Context.-The transfusion of donor red blood cell units (RBCs) that lack certain red cell antigens (such as C, E, and K) when the corresponding antigens are absent from the recipient's red cells has been shown to reduce the risk of red cell alloimmunization in sickle cell disease patients. However, data are limited regarding the extent to which transfusion services routinely perform red cell antigen phenotype testing of nonalloimmunized sickle cell disease patients, and then use that information to select donor RBCs lacking 1 or more of the red cell antigens that the patient's red cells do not express.
Objective.-To determine the extent to which transfusion services routinely perform red cell antigen phenotype testing of nonalloimmunized sickle cell disease patients, and then use that information to select donor RBCs lacking 1 or more of the red cell antigens that the patient's red cells do not express.
Design.-An educational subsection of a College of American Pathologists Proficiency Testing Survey (J-C 2003) assessed transfusion service practices regarding performance of red cell antigen phenotype testing of nonalloimmunized sickle cell disease patients and how transfusion services use this information for the selection of donor RBCs. The data analysis of the survey included 1182 North American laboratories.
Results.-Data from 1182 laboratories were included in the survey analysis, of which the majority (n = 743) reported that they did not routinely perform phenotype testing of sickle cell disease patients for antigens other than ABO and D. The other 439 laboratories reported that they did routinely perform phenotype testing of sickle cell disease patients for antigens in addition to ABO and D. The majority of these 439 laboratories (three fourths; n = 330) reported that they used these patient data for prophylactic matching with donor RBCs when sickle cell disease patients required transfusion. When phenotype-matched donor RBCs were used, the antigens most commonly matched (85% of the time) were C, E, and K.
Conclusions.-The majority of North American hospital transfusion service laboratories do not determine the red cell antigen phenotype of nonalloimmunized sickle cell disease patients beyond ABO and D. Those laboratories that do determine the red cell phenotype of nonalloimmunized sickle cell disease patients beyond ABO and D most commonly match for C, E, and K antigens when phenotype-matched donor RBCs are used.
(Arch Pathol Lab Med. 2005;129:190-193)
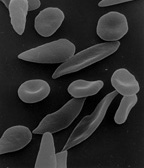
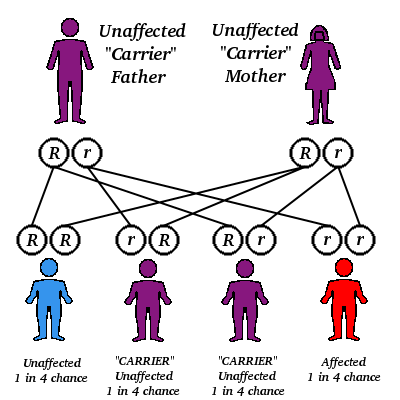
Sickle cell disease affects approximately 72 000 people in the United States (approximately 1 in 500 African Americans and 1 in 1000 to 1400 Hispanics).1 During the past 30 years, the management of sickle cell disease has improved significantly, such that today, patients with sickle cell disease are living beyond 50 years of age, rather than dying before the age of 14.2 Transfusion therapy has played a role in allowing sickle cell disease patients to live longer.1 However, associated with red blood cell unit (RBC) transfusion is the risk of red cell antigen alloimmunization, and studies show that 25% or more of chronically transfused sickle cell disease patients may experience alloimmunization to red cell antigens.4 Several reports document that the most common clinically significant alloantibodies to develop in transfused sickle cell disease patients include antibodies to the Rhesus blood group system antigens, such as C and E, and to the Kell blood group system antigens, such as K.5-8
Studies have also shown that the transfusion of ABO- and D-compatible donor RBCs that lack C, E, or K antigens when the corresponding antigen(s) are absent on the recipient's red cells can significantly reduce the rate of alloimmunization in patients with sickle cell disease and can also decrease the occurrence of complications such as hemolytic transfusion reactions.4
This report describes the results of a data subset from a recent College of American Pathologists (CAP) Proficiency Testing Survey (J-C 2003). The data subset came from an educational module that was designed to determine the extent to which hospitals perform phenotype testing of nonalloimmunized sickle cell disease patients and then select donor RBCs that lack 1 or more red cell antigens that the patient's red cells do not express.
MATERIALS AND METHODS
The CAP Proficiency Testing Survey J-C 2003 was distributed to 4251 participants to assess their proficiency in testing the following analytes: ABO, Rhesus (Rh), antibody detection, antibody identification, and crossmatching.
A subset of the survey participants (n = 1360) also subscribed to an educational module through which they were surveyed for their routine practice to provide (or not to provide) phenotype-matched donor RBCs for the transfusion of nonalloimmunized sickle cell disease patients. The survey consisted of a case history, a series of short vignettes that pertained to the case history, and follow-up questions that allowed for the survey of laboratory practices (see "Results"). By the data collection deadline (set as 10 working days after receipt of survey materials), participants had submitted their survey responses. The survey focused on whether or not laboratories routinely performed red cell phenotype testing of nonalloimmunized sickle cell disease patients, and if so, whether they used that information for prophylactic matching of donor RBCs for antigens other than ABO and D. No effort was made to stratify the data according to the category of the transfusion (eg, red cell exchange, response to a life-threatening event). In addition, no questions were directed at the participants to determine how they discover that a particular patient has sickle cell disease.
RESULTS
The survey participants were to answer a number of questions based on the following history: "Your blood bank is made aware of a newly diagnosed sickle cell disease patient who will require a chronic transfusion therapy regimen. Your tests show that the patient is group A, Rh positive, and has a negative antibody screen. The physician orders a unit of red blood cells to be crossmatched for a transfusion later that day." The responses to the survey questions are displayed in Tables 1 through 9.
COMMENT
A total of 1182 North American laboratories (most located in the United States) participated in the educational module of the CAP J-C 2003 survey. The majority of laboratories participating (n = 743; 62.9% of all participants) followed a policy that did not require them to perform red cell antigen phenotype testing beyond ABO and D for nonalloimmunized sickle cell disease patients. Slightly more than 37% (n = 439) of participants routinely determined a red cell antigen phenotype beyond ABO and D for nonalloimmunized sickle cell disease patients. Of these 439 laboratories, 75% (n = 330) reported using the patient's phenotype to select ABO/D-compatible donor RBC units lacking 1 or more of the following red cell antigens (in descending order of frequency): K, E, and C (about one third of all laboratories); c, e (about one fifth of all laboratories); and Jk^sup a^, Jk^sup b^, Fy^sup a^, and Fy^sup b^ (about one seventh of all laboratories).
Clinical evidence that the transfusion of phenotype-matched donor RBCs benefits sickle cell disease patients is provided by several studies.4,9,10 A study done by Castro et al10 evaluated several protocols to determine the most reasonable approach to prevent alloimmunization in sickle cell disease patients; they concluded that the most common antibodies formed by these patients were to the C, E, and K antigens. When using the protocol that matched donor RBCs according to the patient's phenotype for C, c, E, e, and K, 87.5% of sickle cell patients in the study would not have developed alloantibodies, as compared with 70.9% under the protocol of matching for ABO and D alone. Another study, by Vichinsky et al,4 showed that phenotype matching for C, E, and K resulted in a drastic decrease in delayed hemolytic transfusion reactions (which dropped 90%), whereas the alloimmunization rate dropped from 3% to 0.5%.
Despite the evidence that phenotype matching of donor RBCs for C, E, and K antigens (in addition to ABO and D) reduces the risk of alloimmunization of sickle cell disease patients,4,9,10 the data presented in the CAP survey under discussion indicate that the majority of North American hospital transfusion service laboratories do not appear to perform phenotypic testing for antigens other than ABO and D for these patients. The justification for choosing not to provide donor RBC units that are matched for at least C, E, and K antigens for sickle cell patients might be that at most only about 25% of sickle cell disease patients will develop alloantibodies if phenotype-matched donor RBCs are not provided. In other words, if phenotype matching of the nonalloimmunized patient is not done and if donor RBCs are not selected to match the phenotype of the patient, then the majority of sickle cell disease patients (up to or approximately 75%) do not develop alloimmunization. However, arguments in favor of the routine use of at least C-, E-, and K-matched donor RBC units are seen in the data published by Castro et al10 and by Vichinsky et al,4 which show the greatest reduction in alloimmunization risk when donor RBC units are selected to avoid expressing C, E, or K when the recipient is capable of making anti-C, anti-E, or anti-K. A reduction in alloimmunization risk can translate into a reduction in morbidity and mortality of sickle cell disease patients that might otherwise occur if alloantibodies developed, including the cost to treat complications of alloimmunization, such as acute and delayed hemolytic transfusion reactions. In addition, one might also consider the cost and risks associated with a delay in locating compatible blood for necessary transfusions in the event that alloimmunization occurs.
The CAP survey data presented in this report showed that about 37% of laboratories perform red cell phenotype testing for antigens other than ABO and D to obtain baseline phenotype data that can be used for donor RBC unit selection. Most, but not all, of the laboratories that do this phenotype testing use this patient phenotypic information to provide prophylactic matching of donor RBCs with the red cell phenotype of the patient. This suggests that the actual practice of the larger "community" favors not performing antigen phenotyping of sickle cell disease patients beyond ABO/D until the patients become alloimmunized. These data are different than those published in a smaller survey by Afenyi-Annan and Brecher,11 which surveyed 50 academic medical centers. In the Afenyi-Annan and Brecher survey, the authors found that 66% of academic hospital transfusion services routinely provided ABO/D-compatible donor RBCs that were matched for 1 or more additional red cell antigens, in order to reduce the risk of red cell alloimmunization. This suggests that the actual practice of academic centers favors performing antigen phenotyping of sickle cell disease patients beyond ABO/D before the patients become alloimmunized. Importantly, both surveys clearly show that there is not a consensus among community hospitals and academic centers regarding provision of phenotype-matched RBCs to prevent (or reduce) the risk of red cell alloimmunization in sickle cell disease patients who require transfusion. The difference between the current data set and the data from Afenyi-Annan and Brecher11 might be due to the method employed to collect the CAP data subset shown in this report. The responding hospitals in the CAP survey data subset were participating in an educational module, so that there might have been self-selection in favor of laboratories unfamiliar with phenotyping sickle cell disease patients and then matching donor RBC phenotypes to reduce their risk of red cell alloimmunization. However, both the AfenyiAnnan and Brecher11 and CAP survey data suggest there is no consensus to provide phenotype-matched donor RBCs for sickle cell disease patients. Between one third and two thirds of laboratories routinely do not provide ABO/D-compatible donor RBCs that are matched for 1 or more additional red cell antigens, in order to reduce the risk of red cell alloimmunization in patients with sickle cell disease. One might argue that a more standardized approach should be encouraged for the pretransfusion selection of donor RBCs for nonalloimmunized sickle cell disease patients. A more standardized approach would increase the likelihood that sickle cell disease patients would receive a similar standard of care with respect to transfusion therapy.
This study's data demonstrate a lack of consensus for the use of red cell phenotype information in the selection of donor RBCs for nonalloimmunized sickle cell disease patients. It is likely that this lack of consensus is due to a combination of cost and cost-benefit considerations for the management of sickle cell disease in general and transfusion therapy in particular. For example, one study showed that the financial impact of chronic transfusion therapy for sickle cell disease patients is substantial, with charges approaching $400 000 per patient-decade for patients who require deferoxamine chelation.12 A lack of universal use of phenotype-matched donor RBCs for the transfusion of sickle cell disease patients is likely to continue as long as cost-containment pressures exist and there is a lack of clear evidence that the use of phenotype-matched donor RBCs will improve overall cost-effectiveness of therapy. We believe that there is a need for well-designed studies that can provide objective evidence.
References
1. National Institutes of Health, National Heart, Lung, and Blood Institute. Facts About Sickle Cell Anemia. Washington, DC: National Institutes of Health; 1996. NIH publication 96-4057.
2. Claster S, Vichinsky EP. Clinical review: managing sickle cell disease. BMI. 2003;327:1151-1155.
3. National Institutes of Health, National Heart, Lung, and Blood Institute. Management of Sickle Cell Disease. 4th ed. Washington, DC: National Institutes of Health; 2002. NIH publication 02-2117.
4. Vichinsky EP, Luban N, Wright E, Olivieri N. Prospective RBC phenotype matching in a stroke-prevention trial in sickle cell anemia: a multicenter transfusion trial. Transfusion. 2001;41:1086-1092.
5. Vichinsky EP, Earles A, Johnson RA, Hoag MS. Alloimmunization in sickle cell anemia and transfusion of racially unmatched blood. N Engl J Med. 1990;322:1617-1621.
6. Rosse WF, Callagher D, Kinney TR, Castro O, for The Cooperative Study of Sickle Cell Disease. Transfusion and alloimmunization in sickle cell disease. Blood. 1990;76:1431-1437.
7. Davies SC, McWilliam AC, Hewitt PE, Devenish A, Brozovic M. Red cell alloimmunization in sickle cell disease. Br J Haematol. 1986;63:241-245.
8. Orlina AR, Unger PJ, Koshy M. Post-transfusion alloimmunization in patients with sickle cell disease. Am J Hematol. 1978;5:101-106.
9. Ness PM. To match or not to match: the question for chronically transfused patients with sickle cell anemia. Transfusion. 1994;34:558-560.
10. Castro O, Sandier SC, Houston-Yu P, Rana S. Predicting the effect of transfusing only phenotype-matched RBCs to patients with sickle cell disease: theoretical and practical implications. Transtusion. 2002;42:684-690.
11. Afenyi-Annan A, Brecher ME. Pre-transfusion phenotype matching for sickle cell disease patients. Transfusion. 2004;44:619-620.
12. Wayne AS, Schoenike SE, Pegelow CH. Financial analysis of chronic transfusion for stroke prevention in sickle cell disease. Blood. 2000;96:2369-2372.
Melanie Osby, MD; Ira A. Shulman, MD
Accepted for publication September 24, 2004.
From the Department of Pathology, Los Angeles County-University of Southern California Medical Center, Los Angeles, Calif. Dr Osby is currently a Fellow in Transfusion Medicine at Cedars-Sinai Medical Center, Los Angeles, Calif.
The authors have no relevant financial interest in the products or companies described in this article.
Corresponding author: Ira A. Shulman, MD, Department of Pathology, Los Angeles County-University of Southern California Medical Center, 1200 N State St, Room 22900, Los Angeles, CA 90033 (e-mail: ishulman@usc.edu).
Reprints not available from the authors.
Copyright College of American Pathologists Feb 2005
Provided by ProQuest Information and Learning Company. All rights Reserved