Definition
Movement disorders are a group of diseases and syndromes affecting the ability to produce and control movement.
Description
Though it seems simple and effortless, normal movement in fact requires an astonishingly complex system of control. Disruption of any portion of this system can cause a person to produce movements that are too weak, too forceful, too uncoordinated, or too poorly controlled for the task at hand. Unwanted movements may occur at rest. Intentional movement may become impossible. Such conditions are called movement disorders.
Abnormal movements themselves are symptoms of underlying disorders. In some cases, the abnormal movements are the only symptoms. Disorders causing abnormal movements include:
- Parkinson's disease
- Parkinsonism caused by drugs or poisons
- Parkinson-plus syndromes (progressive supranuclear palsy, multiple system atrophy, and cortical-basal ganglionic degeneration)
- Huntington's disease
- Wilson's disease
- Inherited ataxias (Friedreich's ataxia, Machado-Joseph disease, and spinocerebellar ataxias)
- Tourette syndrome and other tic disorders
- Essential tremor
- Restless leg syndrome
- Dystonia
- Stroke
- Cerebral palsy
- Encephalopathies
- Intoxication
- Poisoning by carbon monoxide, cyanide, methanol, or manganese.
Causes & symptoms
Causes
Movement is produced and coordinated by several interacting brain centers, including the motor cortex, the cerebellum, and a group of structures in the inner portions of the brain called the basal ganglia. Sensory information provides critical input on the current position and velocity of body parts, and spinal nerve cells (neurons) help prevent opposing muscle groups from contracting at the same time.
To understand how movement disorders occur, it is helpful to consider a normal voluntary movement, such as reaching to touch a nearby object with the right index finger. To accomplish the desired movement, the arm must be lifted and extended. The hand must be held out to align with the forearm, and the forefinger must be extended while the other fingers remain flexed.
The motor cortex
Voluntary motor commands begin in the motor cortex located on the outer, wrinkled surface of the brain. Movement of the right arm is begun by the left motor cortex, which generates a large volley of signals to the involved muscles. These electrical signals pass along upper motor neurons through the midbrain to the spinal cord. Within the spinal cord, they connect to lower motor neurons, which convey the signals out of the spinal cord to the surface of the muscles involved. Electrical stimulation of the muscles causes contraction, and the force of contraction pulling on the skeleton causes movement of the arm, hand, and fingers.
Damage to or death of any of the neurons along this path causes weakness or paralysis of the affected muscles.
Antagonistic muscle pairs
This picture of movement is too simple, however. One important refinement to it comes from considering the role of opposing, or antagonistic, muscle pairs. Contraction of the biceps muscle, located on the top of the upper arm, pulls on the forearm to flex the elbow and bend the arm. Contraction of the triceps, located on the opposite side, extends the elbow and straightens the arm. Within the spine, these muscles are normally wired so that willed (voluntary) contraction of one is automatically accompanied by blocking of the other. In other words, the command to contract the biceps provokes another command within the spine to prevent contraction of the triceps. In this way, these antagonist muscles are kept from resisting one another. Spinal cord or brain injury can damage this control system and cause involuntary simultaneous contraction and spasticity, an increase in resistance to movement during motion.
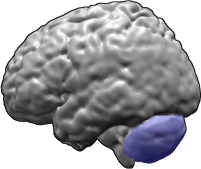
The cerebellum
Once the movement of the arm is initiated, sensory information is needed to guide the finger to its precise destination. In addition to sight, the most important source of information comes from the "position sense" provided by the many sensory neurons located within the limbs (proprioception). Proprioception is what allows you to touch your nose with your finger even with your eyes closed. The balance organs in the ears provide important information about posture. Both postural and proprioceptive information are processed by a structure at the rear of the brain called the cerebellum. The cerebellum sends out electrical signals to modify movements as they progress, "sculpting" the barrage of voluntary commands into a tightly controlled, constantly evolving pattern. Cerebellar disorders cause inability to control the force, fine positioning, and speed of movements (ataxia). Disorders of the cerebellum may also impair the ability to judge distance so that a person under- or over-reaches the target (dysmetria). Tremor during voluntary movements can also result from cerebellar damage.
The basal ganglia
Both the cerebellum and the motor cortex send information to a set of structures deep within the brain that help control involuntary components of movement (basal ganglia). The basal ganglia send output messages to the motor cortex, helping to initiate movements, regulate repetitive or patterned movements, and control muscle tone.
Circuits within the basal ganglia are complex. Within this structure, some groups of cells begin the action of other basal ganglia components and some groups of cells block the action. These complicated feedback circuits are not entirely understood. Disruptions of these circuits are known to cause several distinct movement disorders. A portion of the basal ganglia called the substantia nigra sends electrical signals that block output from another structure called the subthalamic nucleus. The subthalamic nucleus sends signals to the globus pallidus, which in turn blocks the thalamic nuclei. Finally, the thalamic nuclei send signals to the motor cortex. The substantia nigra, then, begins movement and the globus pallidus blocks it.
This complicated circuit can be disrupted at several points. For instance, loss of substantia nigra cells, as in Parkinson's disease, increases blocking of the thalamic nuclei, preventing them from sending signals to the motor cortex. The result is a loss of movement (motor activity), a characteristic of Parkinson's.
In contrast, cell loss in early Huntington's disease decreases blocking of signals from the thalamic nuclei, causing more cortex stimulation and stronger but uncontrolled movements.
Disruptions in other portions of the basal ganglia are thought to cause tics, tremors, dystonia, and a variety of other movement disorders, although the exact mechanisms are not well understood.
Some movement disorders, including Huntington's disease and inherited ataxias, are caused by inherited genetic defects. Some disease that cause sustained muscle contraction limited to a particular muscle group (focal dystonia) are inherited, but others are caused by trauma. The cause of most cases of Parkinson's disease is unknown, although genes have been found for some familial forms.
Symptoms
Abnormal movements are broadly classified as either hyperkinetic--too much movement--and hypokinetic--too little movement. Hyperkinetic movements include:
- Dystonia. Sustained muscle contractions, often causing twisting or repetitive movements and abnormal postures. Dystonia may be limited to one area (focal) or may affect the whole body (general). Focal dystonias may affect the neck (cervical dystonia or torticollis), the face (one-sided or hemifacial spasm, contraction of the eyelid or blepharospasm, contraction of the mouth and jaw or oromandibular dystonia, simultaneous spasm of the chin and eyelid or Meige syndrome), the vocal cords (laryngeal dystonia), or the arms and legs (writer's cramp, occupational cramps). Dystonia may be painful as well as incapacitating.
- Tremor. Uncontrollable (involuntary) shaking of a body part. Tremor may occur only when muscles are relaxed or it may occur only during an action or holding an active posture.
- Tics. Involuntary, rapid, nonrhythmic movement or sound. Tics can be controlled briefly.
- Myoclonus. A sudden, shock-like muscle contraction. Myoclonic jerks may occur singly or repetitively. Unlike tics, myoclonus cannot be controlled even briefly.
- Chorea. Rapid, nonrhythmic, usually jerky movements, most often in the arms and legs.
- Ballism. Like chorea, but the movements are much larger, more explosive and involve more of the arm or leg. This condition, also called ballismus, can occur on both sides of the body or on one side only (hemiballismus).
- Akathisia. Restlessness and a desire to move to relieve uncomfortable sensations. Sensations may include a feeling of crawling, itching, stretching, or creeping, usually in the legs.
- Athetosis. Slow, writhing, continuous, uncontrollable movement of the arms and legs.
Hypokinetic movements include:
- Bradykinesia. Slowness of movement.
- Freezing. Inability to begin a movement or involuntary stopping of a movement before it is completed.
- Rigidity. An increase in muscle tension when an arm or leg is moved by an outside force.
- Postural instability. Loss of ability to maintain upright posture caused by slow or absent righting reflexes.
Diagnosis
Diagnosis of movement disorders requires a careful medical history and a thorough physical and neurological examination. Brain imaging studies are usually performed. Imaging techniques include computed tomography scan (CT scan), positron emission tomography (PET), or magnetic resonance imaging (MRI) scans. Routine blood and urine analyses are performed. A lumbar puncture (spinal tap) may be necessary. Video recording of the abnormal movement is often used to analyze movement patterns and to track progress of the disorder and its treatment. Genetic testing is available for some forms of movement disorders.
Treatment
Treatment of a movement disorder begins with determining its cause. Physical and occupational therapy may help make up for lost control and strength. Drug therapy can help compensate for some imbalances of the basal ganglionic circuit. For instance, levodopa (L-dopa) or related compounds can substitute for lost dopamine-producing cells in Parkinson's disease. Conversely, blocking normal dopamine action is a possible treatment in some hyperkinetic disorders, including tics. Oral medications can also help reduce overall muscle tone. Local injections of botulinum toxin can selectively weaken overactive muscles in dystonia and spasticity. Destruction of peripheral nerves through injection of phenol can reduce spasticity. All of these treatments may have some side effects.
Surgical destruction or inactivation of basal ganglionic circuits has proven effective for Parkinson's disease and is being tested for other movement disorders. Transplantation of fetal cells into the basal ganglia has produced mixed results in Parkinson's disease.
Alternative treatment
There are several alternative therapies that can be useful when treating movement disorders. The progress made will depend on the individual and his/her condition. Among the therapies that may be helpful are acupuncture, homeopathy, touch therapies, postural alignment therapies, and biofeedback.
Prognosis
The prognosis for a patient with a movement disorder depends on the specific disorder.
Prevention
Prevention depends on the specific disorder.
Key Terms
- Botulinum toxin
- Any of a group of potent bacterial toxins or poisons produced by different strains of the bacterium . The toxins cause muscle paralysis, and thus force the relaxation of a muscle in spasm.
- Cerebral palsy
- A movement disorder caused by a permanent brain defect or injury present at birth or shortly after. It is frequently associated with premature birth. Cerebral palsy is not progressive.
- Computed tomography (CT)
- An imaging technique in which cross-sectional x rays of the body are compiled to create a three-dimensional image of the body's internal structures.
- Encephalopathy
- An abnormality in the structure or function of tissues of the brain.
- Essential tremor
- An uncontrollable (involuntary) shaking of the hands, head, and face. Also called familial tremor because it is sometimes inherited, it can begin in the teens or in middle age. The exact cause is not known.
- Fetal tissue transplantation
- A method of treating Parkinson's and other neurological diseases by grafting brain cells from human fetuses onto the basal ganglia. Human adults cannot grow new brain cells but developing fetuses can. Grafting fetal tissue stimulates the growth of new brain cells in affected adult brains.
- Hereditary ataxia
- One of a group of hereditary degenerative diseases of the spinal cord or cerebellum. These diseases cause tremor, spasm, and wasting of muscle.
- Huntington's disease
- A rare hereditary condition that causes progressive chorea (jerky muscle movements) and mental deterioration that ends in dementia. Huntington's symptoms usually appear in patients in their 40s. There is no effective treatment.
- Levodopa (L-dopa)
- A substance used in the treatment of Parkinson's disease. Levodopa can cross the blood-brain barrier that protects the brain. Once in the brain, it is converted to dopamine and thus can replace the dopamine lost in Parkinson's disease.
- Magnetic resonance imaging (MRI)
- An imaging technique that uses a large circular magnet and radio waves to generate signals from atoms in the body. These signals are used to construct images of internal structures.
- Parkinson's disease
- A slowly progressive disease that destroys nerve cells in the basal ganglia and thus causes loss of dopamine, a chemical that aids in transmission of nerve signals (neurotransmitter). Parkinson's is characterized by shaking in resting muscles, a stooping posture, slurred speech, muscular stiffness, and weakness.
- Positron emission tomography (PET)
- A diagnostic technique in which computer-assisted x rays are used to track a radioactive substance inside a patient's body. PET can be used to study the biochemical activity of the brain.
- Progressive supranuclear palsy
- A rare disease that gradually destroys nerve cells in the parts of the brain that control eye movements, breathing, and muscle coordination. The loss of nerve cells causes palsy, or paralysis, that slowly gets worse as the disease progresses. The palsy affects ability to move the eyes, relax the muscles, and control balance.
- Restless legs syndrome
- A condition that causes an annoying feeling of tiredness, uneasiness, and itching deep within the muscle of the leg. It is accompanied by twitching and sometimes pain. The only relief is in walking or moving the legs.
- Tourette syndrome
- An abnormal condition that causes uncontrollable facial grimaces and tics and arm and shoulder movements. Tourette syndrome is perhaps best known for uncontrollable vocal tics that include grunts, shouts, and use of obscene language (coprolalia).
- Wilson's disease
- An inborn defect of copper metabolism in which free copper may be deposited in a variety of areas of the body. Deposits in the brain can cause tremor and other symptoms of Parkinson's disease.
Further Reading
For Your Information
Books
- Martini, Frederic. Fundamentals of Anatomy and Physiology. Englewood Cliffs, NJ: Prentice Hall, 1989.
- Watts, Ray L. and William C. Koller, eds. Movement Disorders: Neurologic Principles and Practice. New York: McGraw-Hill, 1997.
Periodicals
- Movement Disorders. Lippincott-Raven Publishers, 12107 Insurance Way, Hagerstown, MD 21740.
Organizations
- WE MOVE. 1 Gustave L. Levy Place, Box 1052, New York, NY 10029. (800) 437-MOV2. http://www.wemove.org.
Gale Encyclopedia of Medicine. Gale Research, 1999.