ratio of fibrous tissue point counts to muscle point counts, and point count difference (fibrous tissue point counts minus muscle point counts). Data for controls and sickle study groups were compared for age group (pediatrie or adult), sex, sampling site (tibia, iliac crest, or vertebra), and vessel size by diameter (100 µm), and Hb type (HbSS, HbSC, or HbAA), and were tested for statistical significance using analysis of variance technique for the unbalanced data and corresponding multiple comparison procedures using least significant difference and Bonferroni (Dunn) t tests ([alpha] = .05; difference between means with 95% confidence intervals [CIs]). A difference was declared significant at P
RESULTS
Age and sex characteristics for each Hb type are summarized in Table 1. The mean age for cases with homozygous sickle disease (HbSS) was slightly younger and for HbSC was older than the age group-matched normal controls (HbAA), but the differences were not significant (P = .65 and P = .37, respectively). The male-female ratios were predominantly female for both HbSS and HbAA and were equal for HbSC. Pediatrie and adult age group distributions were nearly equal for both sickle study groups and controls. Causes of death in the HbSS group were infection (62%), stroke (15%), splenic sequestration (15%), and transfusion reaction (8%); in the HbSC group, infection (50%), trauma (38%), and drug overdose (12%); and in the HbAA group, trauma (40%), infection (40%), ruptured cerebral aneurysm (10%), and diaphragmatic hernia (10%).
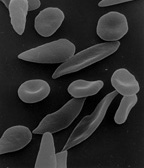
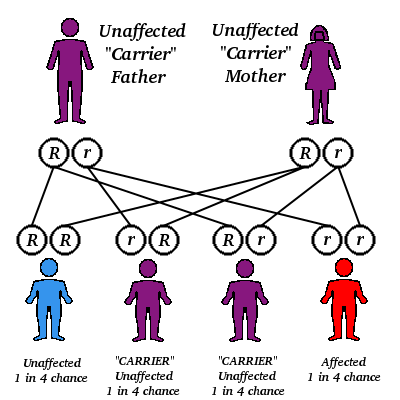
Microscopically, the HbAA samples had a normal architecture of marrow and bone with no significant pathologic changes. In the HbSS group, the marrow cavity was expanded by hyperplastic hematopoietic tissue, vascular channels were distended by sickle erythrocytes, and bony trabeculae were thin and irregular. These changes were most pronounced in the older patients. Frequently, on hematoxylin-eosin-stained sections, small blood vessels were ectatic and blood vessels of all sizes were surrounded by collars of eosinophilic, sparsely cellular tissue, which was composed of fibrous connective tissue by trichrome stains (Figure 1). The microscopic findings in HbSC cases were intermediate between those in HbSS and HbAA cases, with minimal to mild hyperplasia of hematopoietic marrow and no significant thinning of bony trabeculae.
The mean number of small (100 µm) per sample was too low for study in all of the pediatrie groups, but was the same (6.0 ± 0.0) for all of the adult groups (HbSS, HbSC, and HbAA).
Comparison of the overall MPCs for muscle in HbSS, HbSC, and HbAA cases, including all age groups and all vessel sizes (Figure 2), showed no significant differences between the HbSC and HbAA groups (P = .78; difference between means, 0.98; 95% CI, -8.5,10.4), HbSS and HbSC (P = .67; -0.20; 95% CI, -8.7, 8.3), or HbSS and HbAA (Table 2). Comparison of the overall MPCs for fibrous tissue in the HbSS, HbSC, and HbAA groups, including all age groups and all vessel sizes (Figure 2), showed HbSS cases had significantly greater amounts of fibrous tissue compared with either HbSC (P
Differences between the HbSS and HbAA groups were further studied by vessel sizes, age groups, and ratios of arterial fibrous tissue to muscle. Comparison of MPCs for muscle by vessel sizes, including all age groups in HbSS and HbAA cases (Table 2), showed muscle was significantly decreased in HbSS small vessels compared with HbAA, consistent with dilation. In medium-sized vessels, however, comparison of MPCs for muscle showed a nonsignificant increase in the HbSS group as compared with the HbAA group. Comparison of MPCs for fibrous tissue showed HbSS cases had significantly greater fibrous tissue in small and medium-sized vessels and a nonsignificant increase in large vessels compared with HbAA cases (Table 2).
Comparison of MPCs for muscle in all vessel sizes for the HbSS and HbAA groups showed a tendency to increase with age group, as expected with growth (Table 3). Further comparison by vessel sizes for each age group showed a nonsignificant decrease for muscle in HbSS adult small vessels, consistent with dilation, and a nonsignificant increase in HbSS medium-sized vessels (Table 3). However, MPCs for muscle were significantly increased in HbSS adult medium-sized vessels (consistent with medial hypertrophy), compared with HbAA (Table 3).
Comparison of MPCs for fibrous tissue in all vessel sizes for the HbSS and HbAA groups showed a tendency to increase with age group, as expected with growth (Table 4); the increases were significantly greater in both pediatrie and adult age groups in HbSS. Furthermore, comparison by vessel size showed the increased fibrous tissue was significantly greater for HbSS in all pediatrie vessels studied (small and medium sizes) and in medium-sized adult vessels compared with HbAA (Table 4).
To study the proportion of the arterial wall occupied by fibrous tissue and muscle, the ratio of MFCs for fibrous tissue to that for muscle was calculated for each group and compared (Table 5). The ratios showed the increase in fibrous tissue was significantly greater in both the pediatrie and adult HbSS cases than it was in the HbAA group. Further analysis of the data by vessel size showed the findings differed with age. In pediatrie HbSS cases, all of the blood vessels studied (small and medium-sized vessels) had proportionately more fibrous tissue, but in adult HbSS cases, only the large vessels had proportionately more fibrous tissue compared with HbAA cases. The same significant differences were evident when the data were analyzed by calculation of the differences between MFCs for fibrous tissue and those for muscle. Additionally, in the pediatrie HbAA group, the ratios were less than 0.45, indicating proportionately more muscle than fibrous tissue; in the pediatrie HbSS group, however, the ratios were greater than 2, indicating proportionately more fibrous tissue than muscle. In all adult groups, the ratios were greater than 0.8 for all vessel sizes and were significantly greater only for the large vessels in HbSS. Finally, when the data were studied by sex and sampling site, no statistically significant differences were noted.
COMMENT
Previous MRI studies of long bones in sickle cell disease have shown patchy low signals that increase with age and with number of sickle cell crises.13·14 These signals are frequently serpiginous or radially arranged on cross-sections of the marrow cavity (Figure 3). The distribution of these signals is reminiscent of the normal vascular supply to the bone marrow in these long bones (Figure 4). The marrow of long bones is supplied by a nutrient diaphyseal artery, epiphyseal arteries, perforating metaphyseal vessels, and periosteal vessels.20 The nutrient arteries run in the central longitudinal axis, giving off slender arteriolar branches in a radial fashion. Some of these arterioles travel through and out of the marrow, enter the surrounding cortical bone, and run in haversian canals; but many terminate as capillaries near the periphery of the marrow. The periosteal vessels usually supply only the outer portion of cortex in the adult and are not important sources of blood flow to the marrow under normal conditions. When the main nutrient vessel is compromised, however, the periosteal and metaphyseal vessels and their anastomoses with cortical vessels become very important as collateral channels.21 Normally, the circulation passes centrifugally from the medullary cavity to the periosteal surface, but following occlusion of the nutrient artery, the blood flow can reverse.21 These anastomotic vessels are radially arranged on cross-sectioning of long bone.
The few histopathologic studies of the bone marrow of long bones in sickle cell disease that have been published to date have described decreased fat and exuberant hyperplasia of erythroid precursors, as well as granulocytic and megakaryocytic elements, dilation of sinusoids by tightly packed aggregates of sickled cells, thinning and irregular configuration of bony trabeculae, varying stages of infarct resolution, and areas of fibrosis.1422 In sickle cell disease, stasis occurs primarily where blood flow is sinusoidal, where oxygen uptake is high, where circulation is terminal, or where collaterals are poorly developed.22,23 The normal blood flow through the bone marrow meets most of these conditions in sickle cell disease. Several reasons have been postulated to account for the vulnerability of the bone marrow to injury by the stasis and ischemia in sickle cell disease.3"* In the hyperplastic bone marrow of homozygous sickle cell disease, oxygen uptake is increased because of the increased hematopoietic activity. The sludging of blood flow during crisis increases the already high baseline demands for oxygen and exacerbates the local and regional acidosis, hypoxemia, and infarction. The intravascular sludging leads to increased resistance to blood flow and distention and/or constriction of vascular channels.
This morphometric study of bone marrow has shown significant vascular changes that vary with vessel size and with age in sickle cell disease. The evidence of decreased muscle thickness in small bone marrow arteries is consistent with distention of these vessels secondary to sludging of blood flow through the more distal sinusoidal channels. The increased thickness of muscle in the medium-sized arteries of adult sickle cell samples, but not in the pediatrie samples, suggests a proliferative response of the vascular smooth muscle that appears with increased age. Previous studies in cultures have shown that conditions of hypoxia or even simple exposure of endothelial cells to sickled erythrocytes cause a 4- to 8-fold transcriptional induction of the gene encoding endothelin-1 and release of this potent vasoconstrictor into the medium.24 Increased levels of endothelin-1 have actually been demonstrated in the plasma of patients with sickle cell anemia.25,26 It is interesting to speculate that the increased muscle reflects a mitogenic response of the vascular smooth muscle to such vasoactive amines released by endothelial cells in response to sickled cells and/or hypoxia. Additional studies are needed.
Finally, the increased perivascular fibrosis seen in this study was seen in all vessel sizes and in all age groups compared to normal controls. The proportion of fibrous tissue within the vessel walls was greatest for the pediatrie sickle cell group, suggesting an age-related catch-up phenomenon in the adult controls. Nevertheless, this perivascular fibrosis may provide a compartment where edema fluid can collect during crisis and be detectable by MRI as patchy low signals. In this scenario, perivascular fibrosis would likely increase with increased severity of the disease and with increased frequency of crises, similar to the MRI signals. The finding of intermediate amounts of perivascular fibrosis in HbSC disease is consistent with the milder degrees of anemia, milder sickling of red cells, and few or no crises or vaso-occlusion in this hemoglobinopathy.
Additional studies are needed for correlation of these histopathologic findings with MRI findings, which may be useful in the long-term follow-up and management of patients with homozygous sickle cell disease.
This study was supported by the Heart, Lung, and Blood Institute of the National Institutes of Health, Bethesda, Md, contract No. NO1-HB-07086.
References
1. Ben Dridi MF, Oumaya A. Gastli H, et al. Radiological abnormalities of the skeleton in patients with sickle-cell anemia: a study of 222 cases in Tunisia. Pediatr Radial. 1987;1 7:296-302.
2. Serjeant CR, Serjeant BE. Bone and joint lesions. In: Serjeant CR, Serjeant BE, eds. Sickle Cell Disease. 3rd ed. New York, NY: Oxford University Press; 2001:240-280.
3. Eukens JN. Sickle cell disease. Dis Mon. 1981:27:1-56.
4. Charache SE, Eubin BH, Reid CD. Management and Therapy of Sickle Cell Disease. Washington, DC: US Department of Health and Human Services, National Institutes of Health; 1989:1-51. Publication 85-211 7.
5. Cristy M. Active bone marrow distribution as a function of age in humans. Phys Med Biol. 1981:26:389-400.
6. Kricun ME. Red-yellow marrow conversion: its effects on the location of some solitary bone lesions. Skel Radiol. 1985;14:10-19.
7. Eecklitner ML. Nuclear imaging studies and sickle cell disease. Ala I Med Sd. 1987:24:390-396.
8. Heiden RA, Eocko RC, Stent TR. Hyperemic peripheral red marrow in a patient with sickle cell anemia demonstrated on Tc-99m labeled red blood cell venography. CUn Nucl Med. 1991:16:153-156.
9. Glaser AM, Chen DC, Siegel ME, Norris SE, Haywood EJ. An unusual scintigraphic pattern in sickle cell patients. Fury Nucl Med. 1989;!5:357-360.
10. Kirn HC, Alavi A, Russell MO, Schwartz E. Differentiation of bone and bone marrow infarcts from osteomyelitis in sickle cell disorders. Clin Nucl Med. 1989:14:249-254.
11. Skaggs DE, Kim SK, Greene NW, Harris D, Miller JH. Differentiation between bone infarction and acute osteomyelitis in children with sickle-cell disease with use of sequential radionuclide bone-marrow and bone scans. / Bone joint SurgAm. 2001;83-A:1810-1813.
12. Roa VM, Mitchell DG, Rifkin MD, et al. Marrow infarction in sickle cell anemia: correlation with marrow type and distribution by MRI. Magn Reson Imaging. 1989;7:39-44.
13. Mankad VN, Yang Y-M, Williams JP, Harpen M, Brogdon BC. Magnetic resonance imaging, of bone marrow in sickle cell patients. Am j Pediatr Hematol Oncol. 1988; 10:344-347.
14. Mankad VN, Williams JP, Harpen MD, et al. Magnetic resonance imaging of bone marrow in sickle cell disease: clinical, hematologie and pathologic correlations. Blood. 1990;75:274-283.
15. Powers JA. Magnetic resonance imaging in marrow diseases. Clin Orthop. 1986;206:79-85.
16. van Zanten TE. Statius van Eps EW, Golding RP, VaIk J, Stratius van Eps EW. Imaging the bone marrow with magnetic resonance during a crisis and in chronic forms of sickle cell disease. CHn Radiol. 1989;40:486-489.
17. Manci EA, Culberson DE, Chen GJ, Mankad V, Joshi VV, Fujumura FK. Polymerase chain reaction facilitates archival autopsy studies of sickle cell disease. Pediatr Pathol. 1993;13:75-81.
18. Weibel ER. Practical methods for biological morphometry. In: Weibel ER, ed. Stereologicat Methods. VoI 1. Eondon, United Kingdom: Academic Press; 1979:1-396.
19. Weibel ER. Morphometry: stereological theory and practical methods. In: Gil J, ed. Models of Lung Disease: Microscopy and Structural Methods. New York, NY: Marcel Dekker; 1990:245-353.
20. Kelly PJ. Anatomy, physiology and pathology of the blood supply of bones. Bone Joint Surg Am. 1968;50:766-783.
21. Earson RE, Kelly PJ, Janes JM, Peterson EFA. Suppression of the periosteal and nutrient blood supply of the femora of dogs. CHn Orthop. 1961 ;21:217-223.
22. Diggs EW, Pulliam HN, King JC. The bone changes in sickle cell anemia. South Med J. 1937;30:249-258.
23. Middlemiss JH, Raper AB. Skeletal changes in the haemoglobinopathies./ Bone Joint Surg Br. 1966:48:693-702.
24. Phelan M, Perrine SP, Brauer M, Faller DV. Sickle erythrocytes, after sickling, regulate the expression of the endothelin-1 gene and protein in human endothelial cells in culture, y Clin Invest. 1995;96:1145-1151.
25. Rybicki AC, Musto S, Swinson GE, Benjamin EJ, Nagel RE, Schwartz RS. Increased levels of endothelin-1 in plasma of sickle cell anemia patients. Blood. 1991;78:202a.
26. Eongenecker GD, Culberson D, Beyers B, Manci E, Mankad V. Plasma endothelin (ET) levels are elevated in sickle cell disease (SCD). Blood. 1991;78: 1645a.
Elizabeth A. Manci, MD; Donald E. Culberson, PhD; julia M. Gardner, BA; Byron C. Brogdon, MD; Arvind K. Shah, PhD; J. Elyse Holladay; Randall W. Powell, MD; Vipul N. Mankad, MD
Accepted for publication January 28, 2004.
From the Departments of Pathology (Drs Manci and Culberson, Ms Gardner, and Ms Holladay), Radiology (Dr Brogdon), Mathematics and Statistics (Dr Shah), and Pediatrie Surgery (Dr Powell), University of South Alabama, Mobile; and the Department of Pediatrics, University of Kentucky, Lexington (Dr Mankad).
The authors have no relevant financial interest in the products or companies described in this article.
Reprints: Elizabeth A. Manci, MD, University of South Alabama, Centralized Pathology Unit for Sickle Cell Disease, 1700 Center St, Mobile, AL 36604 (e-mail: emanci@usouthal.edu).
Copyright College of American Pathologists Jun 2004
Provided by ProQuest Information and Learning Company. All rights Reserved