The casual coexistence of ventricular preexcitation with either right or left bundle branch block has been reported by several authors.[1-4] The resulting electrocardiographic pattern is quite different, if the accessory pathway is located in the same side of the heart where the bundle branch block exists, or in the opposite side of the heart. In the former case, the bundle branch block is considered ipsilateral to the anomalous pathway, and in the latter, it is considered to be contralateral. Ipsilateral bundle branch block is masked when preexcitation is present and can be seen occasionally in the electrocardiogram only if the preexcitation is intermittent. The association of preexcitation and contralateral bundle branch block results in wide QRS complexes showing both delta waves and terminal slowing. An unusual combination of bifascicular block and Wolff-Parkinson-White syndrome forms the basis of this report.
CASE REPORT
The patient, a 52 year-old-woman with ischemic heart disease, had attacks of tachycardia since 1980. In the same year, the Wolff-Parkinson-White syndrome was diagnosed from surface electrocardiogram and confirmed by electrophysiologic study, which revealed a left-sided accessory pathway. In 1982, right bundle branch block was seen for the first time. On admission, the patient had orthodromic tachycardia 180 beats/min and right bundle branch block. She had nausea and was hypotensive. The attack was terminated by administration of amiodarone 300 mg intravenously. On x-ray examination, the heart silhouette was diffusely enlarged.
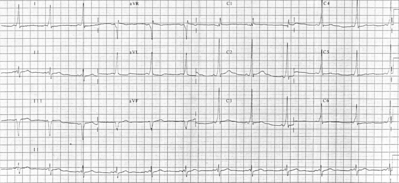
During the following days electrocardiograms showed two different patterns, which can be seen in Figures 1 and 2. One pattern (Fig 1) is consistent with right bundle branch block and left anterior hemiblock, and the other (Fig 2) with right bundle branch block and Wolff-Parkinson-White syndrome.
DISCUSSION
It is evident from both electrocardiographic tracings (Fig 1 and 2) that the patient had right bundle branch block. The electrocardiogram in Figure 1 shows additional features of the left anterior hemiblock. The latter can be diagnosed utilizing the following two criteria: (1) left axis deviation, and (2) delay of the intrinsicoid deflection in lead aVL. The delay in the intrinsicoid deflection in aVL that is not detected in [V.sub.6] is called "regional delay" and is, if found associated with left axis deviation, specific for left anterior hemiblock.[5] In our case, both criteria are fulfilled. The association of right bundle branch block and one of the left hemiblocks is often called bifascicular block.
The electrocardiogram in Figure 2 shows right bundle branch block only; the signs of left anterior fascicular block are missing. Since the conduction abnormalities can be intermittent, the first impression could be that the left anterior hemiblock is present only occasionally. A closer look at this electrocardiogram, however, reveals signs of ventricular preexcitation (Wolff-Parkinson-White syndrome). Note the short PR interval and the delta wave. The QRS complexes are wide both due to preexcitation and due to right bundle branch block, which persists during preexcitation. The electrophysiologic criteria for co-existence of preexcitation and contralateral bundle branch block were published elsewhere.[4]
The association of bundle branch block and preexcitation is rare, since these two conduction abnormalities have different pathoanatomic substrates.[1,2]
In Wolff-Parkinson-White syndrome an accessory pathway bypasses the normal conduction pathway through the atrioventricular node, His bundle and its branches, and preexcites a portion of the ventricle. It has been shown that the prexcitation obscures the electrocardiographic pattern of the branch block, if it is ipsilateral to the accessory pathway.[2,3] Thus, in our case, the persistence of the right bundle branch block during preexcitation is indirect evidence of the fact that the accessory pathway is contralateral to the branch block, ie, left-sided. We reach the same conclusion by analyzing the delta wave polarity.[6] We see, however, that the conduction through the accessory pathway--intermittent in our patient--obscures the signs of left anterior hemiblock. The left ventricle is at least partly activated by the depolarization wave coming through the accessory pathway and the conduction delay due to left anterior fascicular block has no effect on the electrocardiographic pattern.
REFERENCES
[1] Pick A, Fisch C. Ventricular preexcitation (WPW) in the presence of bundle branch block. Am Heart J 1958; 55:504-12
[2] Denes P, Goldfinger P, Rosen KM. Left bundle branch block and intermittent type A preexcitation. Chest 1975; 68:356-58
[3] Rakovec P, Kranjec I, Fettich JJ. Association of an accessory pathway and ipsilateral bundle branch block. Int J Cardiol 1985; 7:161-64
[4] Rakovec P, Kranjec I, Fettich JJ, Jakopin J, Fidler V, Turk J. Wolff-Parkinson-White syndrome type B and left bundle-branch block: Electrophysiologic and radionuclide study. Clin Cardiol 1985; 8:51-6
[5] Horwitz S, Lupi E, Hayes J, Frishman W, Cardenas M, Killip T. Electrocardiographic criteria for the diagnosis of left anterior fascicular block. Chest 1975; 68:317-20
[6] Gallagher JJ, Pritchett ELC, Sealy WC, Kasell J, Wallace AG. The preexcitation syndromes. Prog Cardiovasc Dis 1978; 20:285-327
COPYRIGHT 1990 American College of Chest Physicians
COPYRIGHT 2004 Gale Group