Objectives: The normal expression of [Ca.sup.2+]-handling protein is critical for efficient myocardial function. The present study was designed to test the hypothesis that [beta]-blocker treatment may attenuate left ventricular (LV) remodeling and cardiac contractile dysfunction in the failing heart, which may be associated with alterations of [Ca.sup.2+]-handling protein
Methods: We investigated the change of LV remodeling and function in a rat model of heart failure due to myocardial infarction (MI) with or without carvedilol (30 mg/kg/d) or metoprolol (60 mg/kg/d) treatment for 6 weeks (n = 9 in the MI plus carvedilol group, and n = 8 in every other group). The expression of messenger RNA and proteins of sareoplasmic reticulum [Ca.sup.2+]-adenosine triphosphatase (SERCA) and phospholamban in cardiomyocytes of all rats were also measured
Results: There was significant LV remodeling and cardiac contractile dysfunction in MI rats. The messenger RNA and protein expression of SERCA were down-regulated (p < 0.01), but the expression of phospholamban messenger RNA and protein were up-regulated (p < 0.01) in MI rats compared to sham-operated rats. After the treatment with [beta]-blockers, LV remodeling and function were clearly improved. Carvedilol was better in attenuating the weight of the LV and the relative weight of the right ventricle than metoprolol (p < 0.05). [beta]-Blockers restored the low expression of SERCA (p < 0.05) but showed no effect on phospholamban expression (p > 0.05). Moreover, carvedilol induced a more significant improvement of SERCA expression than metoprolol (p < 0.05)
Conclusions: [beta]-Blockers are effective in preventing LV remodeling and cardiac contractile dysfunction in the failing heart. The molecular mechanism may be related to normalization of SERCA expression.
Key words: [Ca.sup.2+]-adenosine triphosphatase; carvedilol; heart failure; metoprolol; phospholamban; sarcoplasmic reticulum
Abbreviations: A wave = late filling velocity; [+ or -] dp/dt = rate of rise and fall; + dp/dtmax = maximum rate of rise; - dp/dtnmx = maximum rate of fall; E wave = early filling velocity; E/A ratio = ratio of early filling velocity to late filling velocity; HR, = heart, rate; FS = fractional shortening; GAPDH = glyceraldehyde phosphated dehydrogenase; v =left ventricle/ventricular; LVAW = left ventricular actual weight; LVAWd = anterior wall thickness at diastolic phase; LVEDP = left ventricular end-diastolic pressure; LVIDd = left ventricular internal diameter at diastolic phase: LVIDs = left ventricular internal diameter at systolic phase; LVPWd = posterior wall thickness at diastolic phase; LVRW = left ventricular relative weight; LVSP = left ventricular systolic pressure; MI = myocardial infarction; PCR = polymerase chain reaction; RT = reverse transcriptase; RV = right ventriele/ventrieular. RVAW = right ventricular actual weight; RVRW = right ventricular relative weight; SERCA = sarcoplasmic reticullum [Ca.sup.2+]-adenosine triphosphatase; SR = sarcoplasmic reticulum
**********
Heart failure is characterized by progressive myocardial remodeling and deteriorating cardiac function. (1) The cellular and molecular changes contributing to the global and/or regional contractile dysfunction of the remodeled myoeardimn are poorly understood. Intracellular [Ca.sup.2+] homeostasis is critical for efficient myocardial function. (2) Sarcoplasmic reticulum [Ca.sup.2+]-adenosine triphosphatase (SERCA) and SERCA regulatory protein phospholamban are the major proteins responsible for intracellular [Ca.sup.2+] homeostasis throughout excitation-contraction cycling in cardiomyocytes. Changes in the abundance and/or function of these molecules in heart failure have been variable in previous studies. In this regard, SERCA messenger RNA and protein abundance have been reported to be smaller in failing vs nonfailing human ventrieular muscle in some studies, (3,4) whereas others (5) showed no significant differences. The levels of phospholamban were also different in heart failure patients; some found phospholamban was higher, and some found it was normal or even lower. (5-7)
In patients with chronic heart failure, treatment with [beta]-adrenergic receptor antagonists led to a reduction in mortality and an improvement of left ventricular (LV) function. (8-10) The major mechanism by which [beta]-adrenergic receptor blockers exert their beneficial effects is blocking the excessively activized sympathetic nervous system. More importantly, it is possible that [beta]-adrenergic receptor blockade indirectly normalizes [Ca.sup.2+]-regulatory proteins, resulting in improved intercellular [Ca.sup.2+] cycling and, in turn, reversing cardiac dysfunction. (1,6) A study (2) showed that a [beta]-receptor blocker, propranolol, can restore the reduction of SERCA in a failing heart.
Carvedilol, a third-generation [beta]-blocker, is a unique multiple-action drug with nonselective [beta]-blockade, [[alpha].sub.1]-blockade. Compared with the selective [[beta].sub.1]-blocker metoprolol, it needs to be confirmed which one is better in improvement of LV remodeling and cardiac contractile function in heart failure. (11,12) Furthermore, whether the beneficial effects of [beta]-blocker on cardiac dysfunction is related with the change of contractile protein expression in a failing heart is also uncertain.
We therefore undertook the present study to evaluate the effect of carvedilol on attenuating LV remodeling and cardiac contractile dysfunction in rats with heart failure due to acute myocardial infarction (MI) and to compare its effects with those of metoprolol. In order to investigate the molecular mechanism, we also measured and compared the messenger RNA and expression of SERCA regulatory protein phospholamban in the failing hearts of rats treated with and without different [beta]-blockers.
MATERIALS AND METHODS
Animal Preparation
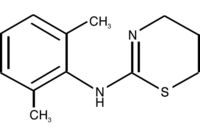
The rat coronary ligation model was employed to induce MI and heart failure. All procedures were approved by the Zhejiang University Animal Care and Use Committee and conformed to the revised 1985 National Institutes of Health guidelines for the care and use of laboratory animals. Adult male Sprague-Dawley rats (weight, 250 to 300 g) were anesthetized with ketamine-HCl (50 mg/kg) and xylazine (5 mg/kg) by intraperitoneal injection. A tracheotomy was performed, and the trachea was intubated with a cannula connected to a rodent ventilator (model CIV-101, Zhejiang University Technologies, Inc; Hangzhon, Zhejian, China). Alter the heart was externalized via an incision between the fourth and fifth intercostal spaces, the proximal left coronary artery was permanently ligated 1 to 2 mm from its origin with a 7-0 silk suture. The heart was immediately internalized, and the chest was dosed. The wound in the trachea due to tracheotomy was closed after the operation. Approximately 50% of the rats survived the procedure. For sham-operated animals, the suture was placed but not ligated. One day after ligation, the animals were assigned to MI group (n = 8), MI plus metoprolol treatment group (donated by ASTRA Pharmaceutical Company, administered by direct gastric lavage at 60 mg/kg/d after the drug dissolved in water for 6 weeks, n = 8) and MI plus carvedilol treatment group (donated by Roche Pharmaceutical Company, administered by direct gastric lavage at 30 mg/kg/d after the drug dissolved in water for 6 weeks, n = 9). Normal control (n = 8) and sham-operated rats (n = 8) were randomly selected before MI.
Echocardiography
Rats were evaluated 2 weeks, 4 weeks, and 6 weeks after coronary artery ligation. Ketamine-HCl (25 mg/kg) was used to induce a semiconscious state. Short- and long-axis images were acquired with an 8-MHz sector-array probe (SONOS 5500; AgilentAqilent Technologies; Palo Alto, CA). Two-dimensional images were obtained at midpapillary and apical levels. LV internal diameter at diastolic phase (LVIDd), LV internal diameter at systolic phase (LVIDs), anterior wall thickness at diastolic phase (LVAWd), and posterior wall thickness at diastolic phase (LVPWd) were measured. LV percentage of fractional shortening (FS) was calculated according to the modified Simpson method: FS (%) = [(LVIDd - LVIDs)/LVIDd] x 100. Peak early filling velocity (E wave) and late filling velocity (A wave) were recorded by pulse-wave Doppler spectra from the apical four-chamber view, and the ratio of the E wave to A wave (E/A ratio) was then calculated. All measurements were averaged for three consecutive cardiac cycles and were made by an experienced technician who was blinded to the group identity.
Hemodynamic Measurement
Six weeks after the initiation of therapy, hemodynamic studies were performed in each group using the methods described by Pfeffer et al. (13) Each rat was weighed and then anesthetized by ketamine-HCl (50 mg/kg) and xylazine (5 mg/kg) by intraperitoneal injection. The right carotid artery was separated and cannulated with a 20-gauge sheathed needle. The needle was extracted, and the end of the sheath was connected to the energy exchanger of an eight-channel physiologic recorder via a heparin/saline solution-filled plastic tube. After balancing with the air pressure, the ascending aortic systolic BP, diastolic BP, and mean BP were recorded. Subsequently, the sheath was reversed into the LV, and the LV systolic pressure (LVSP), LV end-diastolic pressure (LVEDP) and the maximal rate of rise and fall ([+ or -] dp/dt) were recorded. The heart rate (HR) was also recorded synchronously.
Weighing of the Heart and Infarct Size Measurement
After the hemodynamic studies, the heart was arrested in diastole by IV injection of 2 to 3 mL of 10% KCl through the femoral vein. The thorax was rapidly opened, and the heart was excised. The ventricles were separated by incising the right ventricle (RV) along the septum, and each was weighed by an electronic balance. When the LV actual weight (LVAW) and RV actual weight (RVAW) were corrected by body weight, LV relative weight (LVRW) and RV relative weight (RVRW) were calculated.
The tissue was cut in a 5-ram-thick cross-section at the level of the papillary muscle, fixed in 10% formalin, and then dehydrated and embedded in paraffin. One 5-[micro]m section was obtained from this slice and stained with hematoxylin-eosin. The outer infarction length and the outer and inner LV circumferences were measured with a planimeter digital image analyzer (Model MVC-FD71; Sony Corporation, Shinagawa-Ku, Tokyo, Japan). The myocardial infarct size of each section was calculated as the ratio of the outer infarction length to the outer LV circumference and the inner infarction length to the inner LV circumference (perimeter method). Animals with an infarct < 20% or > 45% were not included in the present study.
Western Blotting
Total proteins were isolated from LV myocardium, and concentration was determined by the Lowry method. First, 20 [micro]g of protein was separated on 10% sodium dodecylsulfate-polyacrylamide gel, electrophoresed, and transferred onto nitrocellulose membranes. The blots were blocked with phosphate-buffered saline solution containing 5% dry milk and 0.05% Tween-20 and probed with either anti-rat SERCA antibody (1/1,000 dilution; Affinity BioReagents; Golden, CO) or anti-rat phospholamban antibody (1/1,000 dilution; Affinity BioReagents), for 12 h at 4[degrees]C. Subsequently, blots were incubated with horseradish peroxidase-conjugated sheep anti-rat antibodies (1/500 dilution; Affinity BioReagents) for 1 h at 37[degrees]C. SERCA protein was detected as a 110-kD band and phospholamban protein as a 25-kD band. Blots were semiquantified using imaging software (Kodak Digital Science 1D 2.0 imaging software; Scientific Imaging System, Eastman Kodak, New Haven, CT) and corrected by comparison of actin (43 kD).
Reverse Transcription and Polymerase Chain Reaction
Total cellular RNA was isolated using TRIZOL reagent (Life Technologies). For reverse transcription, each sample containing 10 [micro]g of total RNA, 50 mmol/L of Tris-HCl, pH 8.3, 75 mmol/L of KCl, 0.5 mmol/L of MgCL, 10 mmol/L of dithiothreitol, 0.5 nmol/L each deoxynucleoside triphosphate, 20 U of ribonuclease inhibitor, 100 pmol/L of random hexamer, and 200 U of reverse transcriptase (RT) in a final volume of 33 [micro]L was incubated at 37[degrees]C for 1 h. For polymerase chain reaction (PCR), each sample containing 50 pmol upstream and downstream primers (glyceraldehyde phosphated dehydrogenase [GAPDH]-F38, 5'-GCGCCTGGTCACCAGGGCTGCTT-3' and GAPDH-R502, 5'-TGCCGAAGTGGTCGTGGATGACCT-3', 465 base-pair, gene ID: 493876 (14); SERCA-F2773, 5'-AAGCAGTTCATCCGCTACCT-3' and SERCA-R2906, 5'-AGACCATCCGTCACCAGATT-3', 134 base-pair, gene ID: 2906; PLB-F189, 5'-TACCTTACTCGCTCGGCTATC-3' and PLB-R329, 5'-CAGAAGCATCACAATGATGCAG-3', 141 base-pair, gene ID: 64672 (15)), 200 nmol/L deoxynucleoside triphosphate, 50 mmol/L KCl, 10 mmol/L Tris-HCl, pH 8.3, 10 mmol/L Mg[Cl.sub.2], 2.5 U Taq DNA polymerase in a final volume of 50 [micro]L was amplified for 21 (GAPDH), 26 (SERCA) or 24 (phospholamban) cycles. The amplification profile involved denaturation at 94[degrees]C for 45 s, primer annealing at 52[degrees]C (GAPDH), 55[degrees]C (SERCA) or 53[degrees]C (PLB) for 45 s and primer extension at 74[degrees]C for 45 s. After the last cycle, samples were incubated at 74[degrees]C for 1.5 min to extend incomplete products. The PCR product of GAPDH (5 [micro]L) was mixed with SERCA (5 [micro]L) or phospholamban (5 [micro]L) and then was analyzed on 2% agarose gel and semiquantified using Kodak Digital Science 1D 2.0 imaging software. The PCR product of GAPDH was detected as a 465 base-pair band, SERCA as a 134 base-pair band and phospholamban as a 141 base-pair band according to the marker.
Statistical Analysis
Data are presented as mean [+ or -] SD. Data sets containing multiple groups were analyzed by analysis of variance. Mean values between the two groups were compared by a least-significant difference test, after an F test for homogeneity of variances had been performed. If data failed to meet the requirements for equal variance, a Tamhane T2 test was used. Differences were considered statistically significant at a value of p < 0.05.
RESULTS
Change of Echocardiography
The data of the echocardiographic examinations on all animals at 2 weeks, 4 weeks, and 6 weeks after MI are shown in Table 1. There was a marked increase of LVIDd, LVIDs, LVPWd, E waves, and E/A ratio in the MI group at 2 weeks after coronary ligation. LVAWd, FS, and A waves were significantly decreased in the MI group at 2 weeks. Thereafter, LVIDd, LVIDs, and LVPWd were increased more clearly at 6 weeks. The further decrease of FS was seen at 6 weeks. It indicates that LV dilatation and hypertrophy grew more obvious with the time after MI, and the myocardial pump function was impaired more clearly.
After 6 weeks of treatment with metoprolol or carvedilol, LVIDs and LVIDd were decreased as compared to the MI group, and FS was increased. LVPWd was also decreased in metoprolol- or carvedilol-treated groups at 6 weeks, but LVAWd was unchanged. E and A waves and E/A ratio were renewed partly at 4 weeks after [beta]-blocker treatment. There was no difference between metoprolol and carvedilol in these parameters. Figure 1 showed the representative two-dimensional, short-axis echocardiographic images in hearts of each group at 6 weeks after the beginning of the experiment. The data show that metoprolol and carvedilol improved the LV remodeling and cardiac function after MI.
[FIGURE 1 OMITTED]
Effect of [beta]-Blocker on Hemodynamics
The data given in Table 2 reveal that LVEDP was significantly increased (p < 0.01), and systolic BP, LVSP, maximum rate of rise (+ dp/dtmax), and maximum rate of fall (- dp/dtmax) were significantly decreased (p < 0.01), and HR was unchanged (p > 0.05) in the MI group compared with the sham-operated group. In comparison with the MI group, HR was significantly decreased in all therapy groups (p < 0.01), and the effect on HR in the carvedilol group was equivalent to that in the metoprolol group (p > 0.05); LVEDP was significantly decreased in all therapy groups (p < 0.01); + dp/dtmax and - dp/dtmax were increased in both the metoprolol and carvedilol treatment groups (p < 0.05). There was no difference on LVEDP, + dp/dtmax, and - dp/dtmax between two drugs therapy groups. The results confirm the effects of metoprolol and carvedilol on improving the cardiac function after MI.
Effect of [beta]-Blocker on Heart Weight and Infarction Size
As the data are shown in Table 3, LVAW, LVRW, RVAW, and RVRW were significantly increased in the MI group (p < 0.01). In comparison with the MI group, LVAW, LVRW, RVAW, and RVRW were all significantly decreased in the metoprolol or carvedilol treatment groups (p < 0.01). Moreover, LVAW and LVRW decreased more clearly in the carvedilol treatment group relative to the metoprolol treatment group (p < 0.05). This points out that metoprolol and carvedilol partially restored the hypertrophy of the heart after MI and carvedilol was better than metoprolol in restoring the hypetrophy of the heart after MI.
There is no difference in infarction size among the MI group, the metoprolol treatment group, and the cavedilol treatment group (p > 0.05). Figure 2 shows the cardiac gross morphology stained with hematoxylin-eosin in different groups.
[FIGURE 2 OMITTED]
Effect of [beta]-Blocker on SERCA and Phospholamban Messenger RNA Expression
The level of SERCA messenger RNA (Fig 3, top, A) in the myocytes was down-regulated clearly after MI (p < 0.01). However, the levels of phospholamban messenger RNA (Fig 3, bottom, B) were elevated significantly in the MI group (p < 0.01). Metoprolol and carvedilol markedly restored the MI-induced decrease in the SERCA gene expression (p < 0.05). Moreover, carvedilol was stronger than metoprolol in improving the expression of SERCA messenger RNA after MI (p < 0.05). Metoprolol and carvedilol did not prevent the elevated expression of phospholamban messenger RNA after MI (p > 0.05).
[FIGURE 3 OMITTED]
Effect of [beta]-Blocker on SERCA and Phospholamban Protein Expression
LV myocyte protein expression of SERCA (Fig 4, top, A) and phospholamban (Fig 4, bottom, B) were also examined. SERCA protein expression was also decreased and phospholamban protein expression was increased in the MI rats (p < 0.01). After treatment with metoprolol or carvedilol for 6 weeks, SERCA protein expression was elevated (p < 0.05), but no significant difference in phospholamban protein levels were observed in treated rats compared with nontreated rats (p > 0.05). Carvedilol restored the expression of SERCA protein more clearly compared to metoprolol (p < 0.05).
[FIGURE 4 OMITTED]
DISCUSSION
It has been elucidated that excessive activation of the sympathetic nervous system is one of the major responses and plays a key role in LV remodeling initiation and progression after acute MI. (16) Therefore, the administration of a [beta]-blocker should have beneficial effects on postinfarction LV remodeling. Carvedilol significantly reduced myocardial collagen deposition in the noninfarcted myocardium and cardiac hypertrophy in the LV, whereas metoprolol had no effect on myocardial hypertrophy. (13) Another study (12) showed that metoprolol also prevented hypertrophy due to MI. The present study revealed that carvedilol and metoprolol were all effective in preventing LV dilatation and hypertrophy, and carvedilol was better in attenuating postinfarction LV remodeling with respect to hypertrophy (LVAW and LVRW) than metoprolol. As we know, carvedilol at 50 to 100 mg/d produced reductions in exercise HR that were similar to metoprolol at 125 to 150 mg/d, (17) indicating comparable degrees of [beta]-blockade. Therefore, carvedilol (30 mg/kg/d) is similar as metoprolol (60 mg/kg/d) on degrees of [beta]-blockade. It means, although [beta]-adrenergic receptor was blocked similarly by metoprolol and carvedilol, the effect on LV remodeling was different. So, the underlying mechanism for better prevention of hypertrophy by carvedilol is probably multifactorial, including the vasodilation effect of LV preload and afterload reduction with [[alpha].sub.1]-blockade and antioxidant effects against catecholamines in myocardium. (18-19)
The beneficial effects of chronic [beta]-adrenergic receptor blockade on myocardial pump function are well documented. (1,6,10,20) Our study on hemodynamics demonstrates that LVEDP was significantly increased, and LVSP and [+ or -] dp/dt were decreased clearly after MI; meanwhile, FS in echocardiography was also decreased, indicating that LV function was impaired, which was consistent with another report. (17) Moreover, the elevated LVEDP and decreased LVSP, [+ or -] dp/dt, and FS were significantly renewed after treatment with carvedilol or metoprolol. These results suggest that both carvedilol and metoprolol have beneficial effects on hemodynamics and can improve LV function after MI. Because most of hemodynamic parameters were partially reversed by [beta]-inhibition but not the infarction size, it is hard to conclude that [beta]-blockers have a directly effect on ischemic myocytes of the LV. It might be speculated that [beta]-blocker protects or enhances the function of remaining survival myocytes in the LV during ischemia. The mechanisms for hemodynamic improvement by [beta]-blockade may be due to the reduction of wall stress and oxygen uptake, and an increase in coronary blood flow associated with blockage of excessive sympathetic activation, (21,22) which can protect and enhance the function of remaining survival myocytes in the LV during ischemia. But the more important mechanism may be related to intracellular [Ca.sup.2+] regulation of remaining survival myocytes in the LV. (2,23)
SERCA is responsible for restoring sarcoplasmic reticulum (SR) [Ca.sup.2+] load per excitation-contraction cycle. Decreasing SERCA content is associated with reduced SR [Ca.sup.2+] loading and elevated cytoplasmic [Ca.sup.2+] levels. (24,25) Ito et al (25) showed that stabilizing SERCA levels prevents alterations in SR and cytosolic [Ca.sup.2+] content, attenuating the transition to heart failure in pressure-overloaded mice. Therefore, restoration of SERCA levels is likely to be a critical factor in normalization of [Ca.sup.2+] uptake in the line-scan and frequency-dependent experiments. (2) The activity of SERCA is regulated by its inhibitory protein phospholamban.
Even though a decrease in the SR [Ca.sup.2+] cycling protein levels has been implicated as a factor underlying changes in the contractile function in the failing heart, (3,4) no alterations in the SERCA or phospholamban proteins were observed in heart failure by some investigators. (5) Lennon et al (7) found that phospholamban expression was increased in dilated cardiomyopathy. It is probable that a defect in these regulatory mechanisms may be of significance in the development of cardiac contractile dysfunction and subsequent heart failure.
Our results indicate that the expression of SERCA messenger RNA and protein was significantly depressed in congestive heart failure due to MI. It may be the important mechanism of cardiac contractile dysfunction. In view of these considerations, we sought to examine the expression of phospholamban in normal and failing rat hearts. Our study showed that the expression of phospholamban messenger RNA and protein was up-regulated in the model of heart failure after MI. At the same time, we found that the cardiac contractile function was severely decreased. Therefore, SERCA phospholamban may play an important role on maintaining cardiac function.
The more important finding is that the 6 weeks of treatment of MI rats with [beta]-receptor blockade, metoprolol or carvedilol, improves SERCA messenger RNA and protein levels, which lead to markedly improved cardiac function as assessed by echocardiography and hemodynamics. SERCA current density levels were elevated by [beta]-receptor blockade treatment, at least partially explaining the improved cardiac contractile function in treated rats. These findings are in agreement with another study (2) that report improved SERCA levels after treatment with the [beta]-blockade propranolol in dilated cardiomyopathy. However, our study showed that metoprolol and carvedilol did not restore the overexpression of phospholamban messenger RNA and protein due to MI. Phospholamban is a prominent mediator of the transduction of cardiac [beta]-adrenergic signaling via its phosphorylation by [beta]-adrenergic stimulation. (26) It is now well established that SERCA is inhibited by the unphosphorylated form of phospholamban in the SR membrane. (27) So, [beta]-adrenergic receptor blockers increasing the expression of SERCA may be not related with phospholamban expression.
We can only speculate about a mechanism for normalization of SERCA abundance produced by [beta]-blockers treatment. This mechanism could involve elimination of [beta]-adrenergic receptor-mediated repression of myocyte SERCA expression. [beta]-Blockers also could reduce apoptosis, (28) thereby increasing the number of functional myocytes. Still another possibility is that [beta]-blockers could be working through nonmyocytes to eliminate the expression of factors that depress myocyte function by decreasing SERCA expression. (29)
It is pointed out that, to the best of our knowledge, our study is the first to compare the different effects on SERCA and phospholamban between selective [beta]-blocker, metoprolol, and nonselective [beta]-blocker, carvedilol. It appears that carvedilol was better in enhancing restoration in protein and messenger RNA content of SERCA, but not phospholamban, compared with metoprolol. The molecular mechanisms of the different regulatory effects of metoprolol and carvedilol on SERCA are not clear. It is very likely that the beneficial effects of carvedilol were due to its antioxidant and antiproliferative activity, which could be important in preventing the progressive loss of myocardial cells that is characteristic of a failing heart. (30,31) Thus the specific mechanism remains to be further investigated.
In summary, [beta]-receptor blockade is effective in preventing LV remodeling and cardiac contractile dysfunction in the failing heart after MI. The molecular mechanism may be related with normalization of [Ca.sup.2+]-handling protein content. The nonselective [beta]-receptor blockade, carvedilol may have more cardioprotective effects on heart failure of MI than the selective [beta]-receptor blockade, metoprolol.
Limitations
In comparison with the levels of SERCA and phospholamban, the activities of SERCA and phospholamban are more important parameters to correlate with the improvement of cardiac function. Because of the experimental condition, we only measured the contents of SERCA and phospholamban to prompt the relationship. Moreover, in order to communicate between [beta]-receptor and SERCA, it is better to measure the [beta]-receptor expression and [Ca.sup.2+] mobilization directly in the postischemic myocyte. It should be investigated in later study. Third, we only observed the change of all of the parameters 6 weeks after MI. Although there is a different effect on SERCA expression between carvedilol and metoprolol treatment, no different effect on cardiac contractile function was observed between the two drugs. If we had the data beyond 6 weeks, we might get more information about it.
ACKNOWLEDGMENT: We thank Jian Sun and Chao-Hui Zhu for their expertise with Western blot, RT-PCR, and figure preparation.
REFERENCES
(1) Bristow MR. [beta]-Adrenergic receptor blockade in chronic heart failure. Circulation 2000; 101:558-569
(2) Plank DM, Yatani A, Ritsu H, et al. Calcium dynamics in the failing heart: restoration by [beta]-adrenergic receptor blockade. Am J Physiol Heart Circ Physiol 2003; 285:H305-H315
(3) Meyer M, Schillinger W, Pieske B, et al. Alterations of sarcoplasmic reticulum proteins in failing human dilated cardiomyopathy. Circulation 1995; 92:778-784
(4) Haseufuss G, Reinecke H, Studer R, et al. Relation between myocardial function and expression of sarcoplasmic reticulum Ca(2+)-ATPase in failing and nonfailing human myocardium. Circ Res 1994; 75:434-442
(5) Schwinger RH, Bohm M, Schmidt U, et al. Unchanged protein levels of SERCA II and phospholamban but reduced Ca2+ uptake and Ca(2+)-ATPase activity of cardiac sarcoplasmic reticulum from dilated cardiomyopathy patients compared with patients with nonfailing hearts. Circulation 1995; 92:3220-3228
(6) Kubo H, Margulies KB, Piacentino V 3rd, et al. Patients with end-stage congestive heart failure treated with beta-adrenergic receptor antagonists have improved ventricular myocyte calcium regulatory protein abundance. Circulation 2001; 104: 1012-1018
(7) Lennon NJ, O'Reilly C, Ohlendieck K. Impaired Ca2+-ATPase oligomerization and increased phospholamban expression in dilated cardiomyopathy. Int J Mol Med 2000; 6:533-538
(8) Waagstein F, Bristow MR, Swedberg K, et al. Beneficial effects of metoprolol in idiopathic dilated cardiomyopathy. Metoprolol in Dilated Cardiomyopathy (MDC) Trial Study Group. Lancet 1993; 342:1441-1446
(9) A randomized trial of [beta]-blockade in heart failure: the Cardiac Insufficiency Bisoprolol Study (CIBIS). CIBIS Investigators and Committees. Circulation 1994; 90:1765-1773
(10) Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. U.S. Carvedilol Heart Failure Study Group. N Engl J Med 1996; 334:1349-1355
(11) Wei S, Chow LT, Sanderson JE. Effect of carvedilol in comparison with metoprolol on myocardial collagen postinfarction. J Am Coll Cardiol 2000; 36:276-281
(12) Masson S, Masseroli M, Fiordaliso F, et al. Effects of a DA2/[alpha]2 agonist and a [beta]1-blocker in combination with an ACE inhibitor on adrenergic activity and left ventricular remodeling in an experimental model of left ventricular dysfunction after coronary artery occlusion. J Cardiovasc Pharmacol 1999; 34:321-326
(13) Pfeffer JM, Finn PV, Zornoff LA, et al. Endothelin-A receptor antagonism during acute myocardial infarction in rats. Cardiovasc Drugs Ther 2000; 14:579-587
(14) Fruebis J, Gonzalez V, Silvestre M, et al. Effect of probucol treatment on gene expression of VCAM-1, MCP-1, and M-CSF in the aortic wall of LDL receptor-deficient rabbits during early atherogenesis. Arterioscler Thromb Vasc Biol 1997; 17:1289-1302
(15) Mirit E, Palmon A, Hasin Y, et al. Heat acclimation induces changes in cardiac mechanical performance: the role of thyroid hormone. Am J Physiol 1999; 276:R550-R558
(16) Metra M, Nodari S, D'Aloia A et al. A rationale for the use of [beta]-blockers as standard treatment for heart failure. Am Heart J 2000; 139:511-521
(17) Litwin SE, Katz SE, Morgan JP, et al. Long-term captopril treatment improves diastolic filling more than systolic performance in rats with large myocardial infarction. J Am Coll Cardiol 1996; 28:773-781
(18) Senior R, Basu S, Kinsey C, et al. Carvedilol prevents remodeling in patients with left ventricular dysfunction after acute myocardial infarction. Am Heart J 1999; 137:646-652
(19) Capomolla S, Febo O, Gnemmi M, et al. [beta]-Blockade therapy in chronic heart failure: diastolic function and mitral regurgitation improvement by carvedilol. Am Heart J 2000; 139: 596-608
(20) Aoyagi T, Yonekura K, Eto Y, et al. The sarcoplasmic reticulum Ca2+-ATPase (SERCA2) gene promoter activity is decreased in response to severe left ventricular pressure-overload hypertrophy in rat hearts. J Mol Cell Cardiol 1999; 31:919-926
(21) Zanchetti A, Stella A. Neural control of renin release. Clin Sci Mol Med Suppl 1975; 2:215s-223s
(22) Eichhorn EJ, Heesch CM, Risser RC, et al. Predictors of systolic and diastolic improvement in patients with dilated cardiomyopathy treated with metoprolol. J Am Coll Cardiol 1995; 25:154-162
(23) Flesch M, Maack C, Cremers B, et al. Effect of beta-blockers on free radical-induced cardiac contractile dysfunction. Circulation 1999; 100:346-353
(24) Schmidt U, del Monte F, Miyamoto MI, et al. Restoration of diastolic function in senescent rat hearts through adenoviral gene transfer of sarcoplasmic reticulum Ca(2+)-ATPase. Circulation 2000; 101:790-796
(25) Ito K, Yah X, Feng X, et al. Transgenic expression of sarcoplasmic reticulum Ca(2+) atpase modifies the transition from hypertrophy to early heart failure. Circ Res 2001; 89:422-449
(26) Stein B, Bartel S, Kokott S, et al. Effects of isoprenaline on force of contraction, cAMP content, and phosphorylation of regulatory proteins in hearts from chronic beta-adrenergic-stimulated rats. Ann N Y Acad Sci 1995; 752:230-233
(27) Netticadan T, Temsah RM, Kawahata K, et al. Sarcoplasmic reticulum Ca(2+)/Calmodulin-dependent protein kinase is altered in heart failure. Circ Res 2000; 86:596-605
(28) Zaugg M, Xu W, Lucchinetti E, et al. [beta]-Adrenergic receptor subtypes differentially affect apoptosis in adult rat ventricular myocytes. Circulation 2000; 102:344-350
(29) Kubo H, Margulies KB, Piacentino V 3rd, et al. Patients with end-stage congestive heart failure treated with [beta]-adrenergic receptor antagonists have improved ventricular myocyte calcium regulatory protein abundance. Circulation 2001; 104: 1012-1018
(30) Bristow MR, Gilbert EM, Abraham WT, et al. Carvedilol produces dose-related improvements in left ventricular function and survival in subjects with chronic heart failure. MOCHA Investigators. Circulation 1996; 94:2807-2816
(31) Watanabe K, Ohta Y, Nakazawa M, et al. Low dose carvedilol inhibits progression of heart failure in rats with dilated cardiomyopathy. Br J Pharmacol 2000; 130:1489-1495
* From the Departments of Respiratory Sciences (Drs. Y-L Sun and J-Y Zhou), and Cardiovascular Sciences (Drs. S-J Hu, L-H Wang, and Y Hu), The First Affiliated Hospital, College of Medicine, Zhejiang University Hangzhou Zhejiang China. This study was supported by a Grant for Scientific Research from Zhejiang Province of China (021107817) and in part by E-Institutes of Shanghai Municipal Education Commission (E-04010).
Manuscript received December 7, 2004; revision accepted February 23, 2005.
Reproduction of this article is prohibited withont written pennission from the Ameriema College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml).
Correspondence to: Shen-Jiang Hu, MD, PhD, Department of Cardiovascular Sciences, The First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, Zhejiang, 310003, China; e-mail: s0hu0001@hotmail.com
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group